1. Background
Degenerative lumbar spine conditions involve the slow loss of normal structure and function of the spine over time especially in aging (1). In general, symptoms of a degenerating lumbar disc include pain with movement or at rest, limited motion, weakness, bladder and bowel function problems, sensory loss, and sexual dysfunction. These symptoms can negatively affect daily tasks (2). Health-related quality of life (HRQoL) is multidimensional and incorporates domains related to physical, emotional, mental and social functioning. Assessing the health-related quality of life is an important marker for the results of treatment and care interventions (3). Finding the quality of life score in addition to providing proper treatments can be effective in the promotion of therapeutic programs, care, and rehabilitation (4). Further, HRQoL measurement in clinical studies makes a closer relationship between the patient and physician as well as treatment team members. Overall quality of life is a multi-dimensional subject that is affected by the disease and therapeutic interventions (5). Treatment of the lumbar degenerative spinal disease depends on the type and severity of the condition. Surgery may be required in more severe cases involving herniated discs or spinal stenosis. In one study analyzing the health-related quality of life (HRQoL) by (EQ-5D-3L/EQ-VAS (Euro Quality of Life - 5 Dimension - 3 Level/visual analog scale)), Jansson et al. reported that the mean EQ-5D score improved from 0.36 to 0.64, and the HRQoL improved in 80% of the patients (6). Other studies indicated that EQ-5D is increasingly used in spinal research and as an outcome measure in spinal surgery (7-11). However, no studies have reported EQ-5D scores in patients who have undergone surgery for degenerative spine conditions in Iran.
2. Objectives
The aim of this study was to demonstrate related factors with quality of life improvement in patients before, 6 and 12 months after lumbar spine decompression surgery in three tertiary hospitals of Tehran, Iran.
3. Methods
This quasi-experimental research was conducted on 145 patients with lumbar disc degeneration disease who underwent decompression surgery with or without fusion during 2017 - 2018. Inclusion criteria for surgery were neurogenic spinal claudication, reduced muscle strength, intractable pain, and those in whom an appropriate 6 to 12 months non operative course of treatment fails. Patients with a previous history of spinal surgery were excluded from the study. A data collection form including demographic characteristics (age, sex, educational level, life model, smoking, past medical history, duration of pain before surgery,) filled by patients before surgery. One form containing signs and symptoms of patients [leg and back pain scale, regular activity, walking ability (meter) (< 100 m, 100 - 500 m, 501 - 1000 m and over 1000 m)] was completed by the neurosurgeons before, 6 and 12 months after surgery. The type of surgery was also explained (decompression with or without fusion). The EuroQol-5D-3L (EQ-5D) questionnaire as an instrument for measuring health-related quality of life was provided to patients three times; before, 6 and 12 months after neurosurgery. The EQ-5D-3L essentially consists of 2 pages, the EQ-5D descriptive system and the EQ visual analog scale (EQ-VAS). The EQ-5D-3L descriptive system comprises the following 5 dimensions: mobility, self-care, usual activities, pain/discomfort, and anxiety/depression. Each dimension has 3 levels: no problems, moderate problems, extreme problems which were on a scale of 1 to 3. The total score in 5 dimensions was categorized between 5 and 15, in which 5 was the worst (extreme problems) and 15 was the best (no problem) in all dimensions (12). The EQ VAS records the respondent’s self-rated health on a vertical, visual analog scale where the endpoints are labeled “Best imaginable health” (100 scores) and “Worst imaginable health state” (0 scores). This information can be used as a quantitative measure of health outcome as judged by the individual respondents (13). The mean score of QOL/VAS in leg and back pain scales, regular activity scale and walking distance (meters) is estimated. Overall EQ5D is one comprehensive and short questionnaire which only takes 1 to 5 minutes to fill depending on the individual’s condition. Meanwhile, it has been translated into different languages and its reliability and validity have been confirmed (1, 14-16). In this study, all surgeries were performed by three skilled neurosurgeons with at least 10 years of experience in three general and private hospitals. In most cases, patients referred for the follow-up 6 and 12 months after the operation. The quality of life questionnaire (EQ5D/VAS) was completed via phone interview by the researcher. If the patient left the study for any reason (death, travel, etc.), a new eligible case was replaced for beginning the study. All patients completed the informed consent form at the beginning of the study. It was explained to the patients that all information remained confidential and the results of the study will be published only in groups. RCT code registered in irct.ir is 33996. Finally, this study was approved by the Ethics Committee of Shahid Beheshti University of Medical Sciences, Tehran, Iran.
