1. Context
Low back pain (LBP) is one of the most common reasons for functional disability in all populations, both in industrialized and non-industrialized countries (1, 2). An increasing incidence of LBP has been reported in recent years. For example, the total direct healthcare cost of LBP in the United States is between $100 and $200 billion annually (3). Chronic LBP (CLBP) can be described when symptoms persist for more than three months (4, 5). The prevalence of CLBP is around 23%, which results in a disability of 11% - 12% of the CLBP population (6).
There are many studies about LBP; however, many aspects of LBP and the most successful treatments remain unclear. The severity of pain and disability are two important factors in assessment, treatment, and improvement of LBP that they are measured by various scales in clinical and research settings. Arnstein’s study showed that improvement of pain and disability should be a priority in the treatment of patients with LBP. The improvement of pain and disability of patients with CLBP is one of the reasons for referring them to therapists for consultation and treatment (7). There are several non-exercise physiotherapy interventions for treating LBP. Kinesio taping (KT) is one intervention that commonly used in these patients. A Japanese chiropractor named Dr. Kenzo Kased developed KT, which is a latex-free, adhesive, and stretchable tape without restricting the range of motion (8). The potential mechanisms of KT are unclear. However, it has been reported that applying KT affects five human physiological systems, including skin, fascia, blood supply, lymphatic system, muscles, and joints and induce the following effects: (1) improvement of muscle function; (2) activation of circulation (blood and lymph); (3) decrement of pain; (4) support the joint function, and (5) improvement of proprioception (9-13).
A few published clinical trials have provided preliminary evidence on the potential mechanisms of KT, but many questions remain unanswered. Limited studies have reported positive effects of KT in the treatment of CLBP, and the results have been inconsistent. Some systematic reviews on KT in patients with CLBP have been previously published (8, 14-17). For example, Li et al. (15) stated in their systematic review that the KT is not superior to placebo taping regarding pain reduction in LBP. In another systematic review, Junior (14) found very limited evidence to suggest that KT was not better than any other intervention for most of the outcomes evaluated in patients with non-specific CLBP. In these studies, various methods of lumbar KT have been used to improve the severity of pain and disability; nevertheless, the best method is unclear. In all the systematic reviews, KT was compared with KT combined with other interventions (i.e., exercise, manual therapy, and/or electrotherapy) or compared with other interventions alone. Also, the efficacy of the various methods of KT on the lumbar spine has not been argued in the previous literature reviews.
To the best of our knowledge, no literature review assessed and compared various methods of lumbar KT regarding the reduction of pain and functional disability in patients with CLBP. Therefore, we aimed to investigate the previous studies (1990 up to January 31, 2020) about the effect of various methods of KT on the low back region regarding pain and functional disability in patients with CLBP.
2. Evidence Acquisition
2.1. Search Strategy
In the current review study, we tried to identify all published articles that assessed the effect of KT on pain and disability in people with CLBP. A literature search for the period from 1990 up to January 31, 2020, was conducted on PubMed, ProQuest, Science Direct, Thomson, OVID, Google Scholar, Scopus, MEDLINE, and PEDro databases. The used keywords including, Kinesio Taping, Kinesiology Taping, Chronic Low Back Pain, and the searches were adjusted for each database.
2.2. Selection of Studies
Two independent reviewers (SA and AB) read all titles and abstracts and selected the studies accordingly. The whole article was read. If there was any unresolved disagreement between the reviewers, another reviewer was invited to decide on the inclusion of the studies. Finally, seven articles were included based on the inclusion criteria. These studies were full reports published in peer-reviewed journals in the English language, and the list of references from the relevant publications was also used. The inclusion criteria were: (1) articles assessing the effects of Kinesiology Taping/Kinesio Taping application on pain or disability in individuals with CLBP or nonspecific CLBP; (2) control group including either sham/placebo taping.
The exclusion criteria were: the studies that the effect of KT on pain and disability has not evaluated alone, non-peer-reviewed publications, opinion articles, and non-English articles.
2.3. Data Extraction
Data were extracted as follows: name of authors, year of publication, description of the intervention (KT application, duration of taping, amount of tension applied to the tape, renewal of taping, removing method of taping and safety or allergic sign of taping), description of the control group (method of sham or placebo taping or no taping), type of LBP, number and age of participants, study outcomes, assessment times, study results, and conclusions.
2.4. Participants
The individuals in the included articles had to be patients, adults with a diagnosis of CLBP, or non-specific CLBP that subjects experienced pain for more than three months.
