1. Background
Animal-assisted therapy, most frequently used with dogs, is being used increasingly as an adjunctive alternative treatment for psychiatric patients. One of the commonly used methods includes activities with horses which are incorporated into comprehensive rehabilitation therapy sessions aimed at restoring lost function, alleviate, minimize or eliminate physical, psychological, social or mental disability of the patient or client (1). Hippotherapy is also used in psychiatric care where it is found in world literature under the name of therapeutic horse riding and psychotherapeutic horse riding (2).
Although a recent review questions the benefits of hippotherapy in mental illness (3), some reports indicate that hippotherapy has a positive effect on patients with mental illnesses and mental disorders. Interaction with horses had a positive impact on the alleviation of aggression and improved interpersonal interaction both during hospitalization of patients with recent in-hospital violent behavior or highly regressed behavior enrolled in this study and few months after release to home care (4). Another study, including patients with schizophrenia, described positive trends in patients’ self-esteem, self-confidence and social functioning (5). In addition, Cerino et al. (6) reported that a one- year treatment involving therapeutic riding sessions improved negative symptoms, caused disease remission and reduced rate of hospitalization of subjects with schizophrenia.
2. Objectives
In this study, we investigated effects of hippotherapy in the treatment of schizophrenia. We were not satisfied only with the observation of patients in the actual therapy, but we wanted to determine immediate subjective feelings of patients at the beginning and the end of the therapeutic unit, and at the end of the therapeutic process. Our main outcome was well-being, defined as excellent mood, the feeling of total relaxation, no sense of fear, a willingness to establish contacts, and inclination to communicate.
3. Methods
In this study, we included a convenience sample of all patients who underwent hippotherapy. It consisted of 16 patients (three women and 13 men) with paranoid schizophrenia, and 9 patients (4 women and 5 men) with acute and transient psychotic disorders. Participating patients were in the age range from 20 to 57 years with no previous experience with horses. At the time of participation Hippotherapy, the patients were hospitalized in a psychiatric hospital and therapeutic classes were indicated by their physician after the acute phase of their mental illness. In the acute phase of mental illness, hippotherapy is contraindicated and practically impossible, because it is associated with a high risk of unpredictable behavior of the patient (7).
Patients attended hippotherapy on a regular basis two days a week for a period of three weeks. The therapeutic unit lasted 90 minutes and took the form of group therapy. Each therapeutic unit was led by health care professionals and had always been very well prepared in advance (depending on the patient’s individual plans and set targets). The study was approved by the ethical commission, hospital of Havlíckuv Brod, Czech Republic.
3.1. Procedure
Hippotherapy in psychiatry is not concerned only about the patient sitting on a horse and the horseback movement influencing the physical condition of the patient, his functional and postural disorders. We are concerned with positive effects on the mental state of a patient and use mainly contact with the horse, work with the horse from the ground and to a lesser extent, riding on horseback in a saddle or with handles. We put emphasis on enjoyment and processing, social communication and focus on the development of cognitive and executive functions. Therapeutic units are organized as a group therapy with each group having 6 patients. Each unit is started by a group session and ended by reflection of the whole group in a therapy room. During the therapeutic activity, the patients work with a horse in two groups of three and have the same horse throughout the whole hippotherapy treatment.
During those six therapeutic units, patients initially get familiar with the environment of stables with horses and make first contact with a health care worker. In the next lesson, we use therapeutic technique for cleaning horses and general care of the horses. Among the key therapeutic activities is work with the horse from the ground and work with nonverbal communication. This may produce a large amount of valuable therapeutic material, which under the supervision of experienced medical staff may be worked out, consciously adopted and used in the personal life of the patient. During the interaction of the patient with the horse, we can monitor: activity vs. passivity, submissiveness vs. dominance, certainty vs. uncertainty, aggression vs. affiliation, working with space, time and boundaries, stance and posture, work with pressure and relaxation.
In the work with horse from the ground we start from the observed social behavior of horses in the herd. We are talking about interspecies communication between horse and man, where man learns horse’s body language, especially with non-verbal communication. There is an effort to create a natural partnership between the horse and the man, this can only be achieved with mutual trust. It requires mindfulness training and good knowledge of hippology by humans (8).
Other therapeutic activity in hippotherapy includes horse riding. We include this activity only after the patient knows his horse well, thus increasing the therapeutic effect and minimizing patient’s and horse’s discomfort. Some patients are from the beginning scared of the horse and others do not respect the horse, without required empathy. Opportunity to learn his horse and establish a relationship with him results in needed self-confidence, respect, and relaxation for the patient.