3.1. Statistical Analysis
In this study basic descriptive statistics (demographic, signs, and symptoms), reports of each dimension of the EQ5D questionnaire for 3 times, before, 6 and 12 months after surgery (Tables 1 and 2). For comparison of the three EQ-5D-3L/VAS scores before, 6 and 12 months after surgery, repeated measures ANOVA analysis was used. Post-hoc multiple comparisons for observed means of groups performed. In equal variance assumed, Scheffé test was used. The charts of quality of life (EQ5D) were drawn in three periods based on age, BMI, life model and duration of pain before surgery. Analyzes were performed using the SPSS version 19 software. The statistical significance level P value < 0.05 was considered.
4. Results
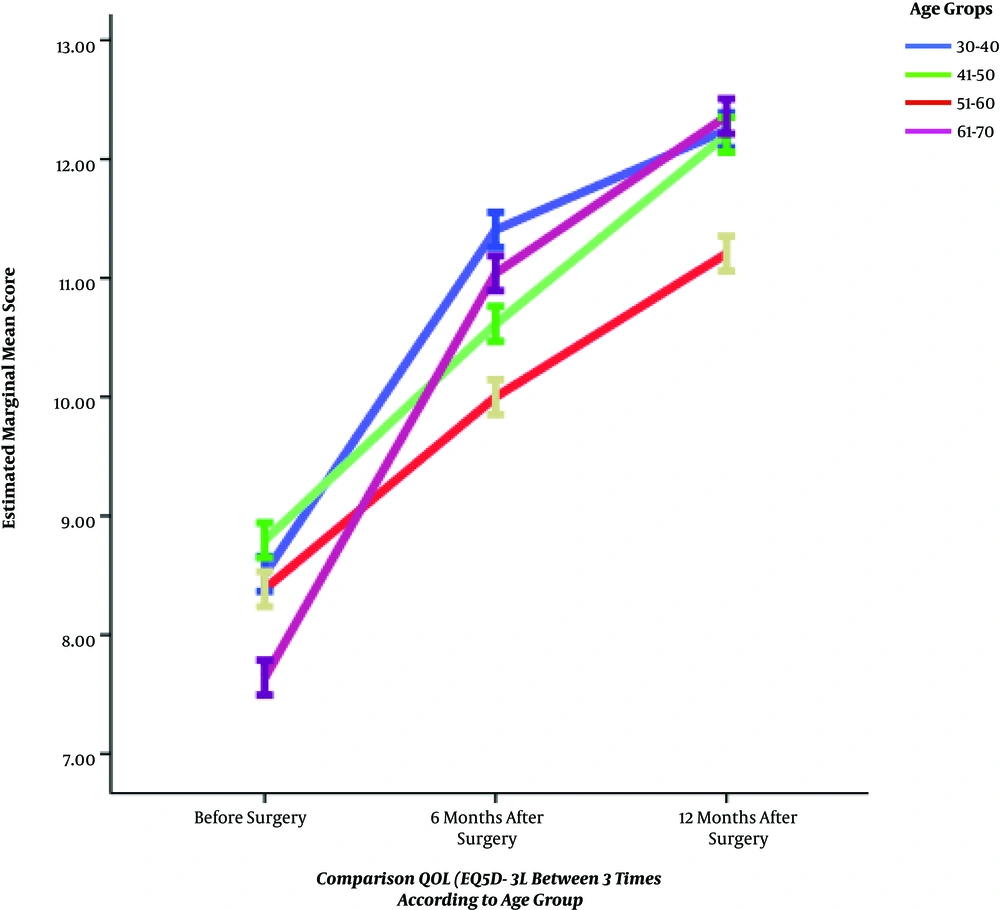
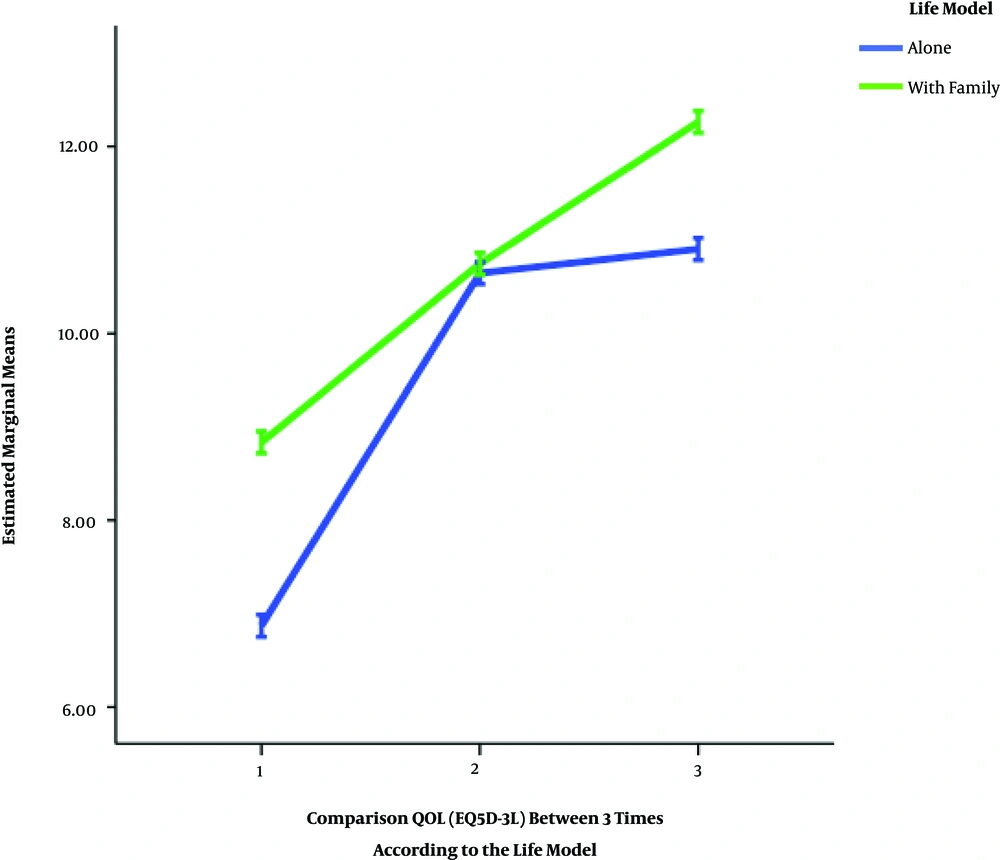
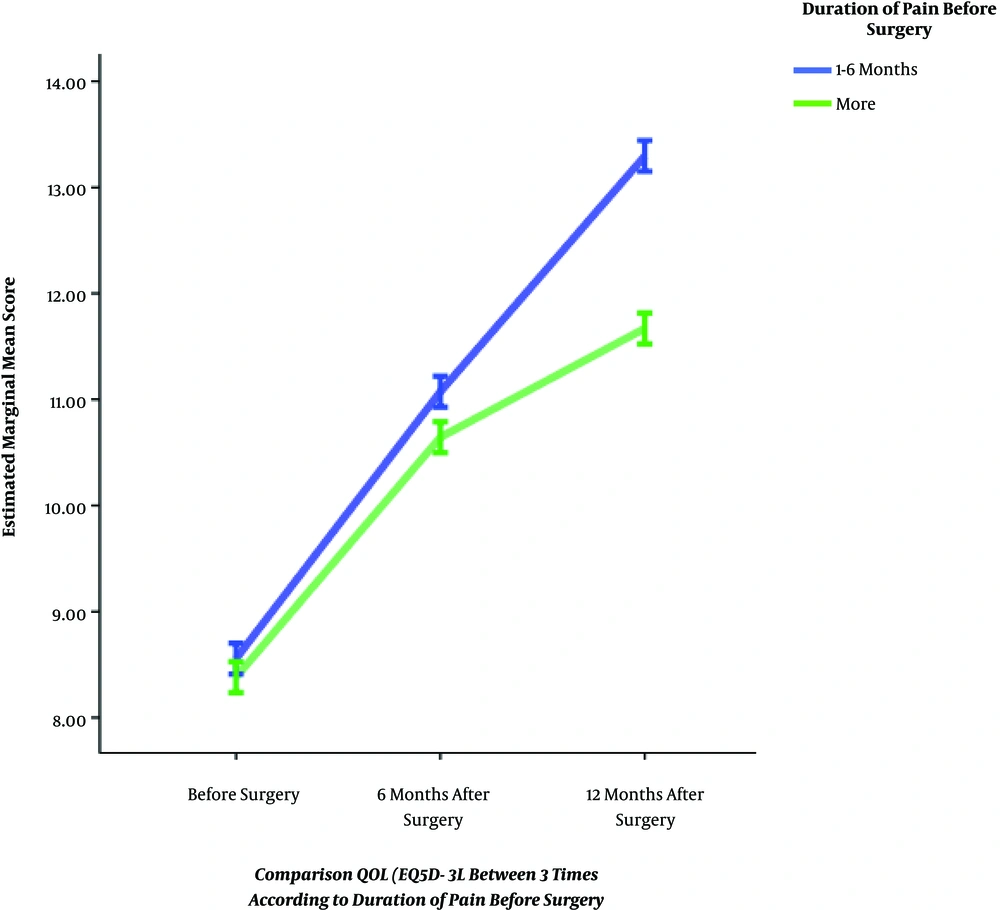
Overall, among 145 patients with lumbar disc degeneration participated in this study, 90 (62.1%) were female. The most patients (30.3%) were in the 41 - 50 years age group. Only 10 (6.8%) patients were not available even by phone 6 or 12 months after surgery who were replaced with other patients for the baseline. All results of the descriptive analysis are presented in Table 1. A detailed analysis of