1. Background
In the field of neurosurgery, patient positioning plays a key role. Seated position is a good position in posterior fossa and cervical spine surgery. There are only a few publications on cerebral perfusion and oxygenation in patients undergoing neurosurgery in seated position, and different discussions could be found about the possible causes of cerebral hypoxia.
Jöbsis first introduced the idea of using near infrared spectroscopy (NIRS) to non-invasively measure cerebral tissue oxygenation in 1977 (1). The principle of NIRS is based on the fact that near-infrared light readily passes through the skin and skull and is absorbed by certain biological molecules in the brain (2).
Significant regional cerebral oxygen saturation (rSO2) desaturation may occur in up to 30% of major non-cardiac surgical procedures in elderly patients (3). Maintenance of rSO2 within 10% to 20% of baseline in these patient groups reduced complications (4, 5). Although the normal rSO2 in a fit young patient may be around 60% to 70%, representing a venous weighted measure of cerebral tissue oxygenation, values as low as 35% are sometimes seen in elderly patients presented for surgery and may be a significant predictor of poor outcome (6). A recent study suggests that rSO2 is a potentially important biomarker that should be measured in heart failure patients and suggests that it may be a useful marker of target organ perfusion (7).
The seated position provides optimum access to posterior fossa and cervical spine, improves venous and cerebral spinal fluid drainage, decreases intracranial pressure, lowers airway pressure, and improves access to the face for signs of cranial nerve stimulations (8). The seated position is thought to be the best for surgical access to the posterior fossa or to dorsally-located parietal lesions. Gravity facilitates drainage of blood and other fluids and an optimal view over the pathology is possible with lowered intracranial pressure and increased venous reflux (9).
However, there are several publications in support and against cerebral perfusion and oxygenation in seated position. Since 1913, when the first surgery with a patient in sitting position was performed, the debate concerning this positioning has continued (10). There are some reports about stroke, loss of vision, and ophthalmoplegia, which are possibly related to hypotension, reduction of blood flow of the vertebral artery due to hyperextension and rotation or tilt of the head, which could decrease cerebral oxygenation resulting in cerebral ischemia (11, 12). However, these reports have not been confirmed by other studies, Lee et al. showed that unlike the pattern of MAP values, there was no additional decrease in rSO2 in seated position during anesthesia (13).
There are also reports that indicate improvements in respiratory mechanics and pulmonary gas exchange after the seated position (14, 15).
The goal of this study was to investigate the effects of the seated position on cerebral oxygenation in patients undergoing surgeries on posterior fossa. In detail, cerebral oxygenation changes in patients before anesthesia induction until the end of surgery in seated position were measured.
2. Methods
In this prospective study, from May 2013 to February 2015, after obtaining informed consent from the participants, the researchers included 95 consecutive patients with American Society of Anesthesiology (ASA) class I-III aged between 18 and 80 years, who were candidates for elective craniotomies in seated position. Ischemic cerebrovascular disease, known patent foramen ovale, severe uncontrolled hypertension, methemoglobinemia or any intra vascular dye injection during the operation was considered as the exclusion criteria.
After hospital admission, an anesthesiologist examined all the patients, and plan of anesthesia and risks and benefits of operation in seated position were described to the participants. Preoperative data, including age, gender, ASA physical status, height, weight, co-morbidities, medications, and routine laboratory analysis were also collected.
On the day of surgery before entering the induction room, patients received Midazolam (5 mg) orally as a premedication. Pre-anesthetic monitoring included non-invasive blood pressure, Electrocardiogram (ECG), heart rate, and Peripheral Oxygen Saturation (SpO2). Two cerebral oximeter sensors (Invos 5100 Somanetics, Troy, MI) were placed bilaterally, two centimeters above the eyebrows on the forehead, and while breathing from room air, baseline rSO2 was recorded.
After pre-oxygenation, anesthesia was induced using propofol 2 mg/Kg and sufentanil (0.2 - 0.3 µg/kg), then rocuronium (0.6 - 0.8 mg/Kg) was given for neuromuscular blockade. Tracheal intubation was performed with an armored tracheal tube and then oxygen concentration and fresh gas flow were adjusted to keep FiO2 in the range of 40% to 50%, and minute ventilation was set to maintain EtCO2 in the range of 30 to 35 mm-Hg and a PEEP of about 5 cm-H2O.