We defined well-being as a state that has five characteristics - excellent mood, the feeling of total relaxation, no sense of fear, a willingness to establish contacts, and inclination to communicate. Patients assessed their current well-being by completing a form where each of these five characteristics had a value from zero to ten. The best well-being was present with the score 10 for mood, contact and communication, and with the score 0 for tension and fear. For the analysis of the scores, tension and fear were reversed scored so that the total scores could range from 0 to 50. This scale had very good reliability with Cochran alpha from 0.73 to 0.83 for different treatments. Patients were asked to fill out a form before starting treatment and after its completion.
3.2. Statistical Analysis
For this study, we analyzed the state of well-being before and after six hippotherapy treatments. The overall effect was analyzed by general linear modeling (GLM) with repeated values. We Also compared the scores for each application by ANOVA and the changes of individual characteristics by the paired t-test. To control for multiple comparisons, we considered significant difference only for P < 0.01. For these analyses we divided patients into two groups: 1, patients with diagnosis of paranoid and undifferentiated schizophrenia and; 2, patients with other diagnoses including acute polymorphic psychotic disorder with symptoms of schizophrenia, acute psychotic disorder with a prevalence of schizoaffective disorder and delusions.
4. Results
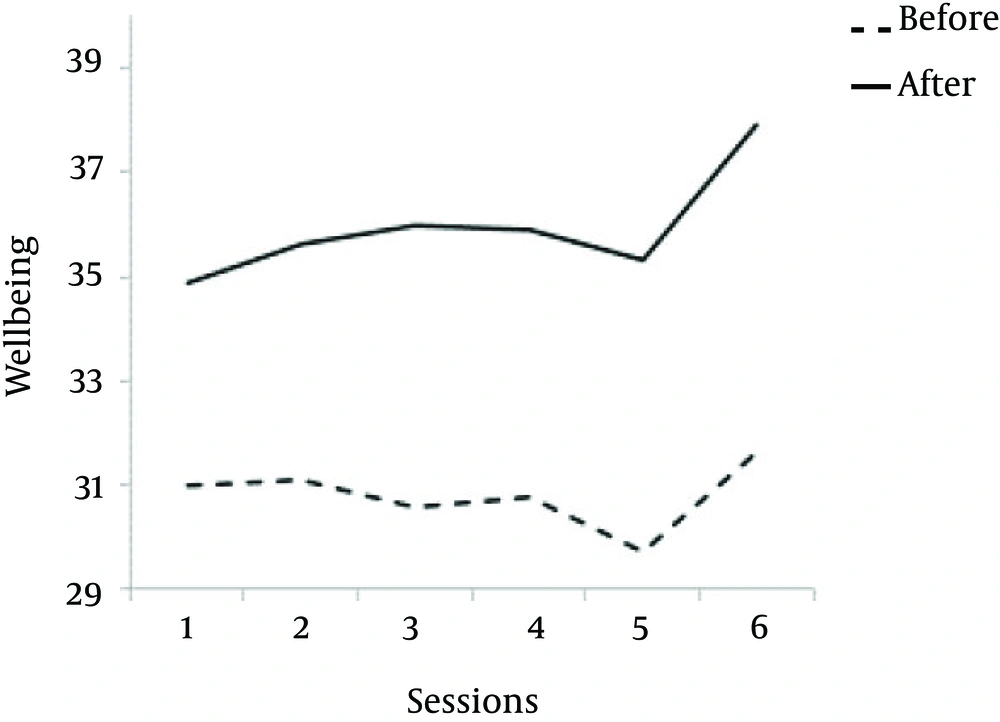
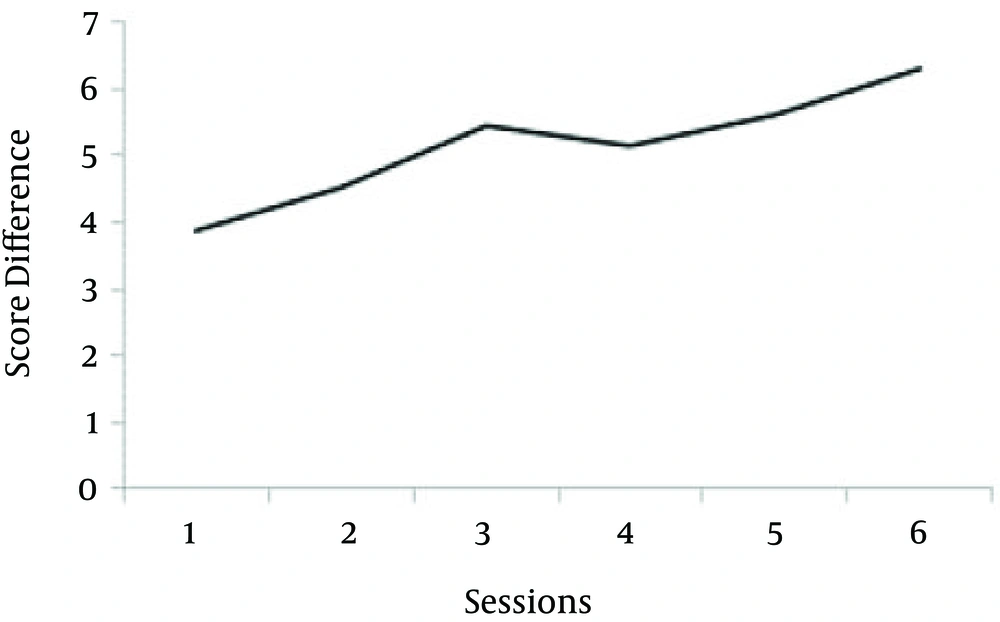
