1. Context
Lumbar spine operations could be performed under general or neuroaxial anesthesia (1, 2). General anesthesia (GA) is the preferred method and used more frequently (3, 4) due to having greater patient acceptance and allowing longer surgical procedures. Anesthesiologists are usually more comfortable with GA as the airways are more secured and safe prior to placing the patient in the prone position (1, 5). Patients usually favor GA due to being completely pain-free during the operation (6). Also, many surgeons may refuse regional anesthesia (RA) mostly due to fear of infection and inability to evaluate neural damage during operation as RA causes sensory and /or motor block (7, 8). Decreased venous pressure resulting from RA may reduce blood loss and improve surgical field, and consequently, shorten surgery time and decrease the comorbidities of prolonged surgical time. A significant advantage of neuroaxial anesthesia is the patient’s ability to self-position and adjust their positioning during operation (1, 6, 9-11), hence avoiding damage to the brachial plexus, pressure necrosis of the face, and innervation of the upper trunk or orbital structures, which may occur in malpositioned patients under GA. However, there are controversies as to the clinical outcomes and cost benefits of each method. Our main objective was to determine the more suitable technique (regional or general anesthesia) for lumbar spine surgery. We also evaluated the duration of surgery, duration of post anesthesia care unit (PACU) stay, duration of hospital stay, and total cost in lumbar spine surgery in published randomized control trials, case-controls, and cohort design studies, without limitation for publication date or language.
2. Methods
2.1. Data Sources
Three major databases (i.e., MEDLINE [PubMed], Embase, and Google scholar) were searched by one of the authors for titles and abstracts using a combination of keywords. We also double checked the bibliography lists of all the related articles to detect articles that might have been missed by electronic searching. The last search was performed before September 2018. This search was undertaken without language and date of publication restrictions. The related literature was presented, graded, and discussed by all the authors. The Preferred Reporting Items for Systematic Review and Meta-analysis (PRISMA) guidelines were used for this systematic review and meta-analysis.
2.2. Search Strategy and Key Terms
The keywords used for our search included: “general anesthesia”, “regional anesthesia”, “spinal anesthesia”, “epidural anesthesia”, “cost”, “hospital stay”, “surgery time”, “post anesthesia care unit time”, and “spine surgery”. Their synonyms or abbreviations were also used as the keywords.
2.3. Study Selection
The analysis was restricted to human studies and no restriction on date, language and geographical location of publication was considered. Additionally, the abstracts of articles were thoroughly checked in order to select the most appropriate studies. Attempts were also made to identify additional articles by searching the reference lists of the studies. Authors were asked for extra details in cases where reports were not presented in the required format for data synthesis. Eventually, EndNote software was used to merge the retrieved citations and eliminate the duplicates.
2.4. Inclusion and Exclusion Criteria
The inclusion criteria were: (1) comparing RA (i.e., spinal or epidural) versus GA (i.e., IV or inhaled) in adult patients and (2) being performed on candidates for lumber spine surgery.
On the other hand, we excluded studies in which the level of spine surgery was not determined. Studies on high-risk patients, pregnant women, children or the elderly, animal studies, case series, and case reports were excluded from the analysis. In addition, we excluded articles that did not have crude data or odds ratio (OR) or had not calculated RR. The search results obtained by each author were compared and the duplicate articles were omitted. Prior to downloading the articles in full text, the final articles were assessed for enrolment first by title then by abstract.
2.5. Data Extraction
Among the selected articles, the data such as study design, author(s)’ name, year of publication, study type, study year, age, age standard deviation (age SD), gender distribution, male: female ratio, quality of assessment, the raw number of RA and GA patients, anesthetic techniques, outcomes related to surgical time, PACU stay duration, length of hospital stay, and cost were extracted independently. Duration of operation was defined as the time from skin incision to the application of surgical dressing. The duration of hospital stay was the number of actual days the patient remained in hospital. Disagreements on the suitability for inclusion of a study were resolved by discussion among the authors.
