1. Background
Acceleromyography, mechanomyography, electromyography, and phonomyography are used to monitor intraoperative neuromuscular blockade (1). Electromyography (EMG) is based on the principle that the compound action potential of the muscle is proportional to the number of motor units that get activated in response to nerve stimulation (2). Classically, the train-of-four (TOF) = 0 in the peripheral muscle of adductor pollicis is used as an endpoint for endotracheal intubation occurring at approximately three minutes.
Entropy monitors the depth of anesthesia. It acquires the electroencephalogram (EEG) and EMG of the underlying muscles. It processes the raw signals to derive two clinically useful values from the data, response entropy (RE) and state entropy (SE) (3). RE is computed over 0.8 to 47 Hz, with values ranging from 0 to 100. It incorporates both the EEG and the EMG. For computing SE, the frequencies associated with the EMG signal are filtered out. It includes the frequencies between 0.8 and 32 Hz, which are associated with EEG activity. The reported SE values range 0-91 (4). Thus, the difference between response entropy and state entropy (RE-SE) represents the EMG of the muscles under the entropy electrode (5, 6).
The RE-SE value is nine in resting conditions. It has been the focus of various studies, with some concluding that the decreasing values, i.e. RE-SE ≤ 2, represent nociception and some inferring that this decrease occurs only with increasing neuromuscular blockade (5, 7). The frontalis, orbicularis oculi, and corrugator supercilii are centrally-placed muscles on the forehead over which the entropy electrode is placed (8, 9).
Adequate conditions for endotracheal intubation require a combination of hypnosis, muscle paralysis, and analgesia. We hypothesized that as the entropy electrode is placed centrally, decreasing values of RE-SE ≤ 2 with SE ≤ 45 would denote adequate conditions required for endotracheal intubation. This could result in earlier intubation than when guided by TOF = 0, which is peripherally placed over adductor pollicis.
2. Objectives
Therefore, the primary objective of the present study was to evaluate if entropy values of RE-SE ≤ 2 with SE ≤ 45 can be used as a measure of adequate conditions for endotracheal intubation. We also determined TOF at this point.
3. Methods
This single center, randomized, double-blind study was conducted on 60 ASA physical status I or II patients aged 18 - 60 years scheduled for elective surgeries with a duration of more than 30 min. The exclusion criteria included patient refusal, BMI of ≥ 28, any neuromuscular disease, pregnancy, predicted difficult airway (mouth opening < 3 cm, restricted neck movement, or Mallampati grade III or IV), a history of liver or renal disease, alcohol or drug abuse, gastric esophageal reflux disease, high blood pressure, the use of beta-blocking agents, and hypersensitivity to any of the drugs used in the study. Patients who required the laryngoscopic time of ≥ 15 seconds were also excluded from the study.
We randomized 60 surgical patients scheduled for routine surgery into two groups of 30 patients each, with the help of a random number table and an anesthetist not involved at any stage of the study. All patients were premedicated with ranitidine tablets a day before and in the morning on the day of surgery. In the operating room, an intravenous line was secured and infusion of a balanced salt solution started. Standard anesthesia monitors were attached.
In order to monitor RE and SE, a disposable entropy sensor (EntropyTM Module, Datex Ohmeda Inc, Wisconsin, USA) was attached on the forehead after degreasing by rubbing it with alcohol. The central electrode was placed in the midline, 2 cm above the eyebrows, and the lateral electrode was placed 2 cm lateral to the outer canthus of the left eye, as recommended by the manufacturer.
The neuromuscular monitoring was done by a kinemyograph (Datex-Ohmeda Mechano Sensor NMT device, Datex Ohmeda Inc, Wisconsin, USA) at the wrist of the dominant hand. After degreasing with alcohol, Ag/AgCl ECG electrodes were placed along the medial aspect of the distal forearm, approximately 2 cm proximal to the proximal wrist skin crease with the negative electrode distal and the distance between the two electrodes of less than 6 cm.
