1. Background
Hearing deficit is the third most common chronic disorder that affects the health status largely and seriously, leading to stress in the patient and the family (1). The prevalence of moderate to profound hearing deficits in children (including sensorineural and conductive impairments) is one to six per 1,000 children. Moreover, 440 million children worldwide are estimated to suffer from over 85 decibels hearing deficit and when the threshold is decreased to 50 decibels, it amounts to about 800 million (2).
Hearing deficit is mostly defined as a communication deficit. Although the communication deficit is an important disorder, hearing deficit co-occurs with other physical impairments such as vestibular disorders (3). Rine et al. (4) believe that as labyrinths and cochlea are anatomically and developmentally interrelated, there is a potentiality for vestibular impairment when the hearing mechanism is impaired. In a study using Barany Rotary test and caloric stimulation, Arnvig (5) found that 82% of 89 children with severe acquired hearing deficits and 34% of 129 children with hereditary hearing deficits had abnormal responses to vestibular tests.
Since the vestibular system activates vestibular reflex mechanisms trying to stabilize the eyes, head, and body in the space, impairment of this mechanism may affect postural sensitivity. Contemporary literature adheres that deaf people show lower dynamic and static balance than people with normal hearing (6). Lindsey and O’Neal (7) found that deaf children had a very weaker performance in static and dynamic balance skills than hearing children.
Development and control of the posture are important prerequisites for skill motor function (8). Crowe and Horak (9) found that children with hearing deficits and impaired sensory organization had weak balance and motor efficiency in many fields. Various studies on motor skills in deaf children have reported deficits in balance, general dynamic coordination, visual-motor skills, ball catching ability, and some disturbances in reaction time and speed of movements (10). Teachers of children with hearing impairment often complain of non-coordination, clumsiness, and balance deficit in such children, preventing the child from the desired function (3).
Deaf children are also reported to show behavioral problems related to impulse control, distractibility, and sustained attention disability in the visual system. Recently, some impairments have been reported in continuous visual function tasks in deaf children. On the other hand, younger deaf children are more distracted by the information existing in their peripheral visual field unrelated to their tasks (11). In recent years, the most important instructions used for learning and teaching motor skills are attentional instructions that direct the attention of learners to different aspects of movement (12).
Cochlear implantation is the common treatment currently considered for children with hearing deficits. Many researchers question the effect of cochlear implants on balance and motor development (3). The effect of this method on the motor ability of deaf children was investigated by Gheysen et al. (10), who found that children with cochlear implants did not have better motor function than other children. On the other hand, another study indicated that almost three-fourth of adults undergoing such a surgery experienced vertigo and imbalance (13). Furthermore, the effect of a program including only static balance exercise on the static balance ability of deaf children was assessed in a 10-day period, which indicated no significant effect (6). However, in another study, by using a balance program together with body awareness, Lewis et al. (14) found improvements in the balance skills of children aged 6 to 8 years. But, the above-mentioned study was conducted as a pilot study with a limited number of patients, which cannot represent the population with hearing deficit (14). In addition, Majlesi et al. (15) performed an interventional program for static balance and gait in deaf children. This program, which was merely based on proprioceptive training, improved static balance, but had no significant effect on the speed of gait (15)
In spite of the above facts, motor and balance impairment assessments have not yet been included in common assessments of deaf children; also, occupational therapy and physical therapy have not yet been introduced into training and rehabilitation programs of such children (2). Interventional programs focusing on motor impairments in children with hearing deficits should consider vestibular and motor function with an emphasis on the improvement of visual and somatosensory effects (3). Despite the growing evidence of the benefits of exercise for health, the available literature lacks clinical evidence that supports exercise guidelines to improve cognitive and motor abilities (16). On the one hand, effective rehabilitation methods are not used to improve balance impairment, as well as motor coordination and the attention of children with hearing deficits. On the other hand, there are a few studies on motor function, attention, and balance impairment of such children.
2. Objectives
Thus, the current study aimed to investigate the effect of an exercise program based on balance and vestibular sensorimotor stimuli on balance function, motor coordination, and attention in children with hearing deficits.