2.6. Statistical Analysis
In this analysis we utilized STATA (V. 10), and the inverse variance model was used to obtain the overall OR, 95% confidence interval (CI), and test statistic for the relationships. Because duration of surgery, PACU stay, hospital stay and cost are continuous measurements, we used standard mean differences (SMD) as the effect size. Statistical heterogeneity of the studies was assessed by the calculation of τ2 and I2. A random effects model was utilized unless I2 was < 25%, for which a fixed effects model was enforced. Generation of a funnel plot and the Egger and Begg P value permitted the detection of the potential publication bias. In addition, the “trim-and-fill” method was utilized to obtain the estimates of ORs corrected for possible publication bias (metatrim command). Furthermore, publication bias was detected by observing the funnel plot by testing funnel plot asymmetry using Begg and Egger’s tests. P values less than 0.05 were considered statistically significant.
2.7. Quality Assessment
The quality of the included articles was assessed by four independent reviewers using different checklists for assessing all our articles after reading the full text. Jadad scale was used as the randomization guide, and STORBE checklist was employed as a guide for assessing the cohort and cross-sectional studies.
3. Results
After omitting the articles that had a quality assessment score of less than 0.5, 28 articles were included in this systematic review and meta-analysis, seven of which compared the total cost between GA and RA, 18 compared the duration of hospital stay, 16 articles compared the PACU stay time, and 25 articles compared the surgery time.
Of the 34160 literature searches from three databases and manual searching, 28 records were eligible for inclusion in this study. The included articles comprised of 2 case-control studies, 4 cross-sectional designs, 7 cohort studies, and 15 randomized clinical trials. Of the 6387 participants, 2739 cases underwent GA for lumbar spine surgery, on other hand, 3648 cases underwent RA for lumbar spine surgery.
3.1. Included Studies
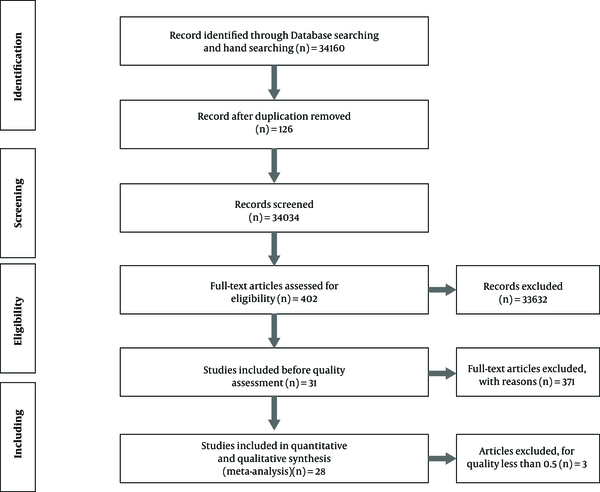
The initial search for studies examining the association between economic outcomes and anesthesia technique (regional or general) yielded 34160 articles (34148 studies from database searching and 12 studies from manual searching). Yet, after reviewing the abstracts and exclusion of the irrelevant and duplicate articles, 402 articles remained in the analysis (Figure 1). Out of the 402 examined articles, 371 were excluded because they did not evaluate our desired variables, considered GA and RA collectively, or did not specify the level of spine surgery. Prior to quality assessment, 31 studies were remained, three of which were excluded due to low quality (< 0.5); therefore, the remaining 28 articles underwent qualitative review and meta-analysis. Figure 1 describes the study design process.
3.2. Cost Comparison in Regional Versus General Anesthesia in Lumbar Spine Surgery
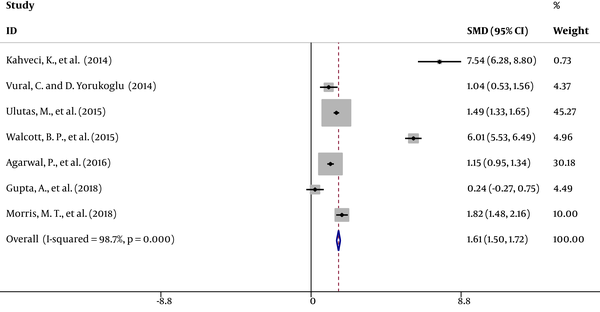
Cost comparison data were available in seven studies (7, 12-17) showing a significant decrease in costs in RA patients compared with GA patients. The results of a random effects model for these seven articles are presented in Figure 2.
