1. Background
Sleep is one of the vital behavioral and psychological processes for the proper functioning of humans. Overnight sleep affects an individual’s mood and emotional responses during the day, and daytime activity affects the quality of sleep at night (1). Sleep disorders, with insomnia on the top, are highly prevalent in different societies and are more common in females (2, 3). The main symptoms of insomnia include dissatisfaction with the quantity and quality of sleep together with complaints of difficulty in sleep onset or maintenance (2). Sleep disorder may occur in the course of another psychological disorder or medical disease or may develop independently (3). Transient and short-term insomnia usually affects 30% - 50% of people. The incidence of chronic insomnia in industrial societies is estimated at 5% - 10%. Chronic insomnia intensifies nervousness and mood disorders, especially depression, and it increases the risk of cardiovascular disease and hypertension (4).
The consequences of insomnia and other sleep disorders are far more than imagined. Individuals with insomnia spend their nights badly due to sleep problems, and they also experience sleepiness and fatigue the next day as well as sharp drops in efficiency and energy. This results in a declined quality of their lives (5). Moreover, sleepiness can affect the patient’s family, colleagues, and the community where she/he lives in (4).
Drug therapy is the best-known treatment for insomnia. However, the long-lasting side effects of soporific and sedative drugs, as well as short-term side effects such as confusion and reduced accuracy shortly after taking medication encourage people towards complementary and alternative medicine (5).
In recent years, several studies investigated the efficacy of Persian medicine (PM) therapies in a variety of diseases, including digestive problems (e.g. constipation, irritable bowel syndrome, and dyspepsia) and gynecological diseases (e.g. abnormal menstrual bleeding and infertility) (6-10). Patients’ satisfaction with PM therapies was the focus of several studies. Nevertheless, research on satisfaction with the effect of PM therapies on insomnia is still a gap.
The slow and time-consuming trend of research and the lack of evaluation systems for the side effects of the PM-associated therapeutic approaches can jeopardize the efforts of scholars and experts in this field during these years. Determination of the patients’ satisfaction with the efficacy of these therapies can play an important role in describing the current status of PM efficacy in the community (11, 12).
The PM healthcare clinics throughout the country are the first treatment centers where the patients are provided with PM services to prevent and treat diseases. The increased patient satisfaction with these services contributes to their motivation to accept and comply with treatments and also plays a significant role in the promotion, growth, and development of PM healthcare clinics.
2. Objectives
The current study aimed at investigating satisfaction with PM therapies among patients with insomnia referring to PM healthcare clinics.
3. Methods
The current descriptive-analytical, cross-sectional study was performed in the PM Healthcare Clinic affiliated to Iran University of Medical Sciences in a nine-month period from 24 June 2017 to 3 December 2017. A total of 100 patients with sleep problems were selected based on the inclusion criteria: age above 18 years, literacy, and insomnia. Individuals with a history of mental disorders and use of sleeping medications were excluded.
In the current study, the patients referring to the PM Healthcare Clinic were visited routinely by PM specialists irrespective of their complaint. They were questioned about a set of criteria, including sleep status as specified on the PM medical history sheet. Subsequently, the patients underwent necessary examinations and received proper treatment.
At this stage, eligible patients with sleep difficulty were introduced to the researcher. After explaining the study objectives to the subjects and receiving their signed written informed consent, they were asked to complete the insomnia severity index (ISI). After a month, when the participants had their second visit at the healthcare clinic, the ISI and the patient satisfaction questionnaire were completed by them.
The ISI is a self-report index measuring an individual’s perception of his/her own insomnia. The index consists of five items comprising of the severity of sleep problems, interference of sleep difficulties with daytime functioning, noticeability of sleep problems by others, and distress caused by sleep difficulties. The validity and reliability of the Persian version of the ISI were confirmed by the Sleep Research Center affiliated to Tehran University of Medical Sciences (13).