the 5 dimensions of the EQ-5D comparing the severity of problems at the three times are demonstrated in Table 2. Overall, in Repeated Measure ANOVA analysis, there was a significant mean difference in the quality of life promotion in all age groups in before, 6 and 12 months after surgery(P = 0.001). Post hoc analysis indicated there was a significant mean difference of quality of life in 30 - 40 and 51 - 60 years age groups (P = 0.01, 95% CI: 0.12 - 1.58) (Figure 1). In VAS, the highest increased score was in the age group of 30 - 40 years. In post hoc comparison, there was significant mean difference between 30 - 40 and 51 - 60 (P = 0.008, 95% CI: 1.61 - 15.1) also in the 30 - 40 and 61 - 70 years age group (P < 0.001, 95% CI: 5.71 - 20.99). Furthermore, between 41 - 50 and 61 - 70 years age groups significant difference was estimated (P = 0.02, 95% CI: 0.84 - 15.6). In comparison QOL in 3 three times based on BMI subgroups, there was the significant mean difference between normal and overweight (P = 0.01, 95% CI: 0.15 - 1.5) also between overweight and obese (P = 0.006, 95% CI: -0.15 - -0.2). In VAS comparison between BMI subgroups, a significant mean difference between normal and overweight was reported (P = 0.01, 95% CI: 1.46 - 15.62). In all educational level, QOL improved in 3 times (P < 0.001) but significant mean difference was between QOL in illiterates and elementary school (P = 0.03, 95% CI: -2.6 - -0.04) as well as illiterate and university education (P < 0.001, 95%CI: -3.03 - -0.6). In comparison of VAS in educational levels, significant mean difference was between illiterates and elementary (P = 0.04, 95% CI: -20 - -0.13) as well as illiterate and diploma (P = 0.01, 95% CI: -25.9 - -1.47) and university education (P < 0.001, 95% CI: -32.30 - -8.36). Also, in repeated measure ANOVA, the mean of QOL/VAS score in 2 models of life improved in three times significantly (P < 0.001) (Figure 2). Furthermore, there was the mean difference between QOL/VAS score and smoking (P < 0.05), duration of pain before surgery (only QOL/VAS) (P < 0.001, P = 0.001) before, 6 and 12 months after surgery (Figure 3). The mean difference between QOL/VAS and walking distance (meters), leg and back pain level as well as regular activity before, 6 and 12 months after was statistically significant (P < 0.05). We did not find any difference between QOL/VAS and kind of surgery. All the results of comparison between mean EQ-5D-3L/ VAS score in three times, before, 6 and 12 months after surgery are showed in Table 3.