Hippotherapy increased well-being when all treatments were combined (F = 7.81, P = 0.007) (Figure 1), and sex and diagnosis had no significant effects (F = 0.49, P = 0.49 and P = 2.07, P = 0.162). The scores of well-being did not differ according to treatment numbers but the differences between the well-being scores before and after the treatments increased with treatment repetitions. This difference had a positive slope (F = 32.83, P = 0.005) (Figure 2). This increasing effect of hippotherapy treatments was also evident from the increasing statistical significance when individual treatments were compared (Treatment 1, P = 0.081; Treatment 2, P = 0.036; Treatment 3, P = 0.005; Treatment 4, P = 0.014; Treatment 5, P = 0.012, and Treatment 6, P = 0.006).
Analysis of individual parts of the well-being scale showed that the overall effect was statistically significant for mood and tension, almost significant for fear and insignificant for contact and communication (Table 1). Gender had no effect but the diagnosis effect was significant for contact, where a willingness to contact was higher in schizophrenic patients than in patients with other diagnoses before and after hippotherapy. Paired t-tests corrected for multiple comparisons showed that the effect hippotherapy was statistically significant for all treatments regarding mood and fear and for other items with the exception of tension, contact and communication in the first treatment and contact in the second treatment (Table 2).
| Parameter | Intervention | Diagnosisa | Gender | |||
|---|---|---|---|---|---|---|
| F | P | F | P | F | P | |
| Mood | 21.37 | < 0.001 | 0.446 | 0.510 | 0.966 | 0.334 |
| Tension | 4.84 | 0.032 | 1.20 | 0.283 | 1.34 | 0.258 |
| Fear | 3.96 | 0.051 | 0.028 | 0.868 | 1.43 | 0.242 |
| Contact | 1.88 | 0.175 | 4.24 | 0.049 | 0.012 | 0.914 |
| Communication | 3.29 | 0.075 | 2.92 | 0.099 | 0.007 | 0.935 |
aComparison of persons with paranoid and undifferentiated schizophrenia, and persons with acute and temporary psychotic disturbances and schizoaffective diagnosis.