A questionnaire was developed to assess the treatment satisfaction in patients referring to the PM Healthcare Clinic. The questionnaire initially consisted of 22 items in four domains: efficacy, convenience and appropriateness, complications, and overall view on PM therapies. The questionnaire was designed by reviewing similar questionnaires in the literature and applying the comments of PM faculty members. The items were scored based on a five-point Likert scale from completely disagree (scored 0) to completely agree (scored 4). To evaluate the validity of the questionnaire, 10 experts of the field were approached, and CVI (content validity index) and CVR (content validity ratio) were computed. After removing the items with a CVR below 0.6, a total of 16 items remained. The CVIs calculated for the efficacy, convenience, complications, overall view, and the total questionnaire were 0.87, 0.9, 0.8, 0.92, and 0.87, respectively. Concerning the internal consistency, the Cronbach’s alpha was 0.89, 0.88, 0.78, 0.76, and 0.92 for efficacy, convenience, complications, overall view, and the total questionnaire, respectively.
Data were analyzed with SPSS software version 17 and expressed as mean, standard deviation, and frequency. The Wilcoxon signed-rank test was used to compare changes in the scores of insomnia symptoms and ISI items before and after the treatment. Satisfaction with the treatment was reported in terms of the number and frequency of patients for the domains of efficacy, convenience, complications, and overall view. The association between satisfaction in the four domains and demographic characteristics such as age, gender, level of education, and marital status was investigated using chi-square test and Spearman correlation coefficient. The relationship between changes in response to the ISI before and after the treatment and different domains of treatment satisfaction was investigated by Spearman correlation test. The significance level in all tests was set at P < 0.05.
4. Results
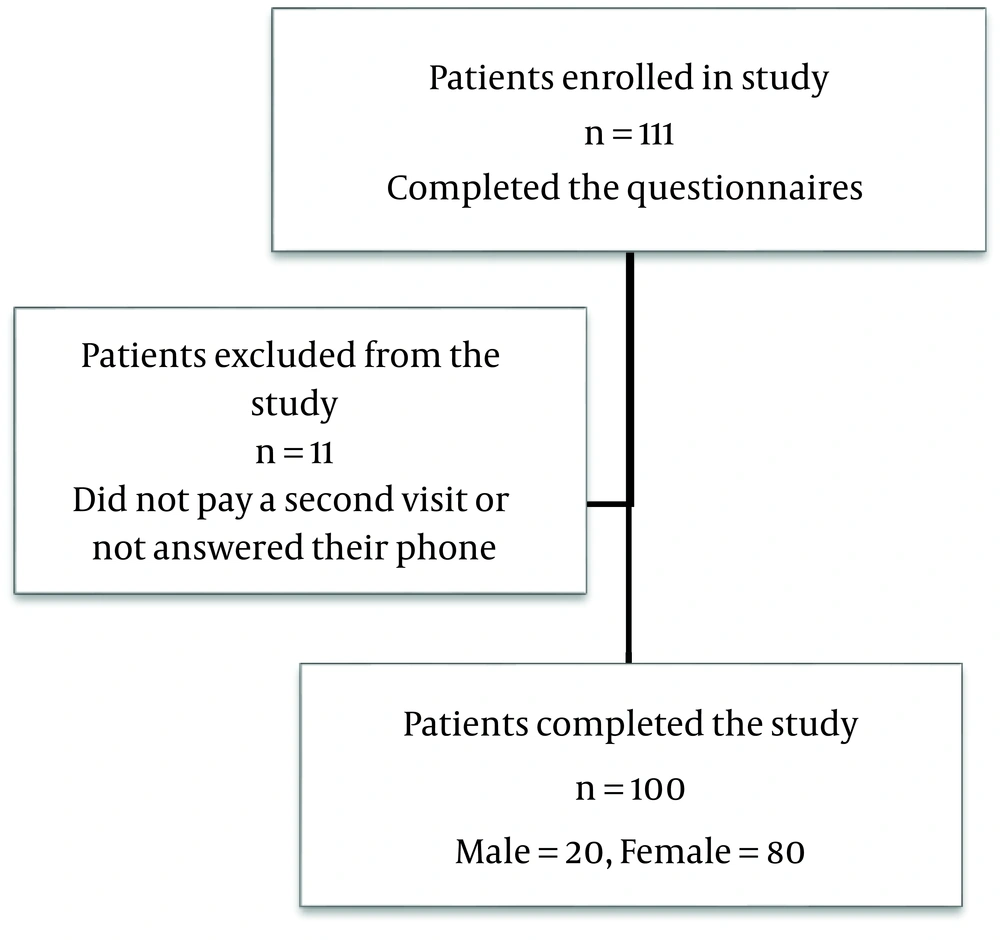
In the current study, the questionnaires were completed by 111 patients referring to the PM Healthcare Clinic affiliated to Iran University of Medical Sciences. One month after the first visit, the patients personally completed the questionnaire for the second time. However, 11 patients were excluded from the study since they did not pay a second visit or not answered their phone. Therefore, 100 patients, including 80 females and 20 males, were finally included in the study (Figure 1).