| Variable | Frequency, No. (%) | Variable | Frequency, No. (%) |
|---|---|---|---|
| Gender | Age groups | ||
| Male | 55 (37.9) | 30 - 40 | 37 (25.5) |
| Female | 90 (62.1) | 41 - 50 | 44 (30.3) |
| Educational level | 51 - 60 | 39 (26.9) | |
| Illiterate | 8 (5.5) | 61 - 70 | 25 (17.2) |
| Elementary school | 25 (17.2) | BMI | |
| Middle/high school | 7 (4.8) | 18.5 - 24.9 (normal) | 45 (31) |
| Diploma | 44 (30.3) | 25 - 29.9 (overweight) | 22 (15.2) |
| University education | 61 (42.1) | ≥ 30 (obese) | 78 (53.8) |
| Back pain | Walk | ||
| Before surgery | Before surgery, m | ||
| 1 > | 16(11) | 100 > | 125 (86.2) |
| 1 - 2 | 36(24.8) | 100 - 500 | 20 (13.8) |
| 2 < | 93(64.1) | 6 months after surgery, m | |
| 6 months after surgery | 100 > | 61 (42.1) | |
| 1 > | 45 (31) | 100 - 500 | 81 (55.9) |
| 1 - 2 | 92 (63.4) | 501 - 1000 | 3 (2.1) |
| 2 < | 8 (5.5) | 12 months after surgery, m | |
| 12 months after surgery | 100 > | 4 (2.8) | |
| 1 > | 106 (73.1) | 100 - 500 | 64 (44.1) |
| 1 - 2 | 39 (26.9) | 501 - 1000 | 53 (36.6) |
| 2 < | 93 (64.1) | 1000 < | 24 (16.6) |
| Past medical history | Regular activity | ||
| Diabetes | 3 (21) | Before surgery | |
| HTN | 3 (21) | Yes | 13 (9) |
| DM and HTN | 20 (13.8) | No | 132 (91) |
| Cardiac diseases | 10 (6.9) | 6 months after surgery | |
| Spine fracture | 5 (3.4) | Yes | 63 (43.4) |
| Depression/anxiety | 15 (10.3) | No | 82 (56.6) |
| Osteoporosis | 16 (11) | 12 months after surgery | |
| Combined | 15 (10.3) | Yes | 137 (94.5) |
| None | 58 (40) | No | 8 (5.5) |
| Leg pain | Smoking | ||
| Before surgery | Yes | 28 (19.3) | |
| 1 - 2 | 64 (44.1) | No | 117 (80.7) |
| 2 < | 51 (55.9) | Duration of pain before surgery | |
| 6 months after surgery | 1 - 6 months | 27 (18.6) | |
| 1 > | 16 (11) | > 6 months | 118 (81.4) |
| 1 - 2 | 116 (80) | Type of surgery | |
| 2 < | 13 (9) | Decompression with fusion | 66 (45.5) |
| 12 months after surgery | Decompression without fusion | 79 (54.5) | |
| 1 > | 48 (33.1) | ||
| 1 - 2 | 97 (66.9) |
| EQ-5D-3L Dimension | Before Surgery | 6 Months After Surgery | 12 Months After Surgery |
|---|---|---|---|
| Mobility | |||
| Level 1 | 56 (38.6) | 3 (2.1) | 0 (0) |
| Level 2 | 89 (61.4) | 109 (75.2) | 74 (51) |
| Level 3 | 0 (0) | 33 (22.8) | 71 (49) |
| Self-care | |||
| Level 1 | 78 (53.8) | 3 (2.1) | 0 (0) |
| Level 2 | 67 (46.2) | 137 (94.5) | 119 (82.1) |
| Level 3 | 0 (0) | 5 (3.4) | 26 (17.9) |
| Usual activity | |||
| Level 1 | 72 (49.7) | 3 (2.1) | 0 (0) |
| Level 2 | 73 (50.3) | 136 (93.8) | 119 (82.1) |
| Level 3 | 0 (0) | 6 (4.1) | 26 (17.9) |
| Pain/discomfort | |||
| Level 1 | 64 (44.1) | 139 (95.9) | 0 (0) |
| Level 2 | 81 (55.9) | 6 (4.1) | 67 (46.2) |
| Level 3 | 0 (0) | 0 (0) | 78 (53.8) |
| Anxiety/depression | |||
| Level 1 | 18 (12.4) | 7 (4.8) | 3 (2.1) |
| Level 2 | 78 (53.8) | 64 (44.1) | 66 (45.5) |
| Level 3 | 49 (33.8) | 74 (51) | 76 (52.4) |
aValues are expressed as No. (%).
