1. Introduction
Metastatic involvement of the spine may present with pathologic fractures, deformity, neurologic deficit due to vertebral canal compromise, and pain. Pain is usually localized and constant and aggravates with the recumbent position. The management of pain mainly consists of medical therapy with non-steroidal anti-inflammatory agents, corticosteroid injection, hormone replacement therapy, and therapeutics with the osteogenic property such as calcitonin.
Percutaneous vertebroplasty was first described by Galibert and colleagues in 1984 for treatment of vertebral angioma (1), which is now recognized as a standard treatment for painful osteoporotic fractures and vertebral metastases. Vertebroplasty has been shown to induce immediate and durable pain relief as much as 80% to 90%, with an acceptable complication rate of 2% - 4%.
Vertebroplasty in the thoracolumbar spine is usually performed via the transpedicular, and less frequently, costopedicular and paravertebral routes. Lower and mid-cervical vertebroplasty is typically addressed with the anterolateral approach, introducing the needle between the upper airway medially and carotid-jugular vessels laterally (2, 3). Vertebroplasty of C2 has been practiced via percutaneous (4) transpedicular and direct trans-oral (5) routes. Although technically challenging, trans-oral vertebroplasty provides a safe procedure for augmentation of the C2 vertebra and may prove as the standard treatment for painful metastatic involvement. Besides pain relief through an exothermic reaction at bone-poly-methyl methacrylate (PMMA) (6) interface through destroying sensitized nociceptor endings, PMMA has shown to possess oncolytic (7) properties. Herein, we present a 41-year-old woman, a known case of breast cancer with metastatic involvement of the odontoid process and the body of the second cervical vertebra, whose painful and disabling lesion was tackled with stand-alone transoral vertebroplasty, with preserving normal motion, stability, and no recurrence after a 36-month follow-up.
2. Case Presentation
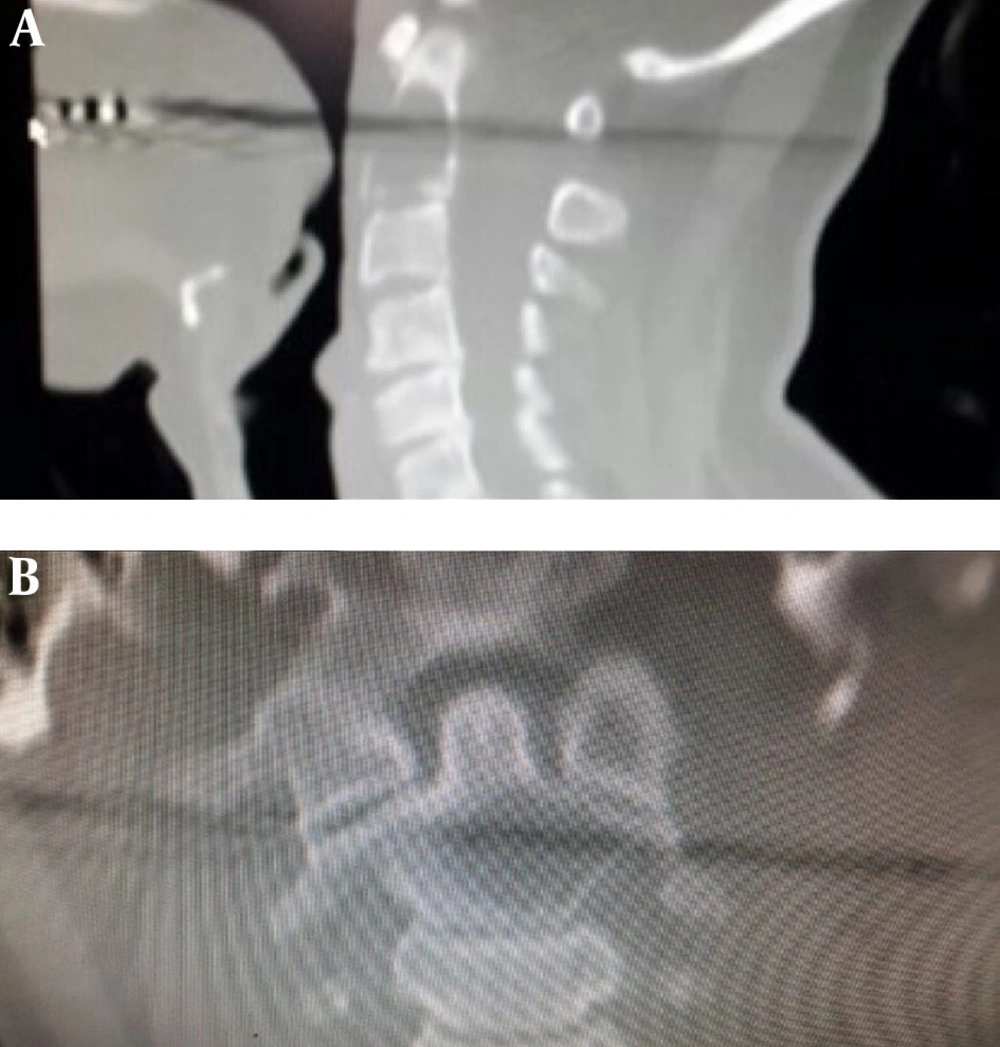
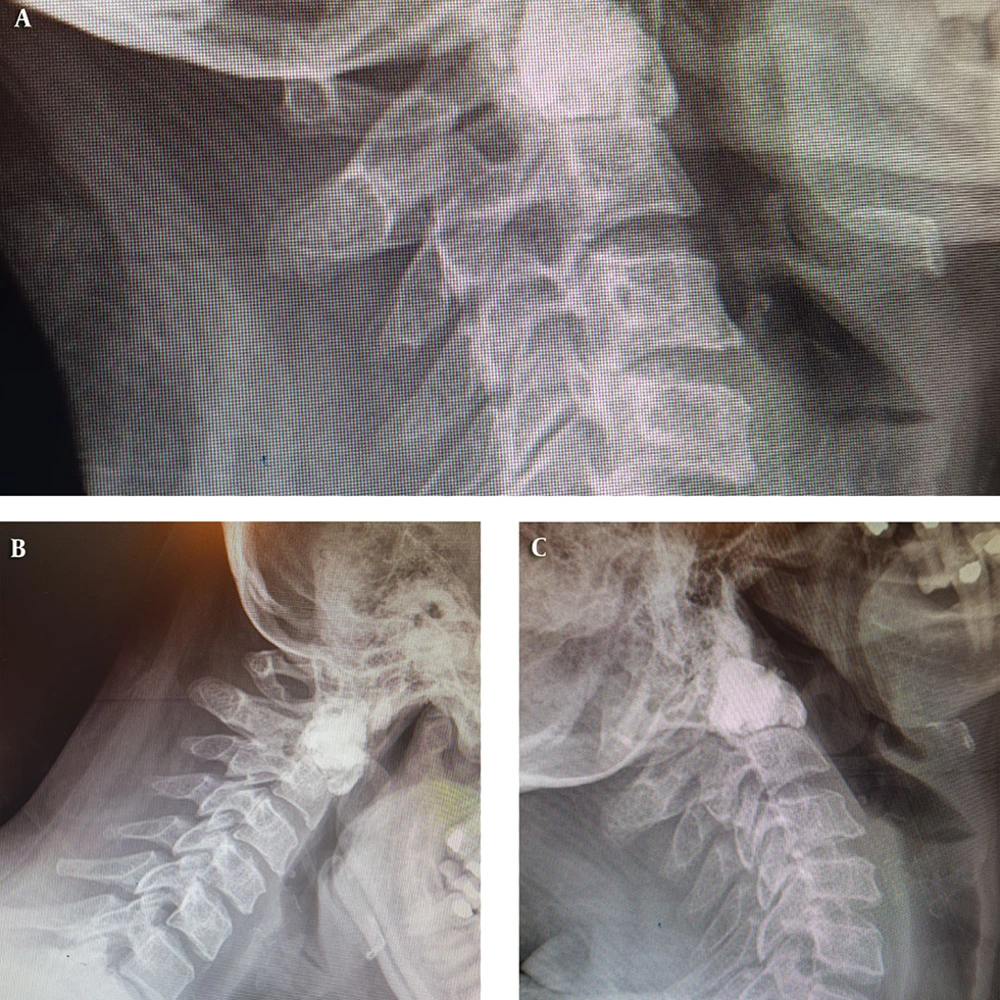
A 41-year-old woman, a known case of breast cancer, with a history of severe neck pain for three months, who had no improvement with analgesics and collar, was referred to our Neurospine clinic. On the day of the first visit, her visual analog scale (VAS) score was 10. Her physical examination revealed upper cervical tenderness without any neurologic deficits. Cervical CT scan showed a well-defined osteolytic lesion in the odontoid process with extension into the body of the axis (Figure 1). After discussing the potential risks of the procedure with the patient and her family, informed consent was obtained for operation.