The mean age of the subjects was 40.06 ± 11.12 years (age range: 18 - 63). In terms of the level of education, 25 had primary or secondary education, 31 had a high-school diploma or associate degree, 26 had a bachelor’s degree, and 15 had M.Sc. degree or Ph.D. Three individuals did not specify their education level. Moreover, 20% were single, 75% married, and 5% widowed or divorced.
As stated, the ISI has five main items about the type of sleep disorder and its impact on the quality of life, with the first item covering three sub-items, including the severity of sleep problem, sleep maintenance, and awakening earlier than usual. This index was completed by patients before and after the treatment. The frequency of response to each item and the P value for the Wilcoxon non-parametric test used to compare baseline and end-of-study results are presented in Table 1. It should be noted that since the number of participants in the study was 100, the frequency reported is equivalent to the frequency percentage.
| Item, Measurement Time | Frequency | Z Value | P Value | |||||
|---|---|---|---|---|---|---|---|---|
| No Problem | Mild | Moderate | Severe | Very Severe | Missing | |||
| Sleep onset | -5.9 | < 0.001 | ||||||
| Before | 5 | 8 | 44 | 30 | 13 | 0 | ||
| After | 22 | 23 | 36 | 15 | 4 | 0 | ||
| Sleep maintenance | -2.8 | 0.004 | ||||||
| Before | 13 | 18 | 37 | 22 | 8 | 2 | ||
| After | 21 | 27 | 34 | 14 | 4 | 0 | ||
| Early morning wakening problems | -3.2 | < 0.001 | ||||||
| Before | 18 | 18 | 26 | 28 | 9 | 1 | ||
| After | 35 | 14 | 26 | 21 | 4 | |||
| Sleep dissatisfaction | -5.6 | < 0.001 | ||||||
| Before | 8 | 3 | 16 | 13 | 59 | 1 | ||
| After | 11 | 10 | 52 | 14 | 12 | 1 | ||
| Interference of sleep difficulties with daytime functioning | -4.8 | < 0.001 | ||||||
| Before | 1 | 5 | 32 | 37 | 25 | 0 | ||
| After | 11 | 20 | 27 | 28 | 14 | 0 | ||
| Noticeability of sleep problems by others | -1.03 | 0.3 | ||||||
| Before | 12 | 25 | 31 | 17 | 14 | 1 | ||
| After | 19 | 25 | 24 | 17 | 15 | 0 | ||
| Distress caused by the sleep difficulties | -4.2 | < 0.001 | ||||||
| Before | 5 | 12 | 33 | 31 | 19 | 0 | ||
| After | 8 | 30 | 28 | 25 | 9 | 0 | ||
The total mean score of the participants for the ISI was 16.49 ± 3.87 at baseline and 12.53 ± 4.59 at the end of the study. Regarding the normal distribution of these two measurements based on the Kolmogorov-Smirnov test, they were compared by Paired Samples t-test, which showed a significant statistical difference between them (P < 0.001) (Table 1).