3. Methods
3.1. Participants
This experimental interventional study was conducted on a statistical population including 36 children aged 7 to 12 years with severe to profound hearing deficits, as reported in the patients’ files. The children were studying in elementary schools for the deaf in Ghom Province, and obtained the standard score below 12 for the balance subtest of Bruininks-Oseretsky test of motor proficiency (indicating lower than average balance function according to the instructions of the test). These children had normal intelligence quotient and did not take medications affecting the central nervous system; they also did not have orthopedic and neurological impairments. They were excluded from the study in the case of being absent from more than two sessions, non-cooperation of the family, and the occurrence of orthopedic accidents and if diseases prevented the patient from participation. The Ethics Committee of Shahid Beheshti University of Medical Sciences approved the study (ethical code IR.SBMU.REC.1396.103).
The children participated in this study after obtaining the parents’ consent, fully explaining the objectives and the procedure of the study to the parents, and completing a demographic data form. The subjects were assigned to experimental or control groups by using permuted block randomization and considering the homogenization of the groups for age, sex, and balance performance. Therefore, 18 subjects were assigned to the control group and 18 subjects to the experimental group. Then, pretests were implemented in both groups. Thereafter, in addition to regular educational programs of the school, a balance, vestibular, sensory, and motor exercise program was implemented for the experimental group. During this period, the control group performed regular educational programs of the school. At the end of the intervention period, posttests were implemented for both control and experimental groups and the obtained results were compared between the pre- and post-intervention phases and between the control and experimental groups. It is necessary to mention that the tests were implemented by an Occupational therapist working in the school who was not aware of group allocation. The intervention program was accomplished by the investigator.
3.2. Intervention Program
This program was compiled from the subject-related research plans. The items of the program were selected as follows: first, 90 exercises were selected from the relevant articles and literature (6, 17-22) and were presented to the experts who were asked to select the exercises they thought to fit. Then, by summing their comments on the type and difficulty level of exercises, finally, 33 exercises at difficulty levels of A, B, and C were selected. They were presented for final approval to six other experts with work experience in the pediatric field. Next, the researcher selected the exercises of each session from the prepared exercise package from easy to difficult by considering the ability level of each child. The exercises began at level A; any exercise that was not challenging for each person in two consecutive sessions was replaced with a more difficult one. On average, 14 exercises were performed in each session.
The program was implemented in three 45-min sessions per week for four weeks in the Occupational Therapy Department of Ababasir School of Ghom. Moreover, three exercises were assigned as home exercises between the sessions; to make sure that the program was performed at home, the family was asked to film the exercise implementation. Such a session structure has previously been used in the study by Majlesi et al. (15), except that home exercise was not considered in that study.
Since the obtained results proved the hypotheses, the exercise program was offered to the occupational therapists working in elementary schools for the deaf in Ghom Province to implement on the control group.
3.3. Assessments and Tests
In this study, the following tests were used in the pretest and posttest for the assessment purpose.
For the assessment of balance performance, we used the balance subtest of the Bruininks-Oseretsky test of motor proficiency. For the assessment of motor coordination, we used the upper limb coordination, bilateral coordination, and visual-motor control subtests of the Bruininks-Oseretsky test of motor proficiency. For the assessment of attention, we used the Continuous Performance test.
In this study, the scores of the subtests were obtained according to the test instruction and used for comparing the results of the Bruininks-Oseretsky test of motor proficiency. The number of correct responses, calculated by the subtraction of omission errors and commission errors from the total number of stimuli, was used for comparing the results of the Continuous Performance test. It is necessary to note that the tests were performed by the occupational therapist working at the Ababasir School of Ghom, and the results were recorded by the researcher.
The Bruininks-Oseretsky test of motor proficiency is one of the most common tools for children aged 4.5 to 14.5 years. The full set of this test includes 46 items that are categorized into eight subtests (23). In this test, four subtests assess gross motor skills, three subtests assess fine motor skills, and one subtest assesses both. Bruininks standardized this test on a sample of 756 children. The test-retest reliability coefficient and the validity of the test were reported to be 0.78 and 0.84, respectively (24). The validity and reliability of this test were examined by Mousavi et al. in Iran, with the validity coefficient of 0.78 (25).