| Variable | EQ-5D (First) | EQ-5D (Second) | EQ-5D (Third) | P Value | VAS (First) | VAS (Second) | VAS (Third) | P Value |
|---|---|---|---|---|---|---|---|---|
| Age groups | 0.007* | < 0.001* | ||||||
| 30 - 40 | 8.51 (1.44) | 11.40 (0.79) | 12.24 (0.89) | 22.29 (5.60) | 45 (15) | 81.48 (7.53) | ||
| 41 - 50 | 8.79 (2.31) | 10.61 (0.57) | 12.20 (1.47) | 21.93 (8.43) | 42.18 (12.10) | 69.31 (10.65) | ||
| 51 - 60 | 8.38 (1.84) | 10 (1.41) | 11.20 (1.43) | 17.56 (6.05) | 42.48 (26.6) | 63.5 (18.24) | ||
| 61 - 70 | 7.64 (1.94) | 10.72 (1.07) | 12.36 (1.82) | 19.40 (12.18) | 32.92 (16.25) | 56.40 (18.84) | ||
| Gender | 0.3 | 0.4 | ||||||
| Male | 8.29 (2.10) | 10.65 (0.88) | 11.98 (1.56) | 20.09 (7.35) | 39.80 (16.10) | 68.65 (13.30) | ||
| Female | 8.04 (1.88) | 10.57 (0.99) | 11.76 (1.31) | 20.61 (8.73) | 42.35 (20.09) | 69.65 (18.12) | ||
| BMI | 0.001* | 0.01* | ||||||
| 18.5 - 24.9 (normal) | 8.08 (1.56) | 11.15 (0.87) | 12.24 (1) | 20.11 (4.45) | 41 (13.7) | 41 (13.7) | ||
| 25 - 29.9 (over weight) | 7.36 (1.52) | 10.09 (0.61) | 11.97 (1.66) | 18.63 (10.02) | 33.13 (12.62) | 33.13 (12.62) | ||
| ≤ 30 (obese) | 8.89 (2.12) | 10.65 (1.18) | 11.97 (1.40) | 21.08 (9.28) | 43.93 (21.78) | 43.93 (21.78) | ||
| Educational level | < 0.001* | < 0.001* | ||||||
| Illiterate | 6.25 (0.70) | 8.2 (0.01) | 10.10 (0.55) | 10 (0) | 21.25 (3.53) | 25.50 (15.81) | ||
| Elementary school | 6.30 (1.18) | 9.72 (0.54) | 11.52 (1.80) | 23.40 (13.21) | 39.16 (18.41) | 64 (20.86) | ||
| Middle/high school | 6.57 (1.27) | 10.57 (0.54) | 11.78 (1.20) | 19.28 (12.05) | 33.85 (15.08) | 67.85 (11.49) | ||
| Diploma | 7.70 (1.77) | 11.18 (1.40) | 12.06 (1.40) | 17.15 (5.84) | 41.59 (25.51) | 66.13 (18) | ||
| University education | 9.54 (1.44) | 11.09 (0.92) | 12.89 (1.56) | 23.03 (4.58) | 45.65 (18.06) | 76.06 (8.76) | ||
| Life model | < 0.001* | < 0.001* | ||||||
| Alone | 6.67 (1.42) | 10.54 (1.70) | 10.77 (1.54) | 14.03 (5.54) | 38.87 (31.19) | 55.16 (17.62) | ||
| With family | 8.53 (1.91) | 10.62 (0.61) | 12.14 (1.23) | 22.14 (7.98) | 42.07 (13.54) | 72.32 (14.09) | ||
| Cigarette smoking | 0.03* | 0.01* | ||||||
| Yes | 7.57 (1.73) | 10.25 (1.37) | 11.57 (1.52) | 20.35 (10.70) | 41.38 (18.66) | 68.65 (16.44) | ||
| No | 8.27 (2.02) | 10.69 (0.80) | 11.91 (1.38) | 20.42 (7.55) | 47.60 (26.22) | 69.28 (21.37) | ||
| Duration of pain before surgery | <0.001* | 0.001* | ||||||
| 1 - 6 months | 8.44 (2.20) | 11 (0.96) | 13.18 (1.27) | 23.51 (12.69) | 42.11 (18.11) | 66.85 (19.66) | ||
| > 6 months | 8.06 (1.91) | 10.51 (0.09) | 11.54 (1.26) | 19.70 (6.67) | 41.22 (18.86) | 69.66 (15.68) | ||
| Type of surgery | 0.07 | 0.08 | ||||||
| Decompression + fusion | 7.80 (1.76) | 10.46 (0.58) | 11.78 (1.37) | 19.54 (8.35) | 36.33 (13.71) | 66.43 (14.92) | ||
| Decompression- fusion | 8.41 (2.09) | 10.72 (1.16) | 11.89 (1.45) | 21.13 (8.08) | 45.60 (21.30) | 70.50 (17.49) | ||
| Leg pain | ||||||||
| Before surgery | 0.04* | 0.002* | ||||||
| 1 - 2 | 8.5 (1.75) | 10.75 (0.69) | 11.93 (1.53) | 21.48 (9.66) | 37.32 (14.52) | 70 (15.01) | ||
| 2 < | 7.83 (2.08) | 10.49 (1.10) | 11.77 (1.32) | 19.56 (6.80) | 44.59 (20.91) | 67.59 (17.51) | ||
| 6 months after surgery | < 0.001* | < 0.001* | ||||||