| Parameter | Session Number | |||||
|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | |
| Mood | 5.37 vs. 6.70 | 5.93 vs. 7.43 | 5.67 vs. 7.27 | 5.90 vs. 7.20 | 5.47 vs. 7.10 | 5.73 vs. 7.53 |
| t | -7.61 | -7.64 | -6.87 | -6.36 | -5.56 | -7.31 |
| P | < 0.001 | < 0.001 | < 0.001 | < 0.001 | < 0.001 | < 0.001 |
| Tension | 3.63 vs. 3.17 | 3.80 vs. 2.80 | 3.27 vs. 2.37 | 3.67 vs. 2.43 | 3.37 vs. 2.47 | 3.27 vs. 1.97 |
| t | 1.65 | 3.83 | 3.59 | 5.18 | 2.88 | 3.99 |
| P | 0.109 | 0.002 | 0.001 | < 0.001 | 0.007 | < 0.001 |
| Fear | 2.50 vs. 1.93 | 2.90 vs. 1.90 | 2.47 vs. 1.53 | 2.87 vs. 1.80 | 3.00 vs. 1.97 | 2.60 vs. 1.53 |
| t | 2.89 | 4.66 | 3.50 | 3.32 | 2.95 | 3.99 |
| P | 0.007 | < 0.001 | 0.002 | 0.002 | 0.006 | < 0.001 |
| Contact | 6.20 vs. 6.63 | 6.00 vs. 6.47 | 5.47 vs. 6.33 | 5.97 vs. 6.53 | 5.40 vs. 6.30 | 6.00 vs. 6.93 |
| t | -2.15 | -1.76 | -3.50 | -4.57 | -5.57 | -3.29 |
| P | 0.040 | 0.090 | 0.002 | > 0.001 | < 0.001 | 0.003 |
| Communication | 5.57 vs. 6.63 | 5.87 vs. 6.60 | 5.17 vs. 6.27 | 5.43 vs. 6.40 | 5.27 vs. 6.37 | 5.77 vs. 6.97 |
| t | -2.66 | -3.06 | -3.37 | -4.82 | -3.44 | -4.09 |
| P | 0.013 | 0.005 | 0.002 | < 0.001 | 0.002 | < 0.001 |
5. Discussion
The purpose of this study was to investigate the effect of hippotherapy sessions on mental well-being of patients with paranoid schizophrenia and patients with acute and transient psychotic disorders who were hospitalized in a psychiatric hospital. We have found that hippotherapy significantly increased well-being of these patients and that the effect was increasing with repeated sessions.
We selected five characteristics of well-being based on our 14-year experience of treating patients with schizophrenia. We focused especially on certain features of emotion (mood, fear, psychic tension) and of social areas (contacts, communication). The patients spoke most often about these subjective feelings during hippotherapy. We also considered that schizophrenia is characterized by disturbed thinking, perception and personality. Schizophrenia results in deficit in patient’s ability to understand world, behave rationally, and act and succeed in life (9).
Most common experience that patients with schizophrenia during hippotherapy mention was mood, which the disease changed towards depressive and anxious states. In our experience, it is optimal if hippotherapy occurs in natural surroundings and in a safe group without white coats. The therapy takes into account individual needs of participants and from the beginning tries to motivate every patient. It is very important that every patient has a positive experience that he later interprets and shares with others. Very important is, if he speaks about enjoying it.
The patient is more open to communication and feelings because of the experience with a horse, the therapist and the group. The horse can focus his interest and distract him from his problems. The horse considers the patient as an equal partner and allows him to recognize and experience his identity. Experience in a stable and with a horse leads to increased emotions of the patient that is reflected in his verbal communication, mentioning improved mood and feeling of release. The release of psychic tension may be related to the improved mood. Patients report that this condition lasts several hours after ending hippotherapy.
Patients with paranoid schizophrenia and psychotic disorder who are provided hippotherapy speak rarely about feeling of fear. That is probably because the disease decreases the ability to read signals from the environment. Therefore, they cannot adjust their actions because they miss a healthy respect. In hippotherapy, we are using the word respect instead of fear. Development of a healthy respect towards the horse is very often related to behavioral limits of the patient. If the patient has tendency to cross his limits, the horse reacts to that sensitively and modify his behavior to one acceptable to the environment. On the other hand, if the patient is withdrawn, the horse activates him by his curiosity and need for contact. According to our experience, the horse obtains respect from the patient naturally, due to its size, neutrality and show of force. The patient almost always responds to non-verbal expression of the horse and later shares the experiences, emotions and feelings with the therapist and the group.
Hippotherapy in psychiatry is always based on individual goals and needs of the patient. Marianne Gang talks about so-called borderline experience where patients have the opportunity during various activities with horses to explore their own possibilities and limits, which allows them a high emotional involvement (10). Work with emotions, feelings and communication is essential to the therapeutic process of hippotherapy in psychiatry. In agreement with some reports (5, 6), we found improvement in negative symptoms of schizophrenia, self-confidence and social functioning.
Our study has several limitations. We did not use a validated evaluation scale but designed one from our clinical experience. However, out scale had very good reliability. We concentrated on evaluation of hippotherapy effect on well-being and did not collect data regarding drug administration and hospital admission. We evaluated effects of only 6 therapeutic units and the relatively short duration of the study may not have an effect on these variables. The patients served as their own controls and we cannot exclude longitudinal changes in disease symptomatology. There is a need for longer study that would evaluate effects of hippotherapy in schizophrenia by a randomized control methodology and collect information about several clinical outcomes.