The Continuous Performance test is a special assessment test with the potential of objective evaluation of attention. The available versions of the Continuous Performance test are performed by personal computers. According to Kelly and Garfinkle, the Continuous Performance test has the potential to examine sustained attention (26). In this study, we used the Persian form of the Continuous Performance test developed by Hadianfard et al. (27). This form has 150 Persian digits as stimuli, from which 30 are target stimuli. The time interval between the presentation of two stimuli is 500 thousandth of a second and the duration of the presentation of each stimulus is 150 thousandth of a second. The above-mentioned researchers obtained reliability coefficients ranging from 0.59 to 0.93 for different parts of this test through retesting at the interval of 20 days in a sample of 43 elementary school boys, calculating all the coefficients at a significance level of 0.001. Furthermore, the above-mentioned researchers reported a desirable validity for this test through criterion validation (27).
3.4. Statistical Analysis
The Shapiro-Wilk test was used for assessing the normality of data distribution. For the data with normal distribution, paired and independent samples t-tests were used for within and between-group comparisons, respectively. For the data with non-normal distribution, we used the Wilcoxon signed-rank test and the Man-Whitney test.
4. Results
The results of this study indicated that 20 (55.6%) participants were females, including 10 subjects in the experimental group and 10 in the control group, and 16 (44.4%) participants were males, including eight subjects in the experimental group and eight in the control group. Furthermore, the mean age was 9.72 years and 9.67 years in the experimental and control groups, respectively, indicating no significant difference. Given the results of Table 1, the control and experimental groups were homogenous with respect to age and sex.
| Experimental Group | Control Group | P Value | |
|---|---|---|---|
| Gender | |||
| Female | 10 (55.6) | 10 (55.6) | |
| Male | 8 (44.4) | 8 (44.4) | |
| Age | 9.72 ± 1.742 | 9.67 ± 1.879 | 0.859 |
aValues are expressed as mean ± SD or No. (%).
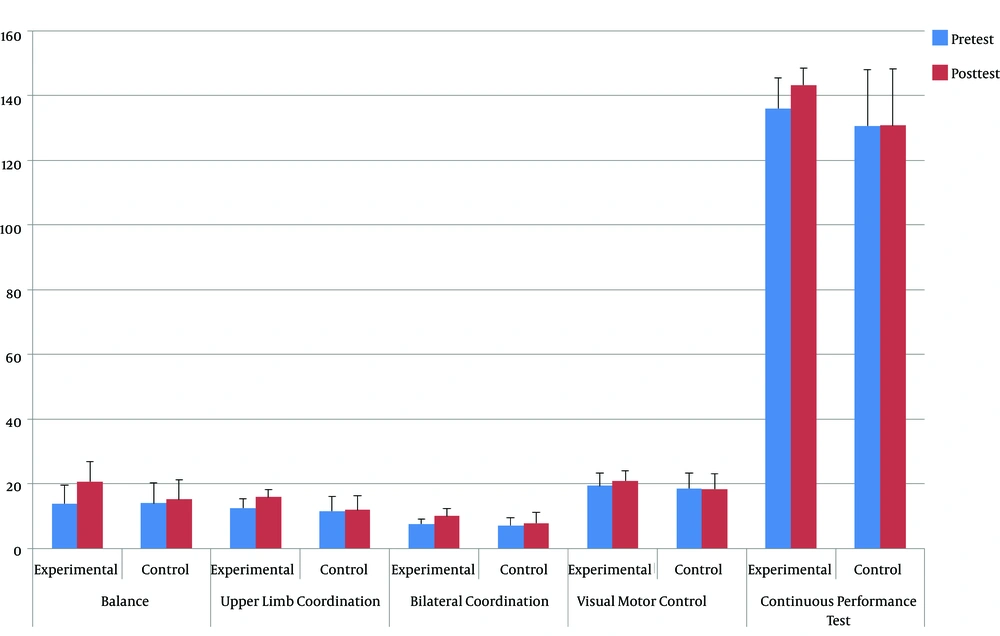
Based on Table 2, there were significant differences between the mean pretest and posttest scores of balance, upper limb coordination, bilateral coordination, and visual-motor control subtests of the Bruininks-Oseretsky test in the experimental group (P = 0.000, P = 0.000, P = 0.000, and P = 0.008, respectively). On the other hand, there were no significant differences between the mean pretest scores of these subtests between the control and experimental groups (P = 0.956, P = 0.477, P = 0.481, and P = 0.622, respectively). In addition, the mean difference in the posttest and pretest scores were compared between the control and experimental groups, which indicated a significant difference between them (P = 0.000, P = 0.000, P = 0.004, and P = 0.023, respectively).