2.5. Outcome Measures
2.5.1. Pain
Pain intensity as the outcome measure was assessed by the Visual Analogue scale (18-20) and/or a Numerical Rating scale (NRS) (21-24). Both scales are unidimensional single item scales that evaluate the levels of pain intensity comprehended by the participant using an 11-point scale, ranging from 0 to 10, where 0 shows no pain, and 10 shows extreme pain that you could conceive (25). In these studies, the recall period of these scales is different; however, the participant is generally asked to report the level of pain intensity in the past day (26).
2.5.2. Disability
The disability level of participants was evaluated by two different questionnaires, including the Roland Morris Disability questionnaire (RMDQ) (20-24) and the Oswestry Disability index (ODI) (18, 19). The RMDQ is a 24-item self-rated physical disability measure caused by LBP in which higher numbers on RMDQ means higher levels of disability (27). The ODI is a questionnaire used by clinicians and researchers to quantify disability and the limitations of various daily activities for LBP, and consists of 10 items of which is scored on a scale of 0 - 5 so that 5 shows the greatest disability (28).
3. Results
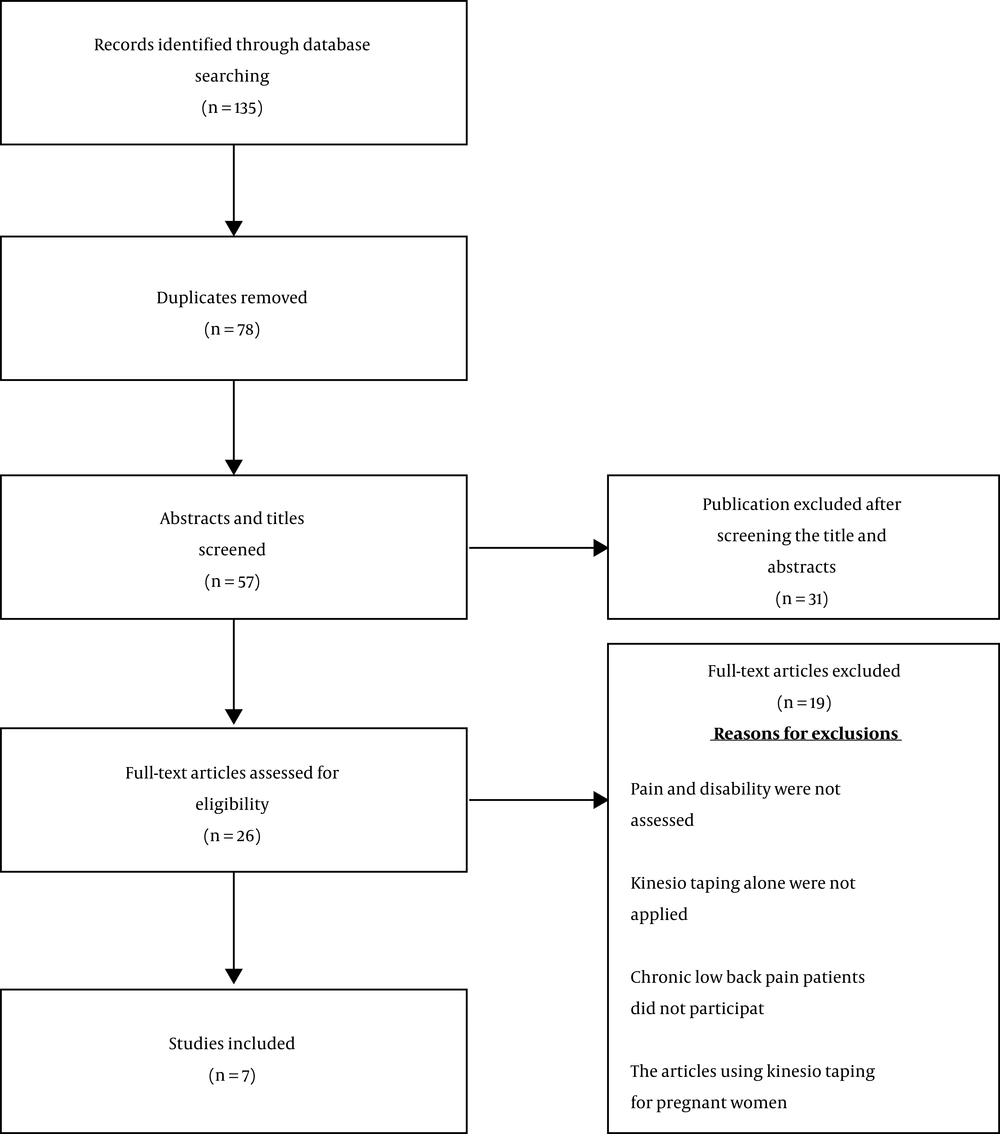
We found 135 articles using the mentioned keywords, and seven articles (18-24) were included based on the above-mentioned inclusion criteria. All of the included studies were randomized control trials (RCTs). Figure 1 illustrates the evaluation process of the study selection. Table 1 shows the details of the included articles chronologically from 2012 to 2018. The studies' sample size was between 44 - 148, and the age range was 18 - 80 years.