| < 1 | 6.50 (1.09) | 11.30 (1.09) | 11.06 (1.98) | 13.43 (5.97) | 25.62 (8.13) | 56.25 (14.08) | ||
| 1 - 2 | 8.54 (1.92) | 10.57 (0.57) | 12 (1.32) | 21.63 (8.12) | 40.13 (13.37) | 70.56 (13.95) | ||
| 2 < | 6.53 (1.19) | 9.92 (2.36) | 11.38 (0.96) | 18.07 (6.93) | 71.92 (32.05) | 66.92 (29.82) | ||
| 12 months after surgery | < 0.001* | 0.02* | ||||||
| < 1 | 6.97 (1.31) | 10.70 (1.40) | 11.41 (1.30) | 18.33 (6.86) | 44.79 (25.88) | 68.75 (20.48) | ||
| 1 - 2 | 8.71 (1.98) | 10.55 (0.59) | 12.06 (1.42) | 21.44 (8.65) | 39.70 (13.63) | 68.60 (15.15) | ||
| Back pain | ||||||||
| Before surgery | < 0.001* | 0.02* | ||||||
| 1 > | 9.37 (2.06) | 10.87 (0.34) | 13.5 (1.09) | 30.62 (15.37) | 50.68 (20.94) | 70.31 (24.25) | ||
| 1 - 2 | 8.41 (1.71) | 10.16 (0.37) | 11.9 (0.94) | 18.75 (4.83) | 36.52 (5.58) | 70 (6.76) | ||
| 2< | 7.8 (1.96) | 10.73 (1.11) | 11.51 (1.41) | 19.30 (6.14) | 41.66 (20.92) | 67.8 (17.56) | ||
| 6 months after surgery | < 0.001* | 0.008* | ||||||
| 1 > | 7.57 (2.02) | 10.68 (0.46) | 12.13 (1.63) | 19.55 (12.82) | 36.57 (17.45) | 63.66 (17.78) | ||
| 1 - 2 | 8.58 (1.79) | 10.71 (0.76) | 11.80 (1.29) | 21.30 (4.62) | 40.54 (12.16) | 72.39 (12.89) | ||
| 2 < | 6.12 (1.55) | 8.87 (2.47) | 10.75 (0.88) | 15 (5.34) | 78.12 (40.35) | 53.70 (28.62) | ||
| 12 months after surgery | < 0.001* | 0.002* | ||||||
| 1 > | 8.49(2.02) | 10.77 (0.66) | 13.53 (1.19) | 21.60 (8.90) | 42.22 (14.11) | 71.08 (14.94) | ||
| 1 - 2 | 7.17(1.41) | 10.15 (1.38) | 11.68 (1.32) | 17.17 (4.55) | 39.10 (27.62) | 62.05 (18.62) | ||
| 2 < | 8.13(1.96) | 10.60 (0.95) | 11.84 (1.41) | 20.41 (8.21) | 41.38 (18.66) | 68.65 (16.44) | ||
| Regular activity | ||||||||
| Before surgery | < 0.001* | 0.02* | ||||||
| Yes | 9.46 (2.29) | 10.92 (0.27) | 13.53 (1.19) | 30 (15) | 50.15 (21.1) | 70 (23.80) | ||
| No | 8 (1.89) | 10.57 (0.98) | 11.68 (1.32) | 19.46 (60) | 40.52 (18.26) | 68.52 (15.66) | ||
| 6 months after surgery | < 0.001* | 0.03* | ||||||
| Yes | 9.12 (1.98) | 10.79 (0.72) | 12.53 (1.54) | 22.69 (10.6) | 42.15 (14.77) | 68.65 (14.76) | ||
| No | 7.37 (1.58) | 16.46 (1.07) | 11.31 (1.04) | 18.65 (5.55) | 40.79 (21.24) | 68.65 (17.72) | ||
| 12 months after surgery | < 0.001* | 0.02* | ||||||
| Yes | 8.26 (1.93) | 8.37 (1.99) | 11.87 (1.40) | 20.72 (8.25) | 39.56 (14.22) | 70.51 (14.51) | ||
| No | 6 (1.19) | 10.73 (0.66) | 11.37 (1.59) | 15 (0.34) | 72.50 (45.43) | 68.65 (16.44) | ||
| Walk, m | ||||||||
| Before surgery | < 0.001* | 0.001* | ||||||
| 100 > | 8.01 (1.92) | 10.59 (1) | 11.60 (1.31) | 19.12 (5.89) | 40.56 (18.31) | 69.24 (14.86) | ||
| 100 - 500 | 8.90 (2.10) | 16.70 (0.47) | 13.35 (1.08) | 28.50 (14.33) | 46.55 (20.45) | 65 (24.33) | ||
| 6 months after surgery | < 0.001* | 0.002* | ||||||
| 100 > | 8.01 (2.31) | 10.44 (1.16) | 11.44 (1.51) | 17.29 (6.86) | 40.90 (23.08) | 61.63 (15.18) | ||
| 100 - 500 | 8.23 (1.69) | 10.64 (0.61) | 12.03 (1.16) | 22.77 (8.55) | 42.17 (14.89) | 74.01 (15.62) | ||
| 501 - 1000 | 8 (1.73) | 13 (0.01) | 15 (0.01) | 20 (0) | 30 (0) | 66.66 (11.54) | ||
| 12 months after surgery | < 0.001* | < 0.001* | ||||||
| 100 > | 5 (0.01) | 6.75 (1.50) | 10 (0.01) | 16.56 (5.69) | 31.48 (8.43) | 62.42 (13) | ||
| 100 - 500 | 7.64 (1.72) | 10.31 (0.55) | 11.29 (1.29) | 25.56 (9.07) | 50.64 (13.06) | 75.94 (16.23) | ||
