1. Background
Spinal cord injury (SCI) is a mixture of motor, sensory and autonomic disorders caused by injury to the spine due to various causes including trauma, sports injuries, violence, etc. (1).
The incidence of SCI in developing countries is 25.5/million/year (95% CI: 21.7 - 29.4/million/year) and ranges from 2.1 to 130.7/million/year. Complete SCIs were found to be more common than incomplete injuries (complete SCI: 56.5%; 95% CI: 47.6 - 65.3; incomplete SCI: 43.0%; 95% CI: 34.1 - 52.0). Similarly, paraplegia was found to be more common than tetraplegia (paraplegia: 58.7%; 95% CI: 51.5 - 66.0; tetraplegia: 40.6%; 95% CI: 33.3 - 48.0) (2, 3). Furthermore, SCI can cause many long-term complications, such as chronic pain, spasticity, contractures, bowel and bladder dysfunction, bedsores, etc. Pain is one of the most important complications of spinal cord injury (4-9).
It affects various aspects of life among SCI patients and decreases their quality of life (1, 10). Approximately 80% of spinal cord injury patients report pain and one-third of them report severe chronic pain which disrupts their activities and quality of life (1). Pain in SCI patients is categorized into two groups of neuropathic and musculoskeletal pains. The latter engages various parts in the body including back, chest, neck, upper limbs and shoulders (11-15).
Shoulder pain is one of the most prevalent pains in spinal cord injury patients. Over time, approximately 50 percent of these patients are afflicted by shoulder pain. It occurs in both paraplegic and tetraplegic patients. In paraplegic patients, the cause of the pain is repeated moves and overuse of upper limbs to carry out daily activities (16). In quadriplegic patients, the major cause of this pain is lack of muscle balance and lack of active moves in the shoulder (17).
Repetitive superior and posterior shoulder joint forces produced during traditional wheelchair (WC) locomotion can result in subacromial impingement if unopposed, as with muscular fatigue or weakness. Other common diagnoses in individuals with SCI presenting with shoulder pain are: bursitis, tendinopathy, rotator cuff tears, biceps tendon tears or acromioclavicular joint arthropathy (18). Shoulder pain can negatively affect mobility, participation in social activities and quality of life (19).
2. Objectives
Considering the importance of the existence of pain in spinal cord injury patients (17), in the present study, we intended to investigate the prevalence of shoulder pain in spinal cord injury patients that referred to our clinic and studied the possible risk factors.
3. Methods
A cross-sectional study was performed at Imam Khomeini Hospital between June 2016 and Sep 2017 including SCI veterans admitted to our center for regular follow-up and planning rehabilitation program. One hundred and twenty spinal cord injury patients were referred to the rehabilitation clinic of the “brain and spinal cord” institute. Out of these patients, 70 who met the inclusion criteria (SCI patients who were injured more than 6 months ago) were included in our study. In addition, the exclusion criteria were: a major systemic disease, history of previous trauma to the shoulder area, history of injection in the shoulder region within the last six months, and the consumption of regular pain-reliever drugs over the last month.
Patients were briefed upon entering the study, and they completed the informed consent form. Then, a specialist in physical therapy and rehabilitation examined the patients and filled a questionnaire including demographic data (age, sex, job, and marital status); BMI and details related to the spinal cord injury were completed. The precedence of the injury, the cause of SCI, and the severity of the disorder were assessed through the ASIA (American Spinal Injury Association) impairment scale, which classified SCI to 5 levels of severity (A to E). Afterwards, the translated version of DASH (the disabilities of the arm, shoulder, and hand) questionnaire was filled based on the patients’ responses. The DASH questionnaire is a standard questionnaire to investigate shoulder pain, the Persian translated version of which has been validated (20). According to the DASH score guideline, a total score less than 15 means patients have no problem, a total score between 15 and 40 means moderate pain (doing their activity with pain) and more than 40 means a severe problem.
SPSS software version 19 was used for statistical analysis. To compare quantitative values, the student’s t-test or correlate binary test and to compare the proportions the chi-square test or Fisher's exact test were used.