After induction of anesthesia, a radial artery cannula was inserted for continuous blood pressure monitoring and blood sampling for arterial blood gas analyses and after intubation, a central vein catheter was inserted peripherally (Cephalic or Basilic vein) or in internal jugular vein and confirmed to be fixed in the right atrium by ECG guidance, and at the same time temperature sensing indwelling urinary catheter was fixed. Before entering the operating room, patients were dressed in intermittent pneumatic compressing stocking to decrease venous pooling.
Before positioning, patients received about 7 mL/Kg of a crystalloid isotonic fluid and if mean arterial pressure (MAP) was less than 20% from baseline, a vasoconstrictor agent Akrinor® (cafedrine/theodrenaline) was administered. The approved seated position in the hospital of study was a modified seated position; after patient's upper body was elevated 90 to 100 degrees, the head was 20 to 30 degrees tilted forward then legs elevated so that toes were at the level of ear tragus, and knees were slightly flexed over a pillow. Then the head was fixed with a Mayfield head holder. To prevent cervical hyper flexion and spinal injury, two-finger breadth distance between chin and sternum was kept. Precordial Doppler ultrasound probe was fixed over the right atrium and its position was verified by injecting 5 mL of normal saline through the right atrial catheter. Body temperature was kept over 36°C, using a Bair Hugger patient warming system. For every patient, intermittent pneumatic compressing stockings were used and activated after seated positioning.
Specific needles insertion for neurophysiological monitoring was performed after anesthesia establishment and before positioning, and therefore, any extremity mal-positioning and nerve retraction could be checked and prevented. When a specified sound in precordial Doppler ultrasound was heard or there was a 5-mm-Hg or more decrease in EtCO2 or hemodynamic instability without any other reason, venous air emboli (VAE) was suspected, and the neurosurgeon was informed and bilateral gentle jugular vein compression was performed in order to help find the site of air entry and close it by bone wax or coagulating the bleeding vessels. When it was not possible to find the air entry site, the field was covered with compresses soaked in saline. Aspiration of air was the last step to remove air bubbles and was approved as definite air emboli.
Approach to a cerebral desaturation event (CDE) was according to a protocol, first by administration of enough fluid and/or a vasoconstrictor to increase MAP and FiO2, then if not improved, by repositioning of the patient so that cerebral perfusion increased. Referring to previous studies (16), CDE was defined as reduction of rSO2 more than 20% from baseline or rSO2 decline to less than 40%.
The MAP, heart rate, rSO2, SPO2, Central Venous Pressure (CVP), and ETCO2 were recorded before and after anesthesia induction, intubation, before sitting positioning (pre-sitting) and on the 1st, 5th, 15th, 30th, 60th, and 120th minute after sitting positioning and also after supine repositioning at the end of surgery, and whenever a VAE or CDE was defined during anesthesia.
Only in refractory hypertension or obstructive airway disease, sevoflurane was used in addition to propofol infusion for anesthesia maintenance. At the end of surgery, patients were transferred to the Intensive Care Unit (ICU) and intubated or extubated, according to the type of surgery and anesthesiologist decision.
3. Results
The SPSS (version 16.0; SPSS, Chicago, IL) and Stata (version 12) softwares were used for the statistical analysis. Differences in rSO2 between right and left side were examined with the paired t test.
Changes in MAP and rSO2 with time were compared with the baseline values by the use of repeated-measures analysis of variance with Bonferroni correction to determine which time point had values significantly different from the baseline values. Univariable and multiple variable linear regression method was used to evaluate the effect of different variables on baseline rSO2. P values of < 0.05 were considered significant in all statistical tests.