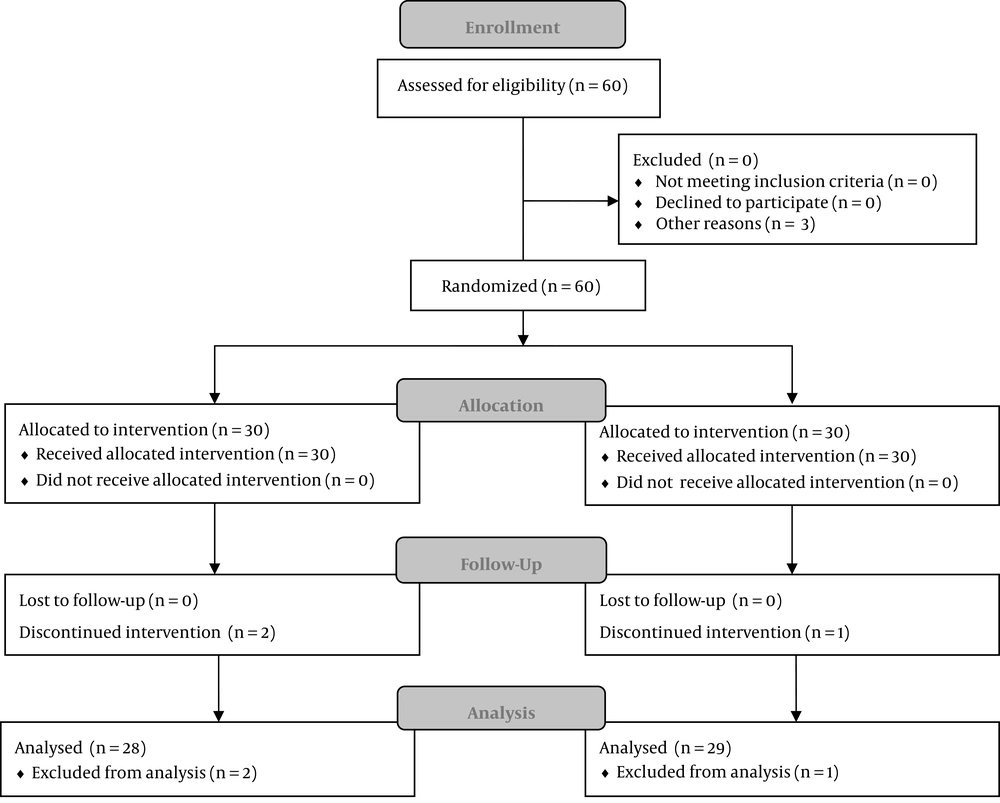
The supervising anesthesiologist allocated the groups and commenced induction. In both the groups, anesthesia was induced with intravenous fentanyl 3 μg/kg after one minute of which, propofol 2 mg/kg was administered over 30 seconds. A stopwatch was started at the onset of propofol injection. Patients were mask ventilated by the intubating anesthesiologist. The neuromuscular blockade was established with intravenous 0.1 mg/kg vecuronium. The supervising anesthesiologist asked the intubating anesthesiologist (an experienced anesthesiologist with more than two years of experience) to intubate at following endpoints. In group entropy (E), intubation was performed when SE dropped from 91 to 45 and RE-SE ≤ 2. In group TOF (T), intubation was performed when TOF came down to 0 (Figure 1).
The monitor with modules of both entropy and TOF was kept on a separate trolley away from the intubating anesthesiologist. Though the electrodes of both entropy and TOF could be seen by the intubating anesthesiologist, the values were hidden to ensure blinding. In both groups, at the time of endotracheal intubation, if the patient had a hypertensive response (> 20% of baseline MAP) or moved in response to intubation, a propofol bolus (20 mg) was injected and repeated if necessary. Additionally, in group E, if SE increased to ≥ 60 before intubation, a propofol bolus was given. SE values were not considered for giving propofol boluses in group T.
The intubating anesthesiologist graded the intubating conditions of jaw and larynx as adequate or inadequate (10). Patient’s movement or coughing was assessed by the intubating anesthesiologist as present or absent. Other parameters noted were SE, TOF, HR, and MAP at baseline, intubation, and 30 seconds postintubation. If given, any propofol bolus was also noted.
The primary outcome was to determine intubating conditions achieved at SE ≤ 45. The secondary outcome was to determine the time taken to achieve this point and the value of TOF (adductor pollicis) at this point.
Though there are a number of studies that have determined the intubating time according to TOF = 0, no studies have used entropy criteria to intubate. Thus, to determine the adequate sample size for intubation using entropy criteria, we required to perform a pilot study. A pilot study with six patients was conducted to estimate the sample size. The time taken to meet the intubating conditions was 110 ± 15 seconds by the entropy method that was lower than the time needed for the TOF group. Therefore, the calculation showed that 21 patients were required in each group for this difference to be significant at a 95% confidence interval, with α of 0.05 and β error of 0.80.