The overall SMD with a 95% CI was 1.61 (1.51 to 1.72); z = 29.35; P < 0.001; I2 = 98.7. After meta-analysis and exclusion of the low-quality studies (> 0.5), SMD with a 95% CI was 1.64 (1.53 to 1.75); z = 29.17; P < 0.001; I2 = 98.9. Publication bias was evaluated by a funnel plot.
3.3. Duration of Surgery in Regional Versus General Anesthesia in Lumbar Spine Surgery
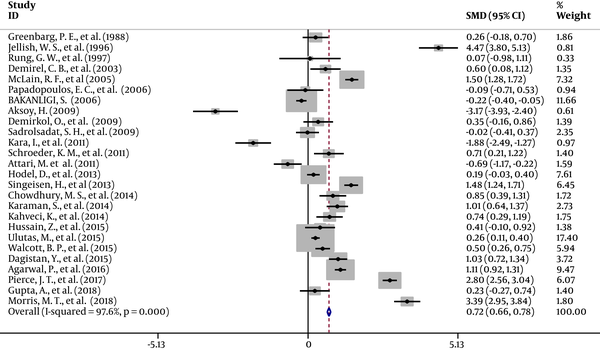
Data on surgery time were available in 25 studies (2, 6, 7, 11-14, 16-33), which showed a significant decrease in the duration of surgery in RA patients compared with GA patients. The results of a random effects model for the 25 studies included in the present meta-analysis are presented in Figure 3. The overall SMD with a 95% CI was 0.72 (0.66 to 0.78); z = 23.52; P < 0.001; I2 = 97.6. After meta-analysis and exclusion of the low-quality studies (lower than 0.5) SMD with a 95% CI was 0.77 (0.71 to -0.84); z = 23.9; P < 0.001; I2 = 97.9.
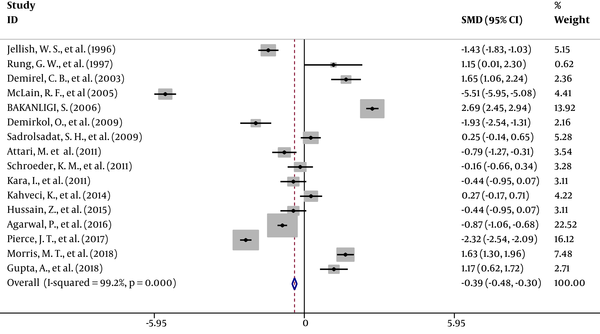
3.4. PACU Stay Time in Regional Versus General Anesthesia in Lumbar Spine Surgery
Data on PACU stay time were available in 16 studies (2, 7, 11, 13, 16-18, 20, 21, 23, 24, 26-28, 32, 34) which revealed a significant increase in the PACU time in RA patients compared with GA patients. The results of a random effects model for the 16 studies are presented in Figure 4. The overall SMD with a 95% CI was -0.39 (0.48 to 0.3); z = 8.47; P < 0.001; I2 = 99.2. After meta-analysis and exclusion of the low-quality studies (< 0.5), SMD with a 95% CI was -0.4 (-0.49 to -0.31); z = 8.65; P < 0.001; I2 = 99.2.
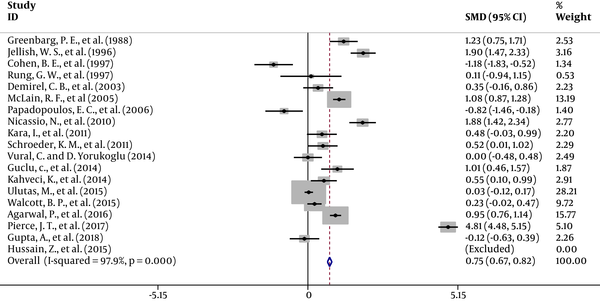
3.5. Hospital Stay Time in Regional Versus General Anesthesia in Lumbar Spine Surgery
Data on hospital stay time were available in 18 studies (2, 7, 11, 12, 14-17, 19-24, 27, 28, 35, 36), which demonestrated a significant decrease in the hospital stay time in RA patients compared with GA patients. The results of a random effects model for the 18 studies included in the present meta-analysis are presented in Figure 5. The overall SMD with a 95% CI was 0.76 (0.67 to 0.82); z = 19.18; P < 0.001; I2 = 97.9. After meta-analysis and exclusion of low-quality studies (lower than 0.5), SMD with a 95% CI was 0.76 (0.68 to 0.84); z = 18.81.; P < 0.001; I2 = 98.3.