A total number of 106 patients were enrolled in this study. Eleven patients violated the study protocol and their data was not analyzed. Demographic data of 95 patients was analyzed (Table 1).
| Variable | Mean | No. (%) |
|---|---|---|
| Age, y | 46.37 ± 13.73 | 95 |
| Gender (F/M) | - | 51 (53.7)/44 (46.3) |
| ASA (I/II/III) | 22/60/13 | |
| BMI, Kg/m2 | 25.84 ± 5.32 | |
| DM | 4 (4.2) | |
| HTN | 14 (14.7) | |
| History of β-blocker usage | 10 (10.5) | |
| IHD, Hb, mg/dL | 13 ± 1.4 | 4 (4.2) |
Demographic Data of Patients Included in the Present Study
Acoustic Neurinoma (47.4%) and Meningioma (18.9%) were the first and second most common tumors found in patients, respectively.
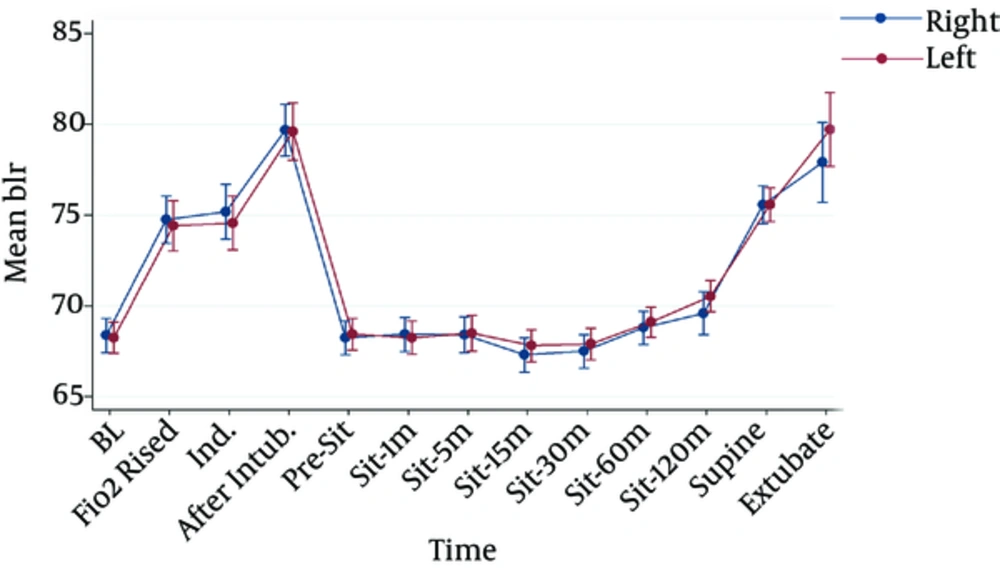
It was observed that there was not any significant difference between the right (68.4 ± 9.3) and left side (68.3 ± 8.4) rSO2 before induction of anesthesia and also at the other specific times that rSO2 was recorded (Figure 1).
There was no significant difference between baseline (68.36 ± 9.26) and pre-sitting (68.24 ± 8.96) rSO2 values; however, during the 15 minutes following the establishment of sitting position there was a statistically significant decrease in rSO2 compared with the pre-sitting time (67.30 ± 9.21) (P = 0.037). Consequently, on the 30th, 60th, and 120th minute after reaching the sitting position, rSO2 increased significantly compared with rSO2 of the 15th minute (Figure 1).
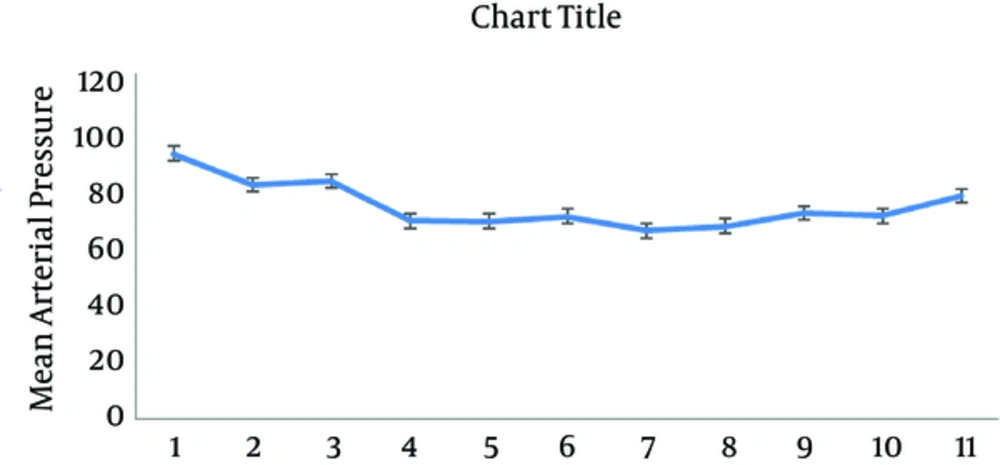
In this study, it was observed that there was a significant decrease in pre-sitting MAP (69.88 ± 11.51) compared with the baseline value (93.62 ± 10.08) (P = 0.00). Furthermore, in comparison with the pre-sitting measurement, a decrease in MAP on the 15th minute after sitting positioning was observed (66.55 ± 11.52) (P = 0.018) (Figure 2).