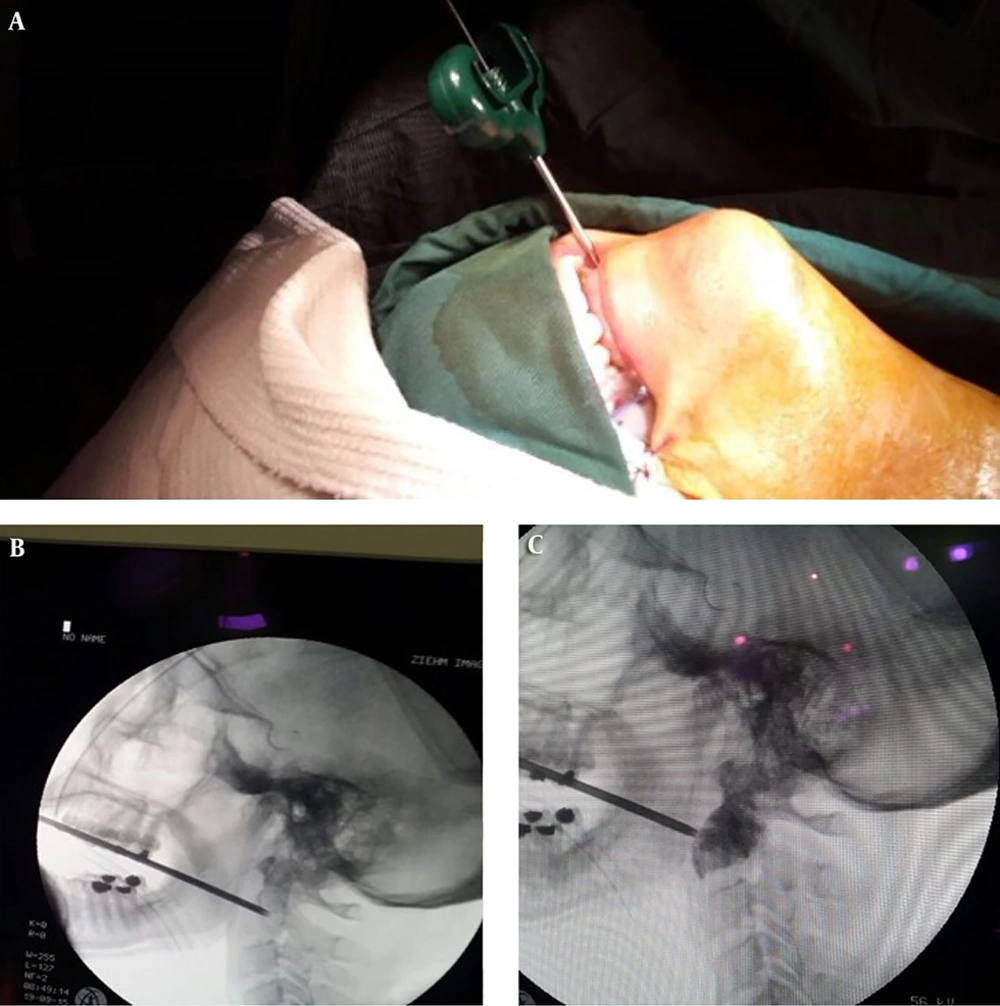
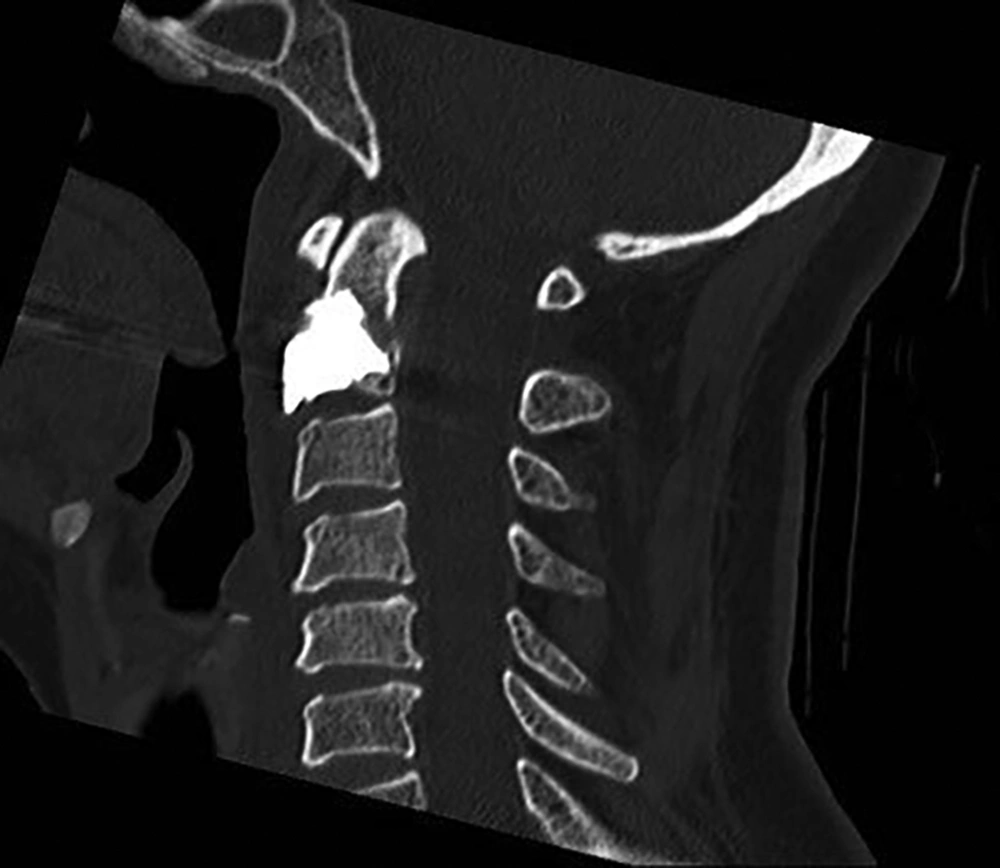
Following general anesthesia and fiber-optic nasotracheal intubation, the patient was positioned supine, the neck was extended, and a roll was placed under the patient’s shoulder between the scapulae. A Dingman mouth gag was placed and blades were adjusted to provide a corridor toward the oropharynx. The oropharyngeal mucosa was then prepped with povidone-iodine solution and the surgical site at the oropharynx was injected with lidocaine/epinephrine solution (1%, 1: 100,000). Under biplanar fluoroscopic guidance, a 22-gauge needle was introduced to the pharynx, which was further replaced by a 6-inch 13-gauge Jamshidi® needle. With the aid of continuous fluoroscopic guidance, approximately 2 cc of PMMA was slowly injected to fill the lesion and after 5 minutes, the needle was gently retracted. Fluoroscopic images confirmed the successful filling of the defect without leakage of the cement (Figure 2). Immediately after recovery from general anesthesia, the patient’s VAS score was 5. In the postoperative course, a rigid cervical collar was fixed for the patient for one month (Figure 3).
The VAS score, which was 10 prior to operation, decreased to 5 immediately after recovery from general anesthesia and improved to 2 at the six-month follow-up visit. At the 36-month follow-up visit, normal cervical motions were preserved, the VAS score was 0, and dynamic lateral cervical X-ray disclosed no instability (Figure 4).
3. Discussion
Metastasis to the spine may present with pain, pathologic fractures, and devastating neurological compromise. Vertebroplasty is an effective measure for the treatment of painful metastatic spinal disease in mid to lower cervical and thoracolumbar vertebrae. Injection of PMMA not only results in pain relief, but also has shown to possess oncolytic properties and enhance the cervical spine biomechanics with improving stiffness and axial load-bearing characteristics. Vertebroplasty in the upper cervical spine is technically challenging through anterolateral and transpedicular approaches, with potential complications of endangering carotid-jugular and vertebral arteries, respectively. We believe that trans-oral vertebroplasty can be safely practiced as the standard approach to avoid the potential devastating vascular complications of the aforementioned routes.