The two-tailed students’ t test was used for between-group differences (concerning time to intubation, RE, SE, HR, and MAP). The paired t test was used for within-group changes in HR, MAP, RE, and SE before and after intubation. Categorical variables (coughing, bucking, and movement on intubation) were compared with the chi-square test. The difference between groups was considered significant if the P value was < 0.05.
4. Results
In this study, 60 patients were recruited and randomized according to the protocol. The patients’ characteristics were comparable in the two groups. Although the difference in the mean patients’ weight was statistically significant between the two groups (P < 0.05), it was not clinically significant (Table 1).
Two patients in group E and one patient in group T were excluded from the study at the time of intubation. One patient in group E was excluded because the intubation criteria were not met until after five minutes of giving the muscle relaxant. The second patient in group E was excluded because of an unanticipated difficult airway that required two attempts at laryngoscopy, with a laryngoscopic time of more than 45 s. The excluded patient of group T did not meet the intubation criteria for 10 minutes. Thus, a total of 57 patients were analyzed for the final results (Figure 1).
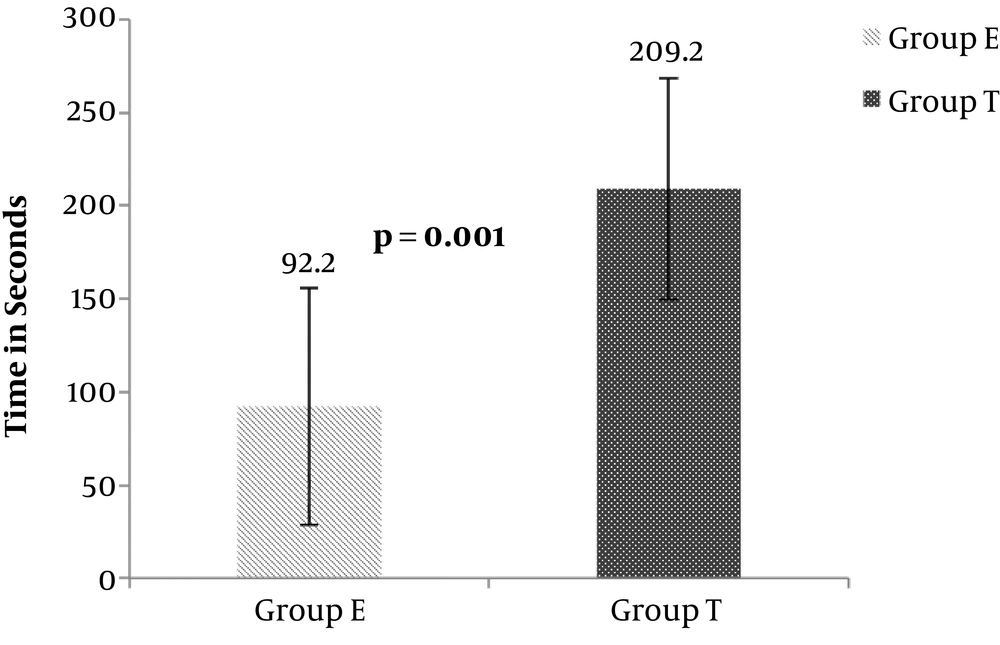
The time to intubation was significantly shorter in group E than in group T (mean: 92.5 ± 63.5 s, 95% confidence interval (CI): 68.9 - 116.0 vs. mean: 209.2 ± 59.6 s, 95% CI: 187.5 - 230.9; P < 0.001) (Figure 1). The mean TOF was 87.3 ± 8.4 at the time of intubation in group E (Figure 2).