| Test | Pretest | Posttest | P Valueb | Difference (Posttest-Pretest) |
|---|---|---|---|---|
| Balance | ||||
| Experimental | 13.94 ± 5.724 | 20.72 ± 6.285 | 0.000b | 6.7778 ± 2.263 |
| Control | 14.06 ± 6.207 | 15.22 ± 6.195 | 0.085b | 1.1667 ± 2.706 |
| P valuec | 0.000c | |||
| Upper Limb Coordination | ||||
| Experimental | 12.44 ± 2.812 | 15.94 ± 2.235 | 0.000b | 3.50 ± 1.248 |
| Control | 11.56 ± 4.409 | 11.94 ± 4.385 | 0.441b | 0.388 ± 2.090 |
| P valuec | 0.000c | |||
| Bilateral Coordination | ||||
| Experimental | 7.61 ± 1.461 | 10 ± 2.425 | 0.000b | 2.388 ± 1.377 |
| Control | 7.11 ± 2.587 | 7.83 ± 3.365 | 0.108b | 0.722 ± 1.808 |
| P valuec | 0.004c | |||
| Visual Motor Control | ||||
| Experimental | 19.44 ± 3.959 | 20.94 ± 3.058 | 0.008b | 1.50 ± 2.093 |
| Control | 18.61 ± 4.791 | 18.39 ± 4.667 | 0.631b | -0.222 ± 1.864 |
| P valuec | 0.023c | |||
| Continuous Performance | ||||
| Experimental | 136.06 ± 9.321 | 143.33 ± 5.303 | 0.002b | 7.277 ± 8.470 |
| Control | 130.72 ± 17.428 | 130.78 ± 17.421 | 0.906b | 0.055 ± 8.768 |
| P valuec | 0.017c |
aValues are expressed as mean ± SD.
bWithin-group comparisons.
cBetween-group comparisons.
There were significant differences between the mean pretest and posttest scores of the Continuous Performance test in the experimental group (P = 0.002). On the other hand, the mean pretest scores of the Continuous Performance test showed no significant difference between the control and experimental groups (P = 0.537). In addition, the mean differences between the posttest and pretest scores were compared between the control and experimental groups, which indicated a significant difference between them (P = 0.017).
As indicated in Figure 1, the differences between the mean pretest and posttest scores were higher in the experimental group than in the control group in all tests.
5. Discussion
The results of the present study indicated that the application of 12 sessions of balance and vestibular exercise protocol, as used in this study, combined with three exercises done under the supervision of the family between the sessions, results in the significant improvement of balance, motor coordination, and attention in children with severe and profound hearing deficit.
The balance process emphasizes on the integration of information from proprioceptive, vestibular, and visual systems in order to produce appropriate muscular responses for postural adaptation so as to keep the center of gravity on the base of support of the body (28). Due to the involvement of these sensory systems in the balance process and the special attention paid to the sensory systems, especially the vestibular system, the exercises are expected to improve the static and dynamic balance, as proved by the results of this study.
Furthermore, three items of upper limb coordination, bilateral coordination, and visual-motor control were considered for the investigation of motor coordination. For postural control, two mechanisms are considered: feedback control that corrects balance perturbation and feedforward control that is predictive. The start of a movement with good coordination requires postural adaptations that predict the imbalance resulting from that movement (29). Studies suggest that balance disorders may have a negative effect on such motor skills as general dynamic coordination and eye coordination (15). In a study by Butterfield and Ersing (30), it was revealed that dynamic and static balance affected the ball catching ability in deaf students. Considering the foregoing, we expect that by the improvement of balance performance, an improvement is observed in motor coordination items in children with hearing deficits. Such a result was observed for all the three studied items, but the improvement was higher in upper limb coordination than in the other two items.
On the other hand, it is suggested that the integration of the information from different senses is a necessary component for the normal development of attention function in each sensory modality of the individual (11). In another theory on attention-deficient, it is also suggested that deaf children spread their attention over a broad visual field in a non-concentrated manner (31). Since vestibular, proprioceptive, and visual senses are integrated to create and keep balance in balance exercises and since the visual field is limited to a specific point in some exercises in the protocol, improved attention was expected by performing such balance exercises, as proved by the results of this study.
The results of the present study are comparable to the results obtained by Horn et al. (32), Yucel and Derim (33), Shin et al. (34) for attention and the results obtained by Lewis et al. (14), Effgen (6), Majlesi et al. (15), Fotiadou et al. (35), and Rajendran et al. (36) for balance disorders and motor skills.