4. Results
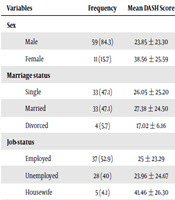
We assessed 70 patients in our study. Among those, 59 (84.3%) of these patients were men and 11 (15.7%) were women. The mean age of the patients was 36 ± 10.9. The mean duration passed after injury was 5 years and 7 months. Of the under study patients, 10 patients (14.3%) suffered from cervical SCI, 55 cases (78.6%) from thoracic paraplegic and 5 cases (7.1%) from lumbar paraplegic SCI. The patients were investigated considering the variables related to spinal cord injury and their relationship with DASH index. The results are shown in Table 1.
| Variables | Finding | P Value with Increasing in Variables |
|---|---|---|
| Age, y | 35.9 ± 10.9 | 0.20 |
| BMI, kg/m2 | 23.6 ± 3.5 | 0.36 |
| Duration pass from injury, mo | 87.7 ± 69.3 | 0.44 |
| Duration of wheelchairs usage, mo | 81.70 ± 54.9 | 0.44 |
The mean value of the quantitative variables such as age, BMI, duration after injury, length of time of wheelchair use and the relationship of DASH level are demonstrated in Table 2.
| Variables | Frequency | Mean DASH Score | P Value |
|---|---|---|---|
| Sex | 0.06 | ||
| Male | 59 (84.3) | 23.85 ± 23.30 | |
| Female | 11 (15.7) | 38.56 ± 25.59 | |
| Marriage status | 0.7 | ||
| Single | 33 (47.1) | 26.05 ± 25.20 | |
| Married | 33 (47.1) | 27.38 ± 24.50 | |
| Divorced | 4 (5.7) | 17.02 ± 6.16 | |
| Job-status | 0.3 | ||
| Employed | 37 (52.9) | 25 ± 23.29 | |
| Unemployed | 28 (40) | 23.96 ± 24.67 | |
| Housewife | 5 (4.1) | 41.46 ± 26.30 | |
| Causes of SCI | 0.1 | ||
| Falling | 21 (30) | 29.89 ± 25.44 | |
| Gunshot | 5 (7.1) | 5.32 ± 7.57 | |
| car accident | 39 (55.7) | 26.12 ± 24.47 | |
| job accident | 4 (5.7) | 24.50 ± 12.40 | |
| sport injury | 1 (1.4) | 60.40 | |
| Type of SCI | 0.3 | ||
| Complete | 33 (47.1) | 28.83 ± 21.04 | |
| Incomplete | 37 (52.9) | 23.78 ± 26.57 | |
| ASIA impairment scale | 0.6 | ||
| A | 43 (61.4) | 25.22 ± 23.16 | |
| B | 17 (24.3) | 32.12 ± 24.45 | |
| C | 7 (10) | 21.78 ± 32.58 | |
| D | 3 (4.3) | 16.13 ± 15.83 | |
| Daily using of wheelchair | 0.5 | ||
| Less than 3 times | 54 (77.1) | 28.13 ± 15.17 | |
| 3 - 6 times | 10 (14.3) | 22.74 ± 13.67 | |
| 7 - 12 times | 2 (2.9) | 7 ± 2.37 | |
| More than 12 times | 4 (5.7) | 12 ± 5.74 |
Frequency of Qualitative Variables, Mean DASH Score AND Correlation Between Them (Chi-Square and Covariance Analysis)a
The overall prevalence of shoulder problems was 59%. Among the thoracic SCI patients, prevalence of shoulder pain in the cervical, the thoracic and lumbar group was 80%, 58.2%, and 20% respectively. Mean of DASH score in cervical, thoracic and lumbar group was 51, 23 and 12 respectively (P value < 0.001). Table 3 demonstrates the prevalence of pain according to the SCI type. The severity of shoulder pain increased with age and the time passed after injury, but this increase was not statistically significant (P value > 0.05).
| SCI Type | DASH Score < 15 % | DASH Score = 15 - 40 % | DASH Score > 40 % |
|---|---|---|---|
| Cervical | 20 | 20 | 60 |
| Thoracic | 41.8 | 40 | 18.2 |
| Lumbar | 80 | 50 | 0 |
| Total | 41.4 | 35.7 | 22.9 |
Mean of DASH Score According SCI Type
Multi-variant regression analysis was done to find possible risk factors. In our population, also male gender, level of injury at lumbar thoracic and cervical level can predict mean Dash score. The results of this analysis are presented in Table 4.