3.6. Publication Bias
None of the analyzed studies showed potential publication bias.
4. Discussion
From an economical perspective, our results demonstrated several benefits of RA over GA, such as its significantly lower cost, shorter surgery time, and shorter duration of hospital stay. On the other hand, PACU stay time was longer when using RA.
Seven articles (i.e., 3 RCT, 2 Cohort, 2 cross sectional) compared the cost of RA versus GA and included 968 patients anesthetized by GA and 1080 patients anesthetized by RA. They indicated a significantly lower cost in RA compared with GA (16340 ± 1727 $ vs. 18167 ± 2780 $; Table 1). The mean age of the patients undergoing GA and RA was 52 ± 10 years in both groups, and male/female ratio was 1.1 for GA patients and 1.3 for RA patients.
Eighteen studies showed that hospital stay was significantly shorter in patients anaesthetized by RA (2.2 ± 0.7 days) compared to GA patients (2.6 ± 0.7 days). In these studies, 1606 patients with the average age of 47.6 ± 9 years received GA, while 1937 patients with the average age of 46.7 ± 9 years received RA, and male/female ratio was 1.2 in both groups (Table 1).
Sixteen articles (10 RCTs, 2 Cohorts, 2 cross-sectionals, and 2 case-controls) compared PACU stay time in RA versus GA and included 1363 patients anesthetized by GA and 1596 patients anesthetized by RA. They indicated significantly higher mean PACU stay time in RA compared with GA (101.8 ± 22.4 vs. 87.5 ± 18 minutes). The average age of patients with GA and RA was 47.7 ± 8.4 in both groups, and male/female ratio was 1 for GA patients and 1.3 for RA patients (Table 1).
| Id, Author, Year | Study Type | Assessment Score | n.GA | n. RA | Surgery Time General Anesthesia (GA) | Surgery Time Regional Anesthesia (RA) | PACU Time GA | PACU Time RA | Cost - GA | Cost RA | Hospital Time GA, Hospital Stay Time | RA |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Attari et al., 2011 (18) | RCT | 0.625 | 37 | 35 | 111 ± 7.4 | 115 ± 3.2 | 50 ± 5.9 | 55 ± 6.7 | ||||
| 2. Demirel et al., 2003 (11) | RCT | 0.625 | 30 | 30 | 137.6 ± 26.8 | 118.8 ± 35.4 | 52.9 ± 10.2 | 34.5 ± 12 | 2.92 ± 0.27 | 2.8 ± 0.4 | ||
| 3. Greenbarg et al., 1988 (19) | Case-control | 0.6 | 40 | 40 | 120.3 ± 20.1 | 115.2 ± 19.16 | 5.9 ± 0.98 | 4.8 ± 0.8 | ||||
| 4. Jellish et al., 1996 (2) | RCT | 0.625 | 61 | 61 | 81.5 ± 3.6 | 67.1 ± 2.8 | 80.3 ± 2.8 | 85.4 ± 4.2 | 1.7 ± 0.1 | 1.4 ± 0.2 | ||
| 5. McLain et al., 2005 (20) | Case-control | 0.66 | 200 | 200 | 120 ± 10 | 105 ± 10 | 120 ± 10 | 225 ± 25 | 3 ± 0.319 | 2.75 ± 0.08 | ||
| 6. Rung et al., 1997 (21) | Retrospective-cohort | 0.5 | 7 | 7 | 99 ± 57 | 96 ± 28 | 87 ± 29 | 48 ± 38 | 7.7 ± 5 | 7.2 ± 4.5 | ||
| 7. Papadopoulos et al., 2006 (22) | Cohort | 0.875 | 16 | 27 | 63.6 ± 26.6 | 65.4 ± 15.2 | 1.8 ± 0.3 | 2.1 ± 0.4 | ||||