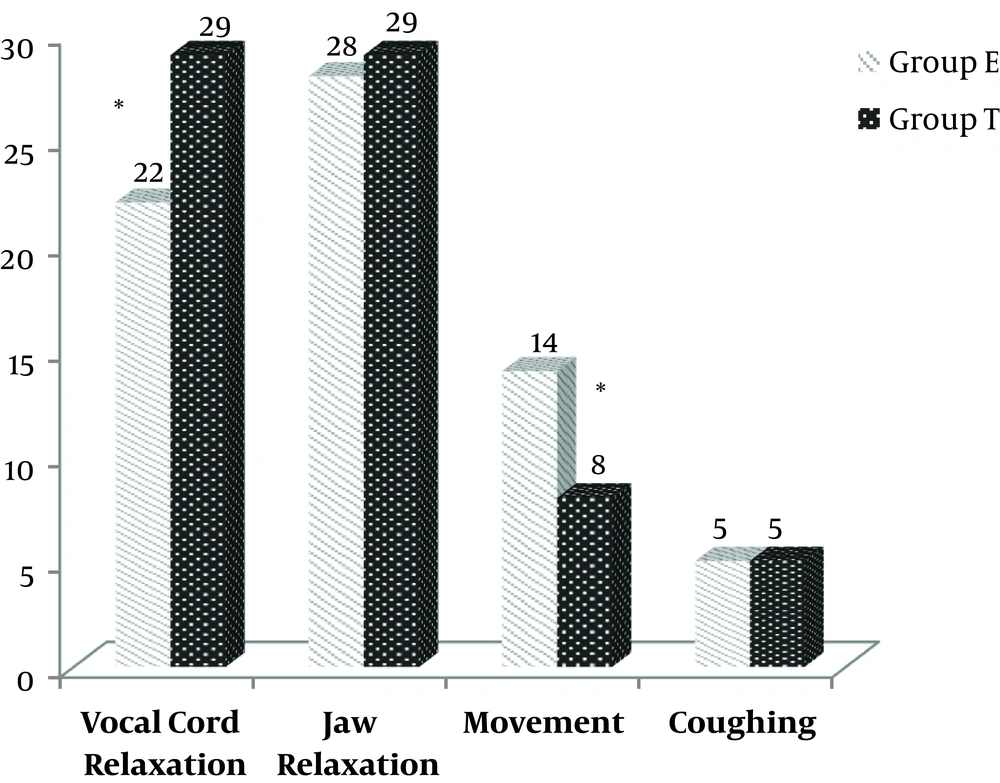
Intubating conditions concerning jaw relaxation, patient movement, coughing, and bronchospasm were not significantly different between the groups. Vocal cord relaxation was significantly inadequate in six patients in group E (P < 0.01). However, no patient had adducted vocal cords and none had difficulty in introducing the endotracheal tube into the trachea. No patient in group T had inadequate vocal cord relaxation (Figure 3). Five patients in each group coughed and moved at endotracheal intubation and required propofol boluses.
In group T, the RE and SE values were significantly higher at intubation and 30 seconds postintubation than group E (P < 0.01). Heart rate and MAP were significantly higher in group E than in group T; however, both groups were comparable at 30 seconds postintubation. At five minutes postintubation, RE and MAP were significantly higher in group T than in group E (P < 0.01). All other parameters were comparable between the groups (Table 2).
| Time | RE | SE | HR, bpm | MAP, mmHg |
|---|---|---|---|---|
| Baseline (E) | 97.3 ± 1.5 | 88.4 ± 2.0 | 86.7 ± 17.5 | 133.7 ± 12.1 |
| Baseline (T) | 96.9 ± 1.7 | 87.4 ± 1.9 | 85.2 ± 14.0 | 134.0 ± 15.2 |
| Intubation (E) | 40.4 ± 12.8 | 38.6 ± 12.9 | 82.2 ± 14.1b | 117.0 ± 13.7b |
| Intubation (T) | 50.7 ± 14.1b | 48.5 ± 13.4b | 73.6 ± 12.5 | 102.9 ± 12.2 |
| 30 seconds post intubation (E) | 46.6 ± 16.5 | 44.6 ± 15.2 | 82.8 ± 9.2 | 110.0 ± 12.1 |
| 30 seconds post intubation (T) | 61.7 ± 11.8b | 59.1 ± 10.8b | 83.7 ± 15.9 | 111.3 ± 15.9 |
| 5 minutes post intubation (E) | 38.9 ± 8.8 | 46.3 ± 9.0 | 82.0 ± 12.1 | 99.8 ± 14.6 |
| 5 minutes post intubation (T) | 46.3 ± 10.2b | 45.2 ± 9.7 | 82.1 ± 10.1 | 111.9 [ ± 10.8]b |
Abbreviations: (E), Group E; HR, Heart rate; MAP, Mean arterial pressure; RE, Response Entropy, SE, State Entropy, (T), Group.
a RE and SE were significantly higher in group T than in group E at intubation and 30 seconds postintubation; RE was significantly higher at 5 minutes postintubation in group T. Heart rate and MAP were significantly higher in group E than in group T at intubation. MAP was significantly higher in group E than in group T at five minutes postintubation.
b Significant at P value < 0.05.