A few instances of this technique in practice are available in the literature. Anselmetti et al. (8) reported CT-guided trans-oral vertebroplasty in 25 patients with C2 metastasis for pain palliation. Their series showed the efficacy of this treatment with significant improvement in VAS scores with 24% of cement leakage. Of note, in this case-series, we found that female patients and those who suffered metastasis from breast cancer had more chance of becoming pain-free after vertebroplasty (VAS = 0). It is unclear whether the response of pain palliation to this procedure is different between the types of metastasis origin and genders and this issue merits further investigation.
In another study by Papp et al. (9) the transoral vertebroplasty of C2 metastatic lesion was practiced, followed by posterior fusion. We believe that vertebroplasty not only alleviates pain but also enhances the biomechanical properties of the axis to withstand axial load and in the absence of pre-operative overt instability, posterior fusion is necessary (10). However, posterior fusion limits motion so it can negatively affect the quality of life.
Herein, we presented our experience with transoral vertebroplasty of a painful C2 metastasis, with an emphasis on the preservation of normal cervical motion and biomechanics through avoiding an unnecessary posterior fusion procedure, with the durability of pain palliation after 36-months and no recurrences. We agree that this procedure has a high risk of infection and bleeding, as of other minimally-invasive lesions. Careful case selection, meticulous technique, and experience with trans-oral procedures are essential prior to proceeding with this approach.
3.1. Conclusions
Trans-oral vertebroplasty is a feasible, safe, and effective minimally-invasive procedure for palliation of painful C2 metastatic lesions. Avoiding a posterior fusion operation, we believe that normal cervical motion and stability can be preserved with this procedure, along with an improved quality of life.