| Model | Unstandardized Coefficients | Standardized Coefficients | t | Sig. P Value | |
|---|---|---|---|---|---|
| B | Standard Error | Beta | |||
| Constant | 73.404 | 14.942 | 4.913 | 0.000 | |
| Male gender | -17.856 | 8.691 | -0.272 | -2.054 | 0.043 |
| Injury level | |||||
| Lumbar | -44.440 | 12.346 | -0.478 | -3.600 | 0.001 |
| Thoracic | -26.109 | 7.569 | -0.448 | -3.449 | 0.001 |
| Cervical | -5.508 | 5.001 | -.144 | -1.101 | 0.01 |
Multi-Variant Regression Analysis for Possible Risk Factorsa
5. Discussion
Shoulder pain, a prevalent complaint in spinal cord injury patients, affects the patients’ quality of life. It can interfere with the patients’ rehabilitation process and independent life. Shoulder pain tends to be more prevalent among complete spinal cord injury patients (21).
Shoulder pain is probably due to frequent use of wheelchair and tendon injuries in paraplegic patients and loss of muscular balance in quadriplegic patients (1, 17). Shoulder pain is more common in paraplegic patients because of the overuse of upper limbs and can be caused by several reasons such as biceps tendinitis, impingement syndrome, subacromial bursitis, capsulitis, and osteoarthritis (22).
The prevalence of shoulder pain among chronic paraplegic patients has been estimated to be 30 - 64 percent (16).
In a study carried out in Brazil in 2011 intending to evaluate shoulder problems of spinal cord injury patients, the prevalence of shoulder pain among quadriplegic and paraplegic SCI patients was 88.89%, and 42.85%, respectively. In our study, generally of the 70 spinal cord injury patients, 41.4% had no shoulder problems, 58.6% had shoulder problems among which 35.7% had moderate shoulder problems and 22.9% had severe shoulder problems. The pain was more prevalent and severe in the quadriplegic group.
Age, gender, injury level, injury duration and the number of times moving from wheelchair onto bed and back factors which reported in previous research affect shoulder pain (23-25). Studies also indicated that the time passed after the injury and transferring from wheelchair to bed and back were considered as influential factors on shoulder pain (11, 26). In a systematic review carried out in 2014, shoulder pain prevalence among quadriplegic patients has been reported to be more frequent in general. In this study, pain prevalence has been more common among women. Besides, other demographic features such as age and weight have shown a positive correlation with the prevalence of shoulder pain (27).
Another study investigated the shoulder pain prevalence and its correlation with moving from and back to wheelchair showing that among 46% of the respondents, 69% had pain in the upper limb. The pain has been positively correlated with the number of times moving from the wheelchair (28). Factors, directly and indirectly, influencing shoulder pain include age, gender, BMI, injury level, injury duration, and times of transferring from wheelchair to bed and back (23, 24). Based on the results of our study, the pain had a higher prevalence among patients who had fewer than three and more than 24 moves from the wheelchair. This can probably be because patients, who have fewer than three moves from their wheelchair, are not able to move mostly because of secondary complications such as shoulder pain or it may be due to muscle imbalance in the shoulder region. On the other hand, people with more than 24 daily moves experience pain because of the overuse of their shoulders.
Shoulder pain has been reported to negatively influence the quality of life. Lifting objects overhead has been reported to be one of the most painful activities in such patients. In one study 68.4% of the patients have had a low quality of life (25). Activities that create problems for the patients include activities and tasks related to wheelchair use such as pushing up the wheelchair on an uneven surface. This activity has been reported to cause severe pain for the patients (11-13). In addition, pain intensity is positively correlated with the number of exposures with activities of daily living (ADL). Therefore, greater care must be taken in detailed evaluation, prevention, rehabilitation and effective medical treatments for such cases (11, 26, 29, 30).
5.1. Conclusions
Based on the result of our study, it seems that shoulder pain has a relatively high prevalence and is more severe in cervical quadriplegic spinal cord injury patients. Given the fact that the quality of life among spinal cord injury patients is considerably influenced by its secondary complications such as shoulder pain, the appropriate attention should be paid to their shoulder pain, asking patients about the pain and examining them regularly. Besides, a proper pain management plan for these patients can be helpful in improving the quality of their life.