There were no complications in group E. However, one patient in group T had bronchospasm resolved with salbutamol puffs).
5. Discussion
At the time of anesthesia induction with propofol 2 mg/kg and fentanyl 3 µ/kg, it took 90 seconds to reach adequate conditions for tracheal intubation when guided by RE-SE ≤ 2 with SE ≤ 45, which occurred 117 seconds earlier than when guided by TOF = 0 with similar drugs for induction. When guided by entropy, there was a transient increase in HR and MAP at intubation, which decreased to non-significant values at 30 seconds postintubation. The mean TOF was 0.87 at RE-SE ≤ 2 with SE < 45.
In our study, one patient in each group did not meet the intubation criteria according to the study protocol. Similarly, in the study by Lee et al. (9), eight patients were excluded as the neuromuscular blockade was incomplete even five minutes after injecting rocuronium 0.6 mg/kg, which was attributed to individual variations in the pharmacokinetics and pharmacodynamics of the drug.
In group E, the TOF was 0.87 at the time of intubation in adductor pollicis. The central muscles of laryngeal adductors are paralyzed earlier than the peripheral muscles of adductor pollicis (8-12); thus, it is likely that the central muscles were more densely blocked than the peripheral muscles during the endotracheal intubation in the present study. However, as 22% of the patients had inadequate vocal cord relaxation in group E, laryngeal muscles were most probably not completely paralyzed. Various studies have demonstrated that endotracheal intubation can be performed by avoiding muscle relaxants by using higher alveolar concentrations of anesthetic agents, propofol boluses, esmolol, remifentanil infusion, and lignocaine boluses (13-17). However, for this adequate levels of anesthesia should be present as an inadequate level of anesthesia may result in trauma to the airway or result in inadequate ventilation (13, 14). Thus, the present study determined that the point after anesthesia induction when nociception was adequate for endotracheal intubation so that endotracheal intubation could be performed smoothly even when laryngeal muscle paralysis was most probably incomplete.
The value of RE-SE has been the focus of various studies, with some concluding that the decreasing values, i.e. RE-SE ≤ 2, represent nociception and some inferring that this decrease occurs only with increasing neuromuscular blockade (5, 7). Based on the present study, we are unable to comment on the contribution of nociception and neuromuscular blockade individually to the decreasing value of RE-SE. However, the study determined the earliest safe point at which endotracheal intubation could be performed with adequate nociception under optimal conditions of the central muscles of the larynx, but possibly with incomplete laryngeal paralysis. This would be useful in patients where succinylcholine is contraindicated, as well as in full stomach patients and at centers wherein sugammadex is not available.
In the present study, the number of patients who coughed was equal in both groups in spite of the fact that endotracheal intubation was much later in group T than in group E (later by 110 seconds). The possible explanation could be that in group E, even though SE was in the hypnosis range (40 - 60), the analgesia was not at peak (note that the effect of fentanyl takes three minutes to reach the peak while intubation was carried out for almost two minutes). In group T, when TOF = 0 at the time of intubation (3½ minutes), hypnosis was probably wearing off due to weaning off of propofol action by the time endotracheal intubation was performed. Bronchospasm in one patient in this group could be the result of inadequate hypnosis at this point.
The higher SE in group T at intubation could be due to the concern about awareness; however, it never exceeded 65 and thus, awareness seemed unlikely (4).
No patients at a routine follow-up complained of sore throat and hoarseness though this was not formally analyzed. This remains a limitation of this study. The patients’ mean weight was statistically different between the groups; however, weight measures did not exceed 63 kg in any group.
Though the values of entropy and TOF on monitors were kept hidden from the intubating anesthesiologist, the time to ask to intubate was strikingly shorter when guided by entropy than when guided by TOF, which could have been a source of bias when assessing the intubating conditions. Further studies could determine the central laryngeal paralysis by central muscle monitoring to compare with peripheral muscle paralysis.
This study demonstrated that the balance of hypnosis, muscle relaxation, and analgesia to perform intubation can be achieved at RE-SE ≤ 2, SE ≤ 45, 90 seconds after the administration of fentanyl (3 µ/kg), propofol (2 mg/kg), and vecuronium (0.1 mg/kg).
5.1. Conclusions
Adequate conditions for endotracheal intubation are achieved 90 seconds after anesthesia induction with the administration of fentanyl, propofol, and vecuronium when it is guided by RE-SE ≤ 2 with SE ≤ 45, which is earlier than when guided by TOF = 0.