Forty-one cases of VAE (43.2%) were detected by precordial Doppler ultrasound. In 16 cases (39%), there was a decrease in ETCO2 (≥ 5 mmHg) while in 7 patients (7.3%) there was positive air bubbles aspiration assumed as definite VAE. The incidence of CDE was 7.3% (Table 2).
| Variable | Frequency, % |
|---|---|
| VAE (precordial Doppler) | 43.2 |
| Confirmed VAE (air bubble aspiration) | 7.3 |
| CDE | 7.3 |
| Clinically significant AUC (AUC > 50 min*%) | 2.1 |
VAE: Venous Air Emboli; CDE: Cerebral Desaturation Event; AUC: Area Under the Curve
In 43.2% of patients, a vasopressor was administered during anesthesia. Patients, who experienced a VAE event, received significantly higher amounts of vasopressor compared with patients without a VAE event (3.16 mL and 1.41 mL, respectively; P = 0.025).
Compared with non-diabetic patients, in patients with diabetes there was a more profound reduction of rSO2 on the 15th and 30th minute, following establishment of the sitting position (P = 0.041, P = 0.025).
Patients with positive history of beta-blocker usage had a significantly decreased MAP values in pre-sitting time compared to baseline (P = 0.01), yet this was not significant in the rest of the anesthesia time.
The BMI (P = 0.48), ASA class (P = 0.78), and age (P = 0.21) did not show any significant effect on baseline rSO2, yet lower pre-operative hemoglobin level and female gender were correlated with lower baseline rSO2 values (P = 0.04, β = 0.235 and P = 0.002, β = 0.753 respectively) (Table 3).
| Independent Variable | β | P Value |
|---|---|---|
| Gender | 0.753 | 0.002 |
| Age | 0.148 | 0.214 |
| DM | 0.056 | 0.681 |
| ASA | -0.034 | 0.785 |
| CHD | 0.088 | 0.455 |
| BMI | -0.088 | 0.410 |
| β blocker | 0.411 | 0.053 |
| HTN | -0.406 | 0.069 |
| Hemoglobin | 0.235 | 0.042 |
Effect of Different Variables on Baseline rSO2
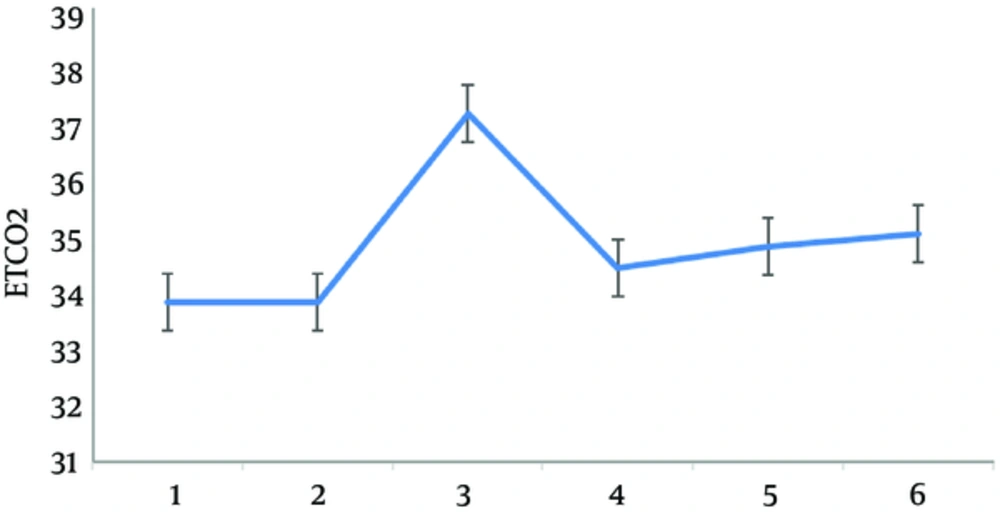
On the 15th (37.43 ± 3.22), 30th (34.98 ± 2.31), and 60th (35.22 ± 2.09) minute, after sitting positioning compared to the pre-sitting time (33.90 ± 3.03), an increase in ETCO2 was observed (P = 0.037, 0.001, 0.00), as shown in Figure 3.