Horn et al. (32) conducted a retrospective longitudinal study on continuous performance in deaf children undergoing cochlear implantation. Such children had weak sustained attention and showed a little improvement as the years of using a cochlear implant increased. The results of the present study indicated that a cochlear implant led to improved performance on a test of sustained visual processing of numbers over two or more years (32). The above-mentioned results are consistent with those of the present study, except that improved sustained attention was observed in a much shorter period in the present study. In another study, Yucel and Derim (33) reported that deaf children with cochlear implants had higher attention deficit and irritability than the control group with no hearing deficit and deaf children with cochlear implants after the age of four had weaker performance than children with implants at lower ages. However, since within-group comparisons were not made in this study and since sustained attention was not assessed before cochlear implantation, the effect of this method may not be judged accurately. In addition, in a study on children aged 6 - 7 years, Shin et al. (34) reported that attention deficit and irritability increased after cochlear implant surgery. The whole results of these studies do not prove the positive effect of cochlear implants on the attention of deaf children. However, in the present study, after using the balance and vestibular exercise protocol, there was a significant increase in sustained attention, which was assessed based on the number of correct responses in the Continuous Performance test.
Lewis et al. (14) found that participation in body awareness and balance program could lead to improved balance skills in children with hearing deficits. This report is consistent with the results of the present study, but Lewis et al. (14) considered a significance level of 0.1 for changes in that pilot study and like the present study, the balance subtest of Bruininks-Oseretsky test of motor proficiency was used for the assessment of dynamic and static balance; this is while in the present study, a significant increase was observed in the mean balance scores after using the balance and vestibular exercise protocol by considering the significance level of 0.05. In another study, Effgen (6) examined the effect of a 10-day exercise program on static balance activities in severe deaf children, and found no significant change in the amount of sway in spite of the improvement in standing time, which is indicative of no change in standing quality. This study, in which force platform was used for the investigation of balance, is consistent with the present study with respect to changes in standing quantity, but since no tool was used for the investigation of the amount of sway in static states in the present study, no special comment may be made on the comparison of the amount of sway between the two studies. On the other hand, unlike the study by Effgen (6), the assessment tool in the present study showed simultaneous improvement in both static and dynamic balance. Furthermore, the results of the present study are consistent with part of the results by Majlesi et al. (15), who investigated the effect of an intervention program focusing on proprioception on static balance and gait of deaf children. The results of that study indicated improvement in the amount of sway in static states, while there was no improvement in the acceleration of gait. Among the reasons stated for such a lack of improvement in that study, we can point to the ineffectiveness of the type of exercises performed on the gait of deaf children and the short duration of exercise program (15). Fotiadou et al. (35) also studied the effect of a rhythmic gymnastics program on the dynamic balance ability of a group of deaf children. The results of this study, which indicated a significant improvement in dynamic balance ability after rhythmic gymnastics program in deaf children, are consistent with the results of the present study (35). However, only one aspect of balance was considered in this study, in such a way that all exercises included dynamic exercises and only dynamic balance was assessed, which gave no information on static balance. In one of the few studies that assessed the effect of vestibular neuromuscular training simultaneously on motor skills and balance in six weeks, Rajendran et al. (36) obtained the results similar to those of the present study.
5.1. Limitations
The presence of a large number of dependent variables led to the extension of assessment times and consequently the study duration, and also made difficult homogenization of the control and experimental groups. On the other hand, due to a large number of variables that should be homogenized in the control and experimental groups, some conditions of the participants such as hearing aid use and/or cochlear implant surgery history were disregarded in the homogenization of the control and experimental groups.
5.2. Conclusions
The results obtained from the present study indicate that:
(1) Balance exercises lead to improved balance performance in children with severe and profound hearing deficits; (2) balance exercises lead to improved motor coordination (upper limb coordination, bilateral coordination, visual-motor control) in children with severe and profound hearing deficits; and (3) balance exercises lead to improved attention in children with severe and profound hearing deficits.
These results reveal the necessity of the application of balance exercise programs, especially those focusing on the vestibular system, for improvement of the mentioned fields in children with hearing deficits.
Using the present exercise package is suggested for other groups of patients with problems in balance, motor coordination, and attention, as well as for other age groups of deaf children.