1. Introduction
Third nerve palsy following closed head trauma may occur due to direct trauma to the nerves or indirect injury of the nerves via compression of the surrounding structures. Isolated involvement of peripheral fibers of the third nerve after head injury is a rare finding (1). In this article, we report a rare case of reversible peripheral third nerve palsy following avulsion of the sphenoid wing due to blunt head injury.
2. Case Presentation
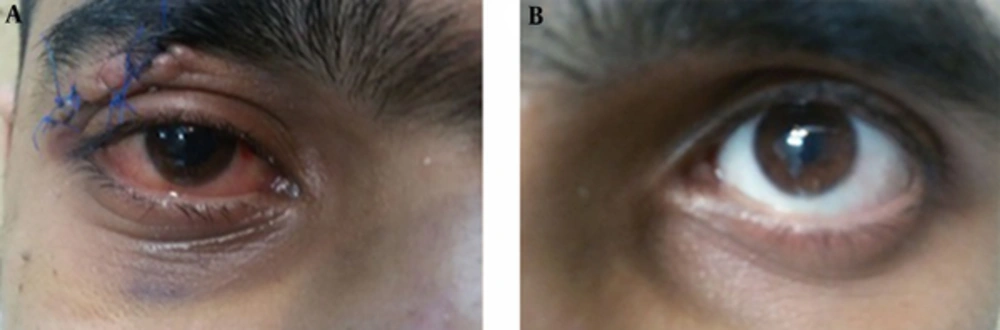
A 21-year-old man was admitted to our emergency department with blunt head injury due to a car crash into a tree. He had 1 episode of generalized tonic-clonic seizure immediately after the accident. Upon arrival, he was confused on examination (Glasgow coma scale score: 13/15). Also, multiple lacerations and abrasions were observed on his face and scalp. The vital signs were stable and no associated internal organ injury was detected. There was no focal neurological deficit, except asymmetry of pupils (Figure 1). The right pupil was dilated without any direct or consensual reaction to light. The extraocular movements were intact in all directions.
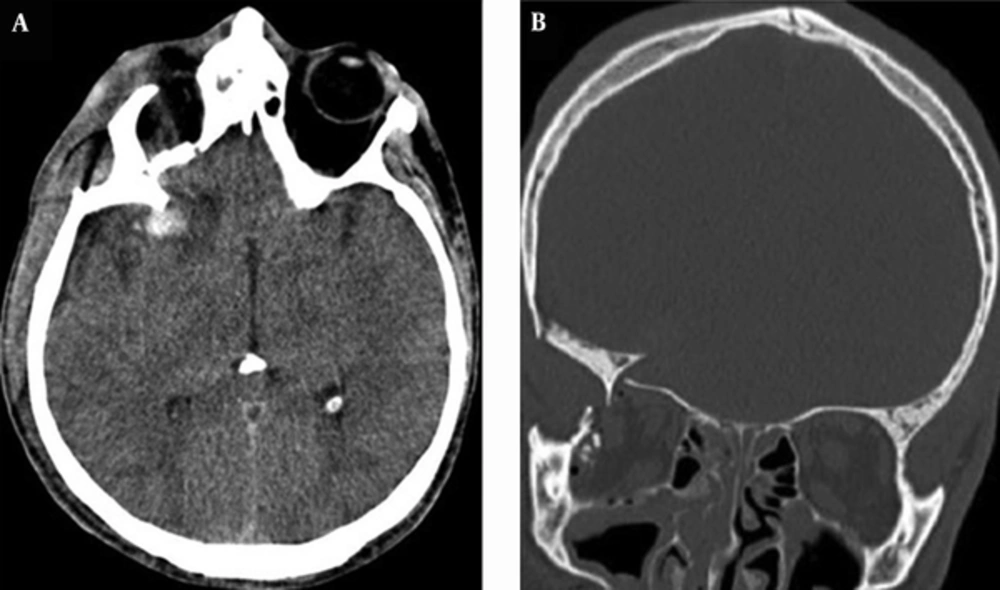
The brain CT scan showed complete avulsion of the right greater wing of the sphenoid bone with isolated contusion of the limen insula anterior to the Sylvian fissure (Figure 2A) and concomitant fractures of the orbital roof and floor (Figure 2B). The neuroophthalmology examination also confirmed right peripheral third nerve palsy without any signs of optic nerve damage.
Early and delayed (a 2-week interval) brain CT angiography showed no traumatic cerebrovascular injury, which was confirmed via digital subtraction angiography (DSA) 10 days later. In addition to standard treatments for traumatic brain injury, the patient received a short-term treatment with tapering doses of oral corticosteroids for his third nerve palsy (prednisolone started at 30 mg/day and tapered by 5 mg/day). Pupillary reactions and blurred vision started to recover about 10 days after admission, and full recovery was achieved after 1 week.
3. Discussion
Isolated third nerve palsy following mild to severe head injury has been reported by several researchers, whereas the occurrence of peripheral third nerve palsy after blunt head injury is a rare event (1). Solomons et al. (2) reported a 1.2% incidence of isolated direct third nerve palsy among 2100 patients with head injury during 12 years. They showed that direct injury to the third cranial nerve is much less common than indirect injury due to an expanding hematoma. Memon and Paine (3) reported an incidence of 1.1% for direct third nerve palsy among 1100 cases of head injury over 10 years. No cases of isolated third nerve palsy were reported following mild head injury in these studies.
Moreover, Tiffin et al. (4) performed a retrospective study on the etiology of acquired third, fourth, and sixth cranial nerve palsies over 9 years. They found no cases of isolated third nerve palsy attributable to trauma. In a larger retrospective study on 4176 cases of acquired third, fourth, and sixth cranial nerve palsies over 40 years, Richards et al. (5) reported an incidence of 15% for isolated third nerve palsy attributable to head trauma. They also reported that trauma is the most common cause of fourth nerve palsy, which can occur after apparently trivial head traumas, probably because of its long intracranial course and very slender connection to the brain stem.
The fibers of the third nerve are normally arranged in a way that the parasympathetic fibers of pupil are located at the periphery, and the somatic motor axons of the extraocular muscles are located at the center of the nerve. The mechanisms proposed for traumatic third nerve palsy include injury at its exit site from the brainstem (1-5), compression at the tentorial notch due to brain herniation (indirect injury), and injury at the superior orbital fissure (1-5).
Nevertheless, the underlying mechanism responsible for isolated peripheral third nerve palsy, similar to our case, has not been discussed so far. One possible explanation could be traumatic aneurysm of the posterior communicating artery, while normal brain CT angiography and delayed DSA ruled out this mechanism in our patient. Another possible mechanism could be transmission of decelerating and traction forces to the content of the superior orbital fissure (SOF) after the initial impact (1). This mechanism also seems unlikely in our case, as the third, fourth, and sixth cranial nerves are located in close vicinity to each other at the anterior end of cavernous sinus and SOF, and isolated injury of the third nerve is not a common finding in lesions of this region.
Another possible mechanism of third nerve injury could be distortion and stretching of delicate blood vessels, supplying relatively less perfuse peripheral fibers of the third cranial nerve1 in our case. This could explain recovery of paresis after restoring microcirculation of the nerve. The most probable mechanism for third nerve paresis in the present case seems to be direct stretching and distortion of nerve fibers on the oculomotor cistern before entering the SOF. Also, because of eyelid laceration and direct trauma to the globe, transient unresponsiveness of iris muscles could be another assumption.
To the best of our knowledge, this is the first report of isolated peripheral third nerve palsy following blunt head injury in the English-language literature.