4. Discussion
This study showed that changes in the position from supine to sitting in elective neurosurgical operations will not impose cerebral hypoxia even though there is a reduction of MAP after reaching the seated position.
Seated position provides a good field of surgery for posterior fossa craniotomies, yet there are some life threatening complications related to this position like tension pneumocephalus, venous air embolism (VAE), and paradoxical arterial embolus that has resulted in diminished use of this position, although VAE during neurosurgery is not attributed exclusively to the seated position and has frequently been reported in the prone and supine positions. For instance, VAE has been reported in 10% to 17% of craniotomies performed in the prone position (17).
The rSO2 values from right and left side was the same as base line until the end of surgery. A decrease of MAP from the time that patients entered the anesthesia induction room (baseline time) until the pre-sitting time was observed in this study, as it could contribute to the anesthetic drugs effect and absence of any surgical stimulation. A second decrease in MAP, 15 minutes after sitting positioning, was detected, yet there was not any rSO2 reduction from baseline measurement during the pre-sitting time. This could be contributed to increased FiO2 after mask ventilation and tracheal intubation. However, the trend of MAP values was the same as rSO2 values during the first 15 minutes following reaching the seated position. After 15 minutes of sitting, there was not any alteration in MAP and rSO2 compared with the pre-sitting time as a reference time after anesthesia induction. During the five minutes following sitting positioning despite gravity effect on blood pressure and anticipated hypotension, the researchers did not observe any decrease in MAP. As Mayfield® head holder is placed only after sitting positioning establishment, it could be assumed that increased central sympathetic output due to painful stimulation may increase MAP and consequently cerebral perfusion pressure, which over comes the gravity effect of the seated position. The rSO2 decrease on the 15th minute was statistically significant; however, this reduction from 68.24 ± to 67.30 ± 9.2, is not clinically important and will not imply any risk to patients.
No other risk from older age, increased BMI or higher ASA class on rSO2 values was found in this study, yet lower hemoglobin levels and female gender were correlated with lower baseline rSO2 values. The lower baseline rSO2 in patients with lower hemoglobin levels may be related to less O2 delivery to cerebral tissue. However, the reason for lower baseline rSO2 in female patients in this study was not clear and conducting further studies in the future is suggested.
Reduction of MAP and rSO2 in patients with diabetes on the 15th and the 30th minute after sitting positioning was more profound compared with non-diabetics, which could be contributed to autonomic dysregulation in this group of patients. In patients, who had a history of beta-blocker medications, there was a greater reduction of MAP at the pre-sitting time compared with baseline, which could be due to inhibition of sympathetic nervous system by these medications.
In this study, the incidence of VAE was 43.2%. The reported incidences of VAE in seated position surgeries vary depending on the type of surgery and the method of detection of VAE. In a systematic review of craniotomy studies, the incidence of VAE in seated position was 15% - 45% (18). This almost high incidence of VAE observed in the present study could be related to the VAE detection technique, which was done by precordial Doppler that has a high sensitivity compared to other techniques, like ETCO2, SpO2, and ECG. As most studies reporting the incidence of VAE have been conducted retrospectively, the possibility of data missing in the recorded documents of patients should be considered as well. In the present study, the researchers observed that 39% (16/41) of patients, who were suspected to have VAE by precordial Doppler also had an ETCO2 decrease (≥ 5 mmHg) and 17% (7/41) of them had visible air bubbles in aspirated blood from the central venous catheter.