| 8. McLain et al., 2007 | RCT | 0.375 | 33 | 43 | 144 ± 24.1 | 234 ± 38.6 | ||||||
| 9. Pierce et al., 2017 (23) | Retrospective-Cohort | 0.75 | 183 | 361 | 151.8 ± 25.1 | 97.4 ± 15.8 | 116.5 ± 19.3 | 178 ± 29.5 | 3.1 ± 0.5 | 1.5 ± 0.2 | ||
| 10. Ulutas et al., 2015 (12) | Retrospective cross-sectional | 0.81 | 277 | 573 | 72.9 ± 21.3 | 67.7 ± 19.6 | 54.46 ± 21.81 | 30.89 ± 11.88 | 1.1 ± 0.3 | 1.09 ± 0.38 | ||
| 11. Schroeder et al., 2011 (24) | Retrospective cross-sectional | 0.54 | 83 | 19 | 113 ± 16.5 | 101.9 ± 10.2 | 102.8 ± 64.4 | 113.3 ± 64.4 | 1.287 ± 0.406 | 1.075 ± 0.424 | ||
| 12. Karaman et al., 2014 (25) | Cohort | 0.875 | 34 | 294 | 102.2 ± 44.23 | 77.21 ± 21.62 | ||||||
| 13. Sadrolsadat et al., 2009 (26) | RCT | 0.875 | 50 | 50 | 94.1 ± 17.9 | 94.4 ± 17.3 | 23.8 ± 7.8 | 21.7 ± 8.8 | ||||
| 14. Inci et al., 2011 (27) | RCT | 0.625 | 30 | 30 | 73.6 ± 6.9 | 89.5 ± 9.8 | 92.3 ± 5.7 | 95.8 ± 9.7 | 2.3 ± 1.2 | 1.7 ± 1.3 | ||
| 15. Hussain et al., 2015 (28) | RCT | 0.625 | 30 | 30 | 43.56 ± 9.86 | 40.36 ± 4.88 | 92.3 ± 5.7 | 95.8 ± 9.7 | 2.27 ± 0.45 | 2 ± 0.1 | ||
| 16. Dagistan et al., 2015 (29) | Retrospective, cross-sectional | 0.68 | 90 | 90 | 85 ± 15 | 71 ± 12 | ||||||
| 17. Chowdhury et al., 2010 (6) | RCT | 0.5 | 40 | 40 | 85.05 ± 13.9 | 74.06 ± 11.8 | ||||||
| 18. Morris et al., 2019 (13) | Cohort | 0.875 | 91 | 97 | 100.58 ± 5.18 | 84.98 ± 3.97 | 248.99 ± 26.64 | 214 ± 15.16 | 9285.78 ± 509.57 | 8446.27 ± 411.78 | ||
| 19. Walcott et al., 2015 (14) | Retro-Cohort | 1 | 319 | 81 | 179 ± 39.08 | 159.93 ± 32.75 | 11033 ± 150 | 10000 ± 240 | 2.12 ± 0.07 | 2.02 ± 0.98 | ||
| 20. Gupta et al., 2018 (7) | RCT | 0.75 | 30 | 30 | 118.94 ± 19.6 | 114.4 ± 19.1 | 79.07 ± 12.7 | 65.63 ± 10.1 | 42326 ± 7054 | 40670.37 ± 6741 | 0.482 ± 0.1 | 0.494 ± 0.1 |
| 21. Vural and Yorukoglu, 2014 (15) | RCT | 0.5 | 33 | 33 | 51193 ± 4467 | 47681 ± 1667 | 0.6 ± 0.1 | 0.6 ± 0.1 | ||||
| 22. Hodel et al., 2013 (8) | Cohort | 0.375 | 105 | 361 | 122.2 ± 641.4 | 64.6 ± 68.3 | ||||||
| 23. Agarwal et al., 2016 (16) | Retro-cross sectional | 0.9 | 178 | 326 | 151 ± 64.7 | 98.3 ± 34.6 | 113 ± 70.3 | 177 ± 74.9 | 13206 ± 7249 | 7534 ± 3016 | 3.1 ± 2.5 | 1.5 ± 1 |
| 24. Guclu et al., 2014 (35) | RCT | 0.75 | 28 | 28 | 1.237 ± 0.404 | 0.93 ± 0.141 | ||||||
| 25. Cohen et al., 1997 (36) | RCT | 0.75 | 21 | 21 | 5 ± 0.2 | 5.3 ± 0.3 | ||||||
| 26. Demirkol et al., 2009 (30) | RCT | 0.625 | 30 | 30 | 71.8 ± 20.1 | 65.2 ± 17.4 | 17.9 ± 6.5 | 48.5 ± 21.5 | ||||
| 27. Kahveci et al., 2014 (17) | RCT | 0.625 | 40 | 40 | 102.05 ± 25.34 | 84.45 ± 22.2 | 20.85 ± 5.2 | 19.55 ± 4.58 | 74.35 ± 9.02 | 22.27 ± 3.74 | 3.1 ± 1.24 | 2.5 ± 0.93 |
| 28. Nicassio et al., 2010 (4) | Cohort | 0.375 | 238 | 23 | 1.8 ± 0.3 | 1.25 ± 0.2 | ||||||