According to Table 1, the difference in responses to all questions before and after the treatment was statistically significant, except for the 4th question, which was about the noticeability of sleep problems by others. Therefore, it can be concluded that the situation improved and the intervention was effective. The results of the treatment satisfaction questionnaire are shown in Table 2.
| Domain | Totally Disagree | Disagree | No Comment | Agree |
|---|---|---|---|---|
| Satisfaction of patients with treatment efficacy | 2 | 12 | 10 | 64 |
| Satisfaction with the convenience and appropriateness of treatments | 3 | 19 | 7 | 64 |
| Satisfaction with low number and severity of complications | 0 | 2 | 6 | 77 |
| Overall treatment satisfaction | 0 | 4 | 5 | 57 |
In terms of complications, 81% of the participants did not report any complications using PM therapies, while 19% believed that they experienced complications such as nausea, vomiting, and stomachache. However, most of them stated that the complication had no interference with their functioning or caused no serious problems. Also, satisfaction in the domains of efficacy and convenience of treatment, complications, and overall satisfaction did not significantly correlate with demographic characteristics (age, gender, level of education, and marital status).
The relationship between reduction of insomnia based on the ISI score changed in the two evaluated time points and the four domains of treatment satisfaction were assessed by Spearman correlation coefficient. ISI reduced score (i.e. improvement of sleep status) and increased satisfaction significantly correlated with treatment efficacy (P < 0.001). Moreover, there was a significant association between the unwanted complications of the treatment and better sleep status (P = 0.039).
5. Discussion
According to the results of the current study, the patients referring to the PM Healthcare Clinic were satisfied with the efficacy, convenience, and complications of PM therapies for insomnia. Most of the patients were satisfied with the treatments, including lifestyle modifications, nutritional interventions, medical treatment, and manual therapies, consistent with the results of the studies by Maghsudi et al. and Mahmoudian et al. (11, 12).
Studies in other parts of the world also indicated an increasing tendency toward the use of complementary therapies. For example, 1.6 million US residents take complementary and alternative therapies to treat insomnia or sleep disorders. In a study by Thomley et al., to assess the satisfaction of 104 patients treated with acupuncture, as a complementary and integrative therapy, 62% of the patients were satisfied with the time spent on the treatment (14). In a study conducted from 2013 to 2015, Crocker et al. investigated the experience and satisfaction of patients with the early treatments of integrative therapy at the University of Arizona, and reported that the patients were generally satisfied with the treatment delivered in the center (15). In a clinical trial conducted by Yeung et al., 92.3% of the patients were satisfied with the use of acupressure in reducing sleep disorders (16).
In the current competitive world, client satisfaction is an important factor in promoting the quality of services in healthcare centers (17). Patient satisfaction involves a patient’s overall understanding of the quality of the provided healthcare services, whereby dissatisfaction and shortcomings rely on patients’ comments. Therefore, studies such as the current one are helpful to identify and eliminate the existing problems. The PM has a substantial capacity to prevent and treat diseases and can solve many of the patients’ problems along with conventional medicine. Satisfaction with treatment is one of the important factors in the employment of therapeutic methods that leads to compliance with the treatment (18). Satisfaction with treatment is a subject that recently received much attention and was particularly considered in clinical studies (19, 20).
Hashem-Dabaghian et al. evaluated the degree to which the patients with chronic diseases accepted the PM treatments delivered in PM clinics. They reported low rates of acceptance generally due to the bad taste of the drugs, forgetfulness, inaccessibility, and high cost (21). According to the results of the current study, it seems that the improved shape and taste of Persian medications in recent years was effective in increasing patients’ satisfaction and acceptance.
Also, despite the fact that most of the common treatments have complications, the patients in the current study, similar to that of Farsani et al., did not report any specific complications for the treatments (22).
Also, based on the results of a recent study by Mohammadi et al., patients referring to a PM healthcare clinic were generally satisfied with the treatments and rarely complained about complications (23). The sleep and wakeup plan is a low-cost and efficient measure that can lead to improving health both at the individual and community levels, provided that its principles and rules are observed (24).
One of the limitations of the current study was the small sample size. It is suggested that satisfaction with PM treatments should be evaluated in larger, multicenter studies, and in general as a daily practice in PM clinics. Moreover, given the availability of PM therapeutic procedures and the satisfaction of patients with these treatments, it is recommended to evaluate the efficacy of these procedures via clinical trials.