One of the most feared complications after seated positioning is cerebral O2 desaturation. In the search of famous data bases, such as PubMed and ISI, the researchers could find only a few studies about cerebral O2 saturation changes after seated positioning in neurosurgical patients. Most published studies have investigated cerebral oxygenation on patients undergoing shoulder surgery in beach chair position, a kind of seated position, in which patient’s legs are not elevated enough and back bending is about 45 degrees. Pohl and Cullen reported a series of 4 otherwise healthy patients that after shoulder surgery in beach chair position demonstrated major brain injuries (11). Following these findings, the need for cerebral perfusion monitoring in the beach chair position has been cleared. Several authors recommend the use of cerebral oximetry to monitor cerebral perfusion (19). In beach chair position, different incidences of CDE have been reported. Murphy et al. (16) found episodes of CDE in 80% of patients operated in the beach chair position while Salazar et al. reported 18% of CDE in their prospective study (20).
In this study, the incidence of CDE was 7.3% and was less than the incidence that could be found in the literature from other published studies. The researchers assume that raising legs in modified sitting position to the level of Tragus leads to a better venous return and improves cardiac output. On the other hand, using total intra venous anesthesia (TIVA) with propofol and opioids for maintenance of anesthesia instead of using volatiles could prevent from profound positional hypotension. Lindoors et al. observed hypotension after seated positioning, and 69% of patients in their review were administered vasoactive agents during anesthesia (21) whereas 43.9% of the patients in the current study received vasopressor; administering 7 mL/kg isotonic crystalloid fluid to patients before changing position to the sitting position and using intermittent pneumatic compressing stockings for all patients in this study may play a role in the occurrence of less profound hypotension.
In comparison with the pre-sitting time on the 15th, 30th and 60th minute after sitting positioning, an increase in ETCO2 was observed. In seated position, ventilation of lungs improves and dead space is less and as a result ventilation/perfusion ratio increases. This increase in ETCO2 could be contributed to this phenomenon. Although a relatively high incidence of VAE was detected by Doppler ultrasound, there was only 2 patients (2.1%), who had AUC > 50 min%. The first case was a 19-year-old male, candidate for pineal tumor resection without any history of cardiovascular disease or any medical therapy, who had sudden rSO2 drop of more than 30% following sitting positioning and AUC = 220 min%. Cerebral desaturation started just after sitting positioning without considerable MAP changes and with unchanged central venous pressure. The anesthesia team had to increase FiO2 but rSO2 did not improve and finally the patient was repositioned to supine position and the initiation of surgery was postponed until rSO2 reached back to the safe level. The second case was a 48-year-old male, candidate for brainstem meningioma resection without a history of medical illness or any medical therapy, who had an rSO2 drop more than 30% and AUC = 55 min%, yet at separate times during anesthesia, which was accompanied by hypotension that responded to fluid loading and vasopressor therapy and in this case supine repositioning was not needed. In both cases, the researchers followed the post-operative course and there was not any new sequel in cognitive function or increased ICU admission or hospital stay according to patient documents.
In the present study, for ethical reasons, the responsible anesthesiologist was not blinded to the Cerebral Desaturation Events (CDE) and had to manage the situation, so the results may show lower incidence and severity of CDEs. Inclusion of only non-emergent cases for neurosurgical operations and lack of trans esophageal echocardiography were other limitations of this study.
To our knowledge, this prospective study with 95 cases was one of the largest studies in this field. According to the current findings, it could be suggested that the seated position could be considered as a safe position and applying modern monitoring instruments like cerebral oximetry or brain tissue oximetry, cardiac output monitoring, and TEE will further increase patients’ safety.
For future studies, the researchers recommend addition of cardiac output monitoring and measurement of changes in cardiac output and vascular resistance differences during position changes.
4.1. Conclusions
This study shows that changing the position from supine to sitting in elective neurosurgical operations will not impose cerebral hypoxia even though there is greater reduction of MAP after reaching the seated position.