| 29. Aksoy, 2009 (31) | RCT | 0.75 | 30 | 30 | 93.5 ± 10.67 | 133.4 ± 14.27 | ||||||
| 30. Bakanligi, 2006 (32) | RCT | 0.75 | 250 | 250 | 91.09 ± 30.22 | 98.63 ± 36.53 | 45 ± 10 | 20 ± 8.5 | ||||
| 31. Singeisen et al., 2013 (33) | Retrospective cohort | 6.25 | 105 | 368 | 77 ± 17.7 | 56.8 ± 12.3 |
Information About the Articles Included in Our Systematic Review That Shows the Four Variables of Cost, Surgery Time, Post-Anesthesia Care Unit (PACU) Time, Duration of Hospital Staya
Comparison of the surgery time analysis in regional versus general anesthesia in 25 articles (i.e., 12 RCTs, 8 Cohorts, 4 cross-sectionals, and 2 case-controls), which included 2386 patients anesthetized by GA and 3500 patients anesthetized by RA, indicated a significant reduction in the mean surgery time in RA (90.6 ± 19) compared to GA (102 ± 22).
The mean age of the patients with GA and RA was 47.5 ± 10 years in both groups, and male/female ratio was 1.2 for GA patients and 1.3 for RA patients (Table 1). We observed significant heterogeneity in the meta-analysis of continuous variables, which could be due to the different tools used for evaluating continuous variables in the studies included. For example, the heterogeneity in PACU time is a probable consequence of the difference in discharge criteria, our results were basically limited to the comparison of RA versus GA. In addition, there were a number of variables (e.g., postoperative hemodynamic data) that could not be included in the meta-analysis due to insuffcient data or significant inconsistencies in the measurements between the studies. In summary, the results of this study support RA as an optimal anesthesia method for lumbar spine surgery for reducing the cost of surgery. The most important findings of this meta-analysis are the significant association of RA with lower costs, shorter surgery time, and shorter duration of hospital stay. Attari et al. (18) demonstrated that RA may be a more desirable choice relative to GA. RA decreased blood loss, systolic pressure and heart rate changes, and postoperative analgesic requirement. In addition, surgeon and patient satisfaction was significantly more in RA. These findings corroborate our findings as to the shorter duration of hospital stay and shorter surgical time, and thereby, significant reduction in cost of surgery.
Chowdhury et al. (6) compared spinal and general anesthesia in patients undergoing only one-level lumbar operations. They found that spinal anesthesia (SA) offered more desirable operating conditions, effective postoperative pain control, and faster discharge when compared with GA for single-level lumbar spine surgery. This finding is in line with the better economic outcomes found in our meta-analysis.