| 501 - 1000 | 9.13 (2.08) | 11.61 (0.41) | 12.52 (1.26) | 21.04 (5.10) | 35.08 (12.11) | 68.65 (16.44) | ||
| 1000 < | 7.79 (1.21) | 11.12 (0.79) | 12.12 (1.32) |
5. Discussion
In this study among 145 patients participating who were candidates for lumbar disc degeneration surgery, 62.1% were female. The mean age was 49.53 (9.8) years with range 36 (32 - 68 years). In the majority of similar studies, the mean and average age of disc degeneration was higher (17, 18). Stromqvist et al. in one cohort survey published in 2017 indicated the quality of life in patients in all age groups before and one year after the disc degeneration surgery improved but this improvement was higher in older age significantly (19). Although in the current study the best preoperative QOL score was in the 41 - 50 age group the best situation 6 and 12 months after surgery was related to the 61 - 70 age group (despite the worst score before the surgery). Nonetheless, the best VAS score belonged to 30 - 40 age group’s three times (P < 0.001). In this research we did not find mean difference between EQ5D/VAS score and gender while Jansson et al. showed women had lower pre- and post-operative EQ-5D scores than men (6). In the current survey, the maximum EQ5D/VAS score reported in normal BMI after surgery while before surgery was in the obese group. In another cohort study by Knutsson et al., the 2 years following-up showed that despite the reduced pain and improved walking ability in obese patients after surgery, the QOL score was higher in normal and overweight groups (11). Another study by Chapin et al. pointed outpatients with BMI scores over 40 had a worse outcome than who were not morbidly obese (18). We found higher QOL in living with family vs alone (P < 0.001). Fitzgerald et al. in one investigation mentioned that patients with more social support (married or living with someone) had 9 times more improvement in bodily pain over 3 follow-up periods (20). Yazdi Ravandi et al. in one research in Iran showed the longtime pain is associated with less quality of life in patients which is in agreement with our study (21). Sanden et al. reported that smoking is a significant factor in patient stratification after surgery (22). Forsth et al. in one randomized trial compared the efficacy of the decompression surgery with or without fusion technique in patients who have lumbar spinal stenosis and reported EQ-5D score for leg pain was lower in infusion group (23) though we did not find any difference between mean QOL score in 2 type decompression in three measured times. In the Jansson et al. study back and foot pain and preoperative walk distance improved after one year of surgery (6). In our study also, QOL based EQ5D/VAS significantly improved in regular activity, leg and back pain scale as well as walking distance (meters) in following up 6 and 12 months after surgery. There are some limitations to this study. Major information was obtained from the patients themselves, which may lead to information bias. In addition, we replaced patients who had not referred or called for following up with other patients during this survey. So, we did not have the information of these patients to missing data analysis.