Dagistan et al. (29) compared the reliability and benefit of spinal anesthesia with GA in patients undergoing lumbar microdiscectomy (LM). The anesthetic durations were longer in the GA group and there was less intra-operative bleeding in the SA group. These differences during surgery may also shorten the surgical time, supporting better economic outcomes in RA.
Demirel et al. (11) evaluated the advantages of both GA and RA techniques in lumbar laminectomy and discectomy. Surgical time (118.80 ± 35.42 vs. 139.60 ± 26.80 minutes) and PACU stay time were longer in the GA group. There was no difference in hospital stay time between the two groups. Gupta et al. (7) studied 60 patients randomly assigned to receive either GA or SA. The results showed that SA was a more desirable, safe, and economical substitute for GA for lower spinal surgery.
Hodel et al. (8) proved that regional techniques are more cost-effective compared to GA. Scrutiny of the data revealed that SA caused significantly shorter surgery time (3.9 minutes), preparation time (3.2 minutes), and exit period (10.4 minutes), compared to GA. Anesthesia time with barring the duration of surgery revealed significant time-saving in regional techniques.
Hussain et al. (28) in a randomized controlled trial compared the efficacy of SA with GA for lumbar discectomy. Mean surgery time in the spinal anesthesia group was 62.70 minutes, while it was 90.73 minutes in the GA group (P < 0.001). The mean duration of hospital stay in the SA group was 2.0 days and in GA group it was 2.27 days (P = 0.002). In conclusion, spinal anesthesia is safe and can be used as the routine anesthesia method for most patients undergoing lumbar discectomy.
Morris et al. (13) in a study compared the economic outcomes of both techniques in teaching setups for lumbar laminectomy and microdiscectomy, which showed no remarkable disparity between the teaching and private hospitals. However, the greatest contrast was observed in costs, such that the cost was much higher (18.74%) for GA in both setups. They inferred that the use of regional techniques for lumbar laminectomy spares operation room time, increases the PACU turnovers, reduces the anesthesia time, and lowers pain sources.
Pierce et al. (23) found that with regional technique the duration of operation was remarkably shorter, blood loss was less, total anesthesia period was shorter, the interval between entrance of patient until incision was briefer, also the time for bandage placement till leaving the operation room was shorter. Although the duration of PACU stay was longer, total hospital stay was shorter with RA.
Vural and Yorukoglu (15) in a study compared SA and GA with regards to cost and satisfaction of patients undergoing lumbar disc surgery. They found that hemodynamic parameters, first urination, mobilization time, and post-operative analgesic requirement were similar in both groups. Intra-operative fentanyl administration was less in the SA group. Similarly, the total cost was less in the SA group along with a higher patient satisfaction. They inferred that lumbar spine operations could be accomplished by implementing either anesthesia techniques. With careful selection of patients, SA is considered reasonable and cost-effective.
The above-mentioned studies showed discrepant findings with regards to the selected variables in patients undergoing either techniques of SA or GA. For lumbar spine surgery, some articles have indicated shorter operation time and PACU stay duration and less post-operative nausea and vomiting with the SA technique. Invariably, all the studies demonstrated cost-effectiveness with SA. Heart rate, blood pressure, and analgesic requirement were higher in the GA group both intraoperatively and at PACU. Post-operative nausea and vomiting were remarkably higher during PACU stay in GA groups, while urinary retention occurred more frequently in SA groups. Pulmonary complications occurred more frequently with GA, but the difference was not significant. These findings indicate that compared to GA, RA can curtail the costs of treatment.
4.1. Conclusions
Despite limitations inherent to the presented article, which is dealing with economic aspects of a larger set of studies, the results of this meta-analysis suggest that RA has several advantages over GA with respect to cost, surgery time, and duration of hospital stay in patients undergoing lumbar spine surgery. Decreased PACU stay time was observed in GA technique. Further perfectly designed studies are needed to clarify the benefits of each technique. Also, more high-quality studies performed on larger cohorts with similar characteristics using similar types of drugs and methods can elucidate the discussion. We concluded that RA is more cost-effective and time-saving than GA.