| Authora’ Names | Subjects (Numbers) | Outcome Measure and Follow-Up | Method of KT and Duration | Conclusion |
|---|---|---|---|---|
| Macedo et al.(22) | 108 patients with chronic nonspecific LBP (12 wk) | 1) Pain-NRS | Ctrl group: No taping | After three days of taping, improved pain relief was observed for Exp group 1 and Placebo group compared with Ctrl group. For disability, there was a difference between Ctrl group and Exp group 1 at three days and 10 days. Conclusion of the study: KT can reduce pain after three days taping even without tension. Also, KT with tension can decrease disability after 3 and 10 days in individuals with LBP. |
| (2) Disability-RMDQ; follow-up at 0 mo (10 days) | Placebo group: Sham taping | |||
| Exp group1: KT | ||||
| Exp group 2: Micropore tape | ||||
| Intervention protocols: placebo group, I-shaped KT over each paravertebral muscle with no tension (0% of tension); Exp group 1, the tape was attached in the shape of an “I” over the paravertebral area up to the T12 vertebra with 10% to 15% of tension. The anchor tape (4 - 5 cm) was applied directly above the transverse process of the T12 vertebra without tension. The same procedure was then performed on the opposite side; Exp group 2, the participants received the application in the same way as Exp group 1. | ||||
| Exp group 1 (KT with tension), n = 26; age (45): 25 (6) | ||||
| Exp group 2, n = 26; age (45): 25 (5); Ctrl group, n=26; age (45): 24 (4); placebo group, n = 26 age (45): 24 (5) | ||||
| Renewal of taping: only one time applied | ||||
| Duration: 3 days | ||||
| Uzunkulaoglu et al. (20) | 60 patients with chronic nonspecific LBP (12 wk) | 1) Pain-VAS | Placebo group: sham taping | Statistically significant improvements for pain and disability were found for both groups (placebo and Exp group) after one month of intervention. There were statistically significant differences between the groups’ pain and disability at the first month of intervention. However, at sixth month follow-up, only ODI values were significantly different between groups. Conclusion of the study: KT can reduce pain and disability at short time. Disability improvement was maintained at long term. |
| (2) Disability-ODI; follow-up at 1/6 mo | ||||
| Exp group: KT | ||||
| Intervention protocols: Exp group, taping was performed in a neutral spine position, and then the base of Y strip was attached in the sacroiliac joint with 15% - 25% of tension or paper-off tension. After that, individuals were asked to move into flexion with rotation to one side, and physiotherapist attached the tail of the Y strip on the opposite side. For the last approximately 5 cm, the physiotherapist laid down the tail with no tension. The individual moved into forward flexion with rotation to the opposite side. Therefore, the second Y tail would be attached. Placebo group: “Y” strip sham taping of the same material was attached to ineffective parts of the muscle without tension to sacroiliac joint in the neutral position. | ||||
| Exp group (KT with tension), n = 30 age (45): 21.63 (1.771) | Renewal of taping: six times by intervals of three days for 15 days | |||
| Placebo group, n = 30 age (45): 21.27 (1.617) | ||||
| Duration: 15 days | ||||
| Araujo et al. (24) | 145 patients with chronic nonspecific LBP (12 wk) | 1) Pain-NRS | Ctrl group: sham taping | No significant between-group differences for pain intensity and disability after 6 months. Conclusion of study: four weeks of KT and even 6 months follow-up was no better than sham taping for individuals with chronic LBP. |
| Exp group: KT | ||||
| (2) Disability-RMDQ; follow-up at 0/6 mo | Intervention protocols: Ctrl group, I-shaped KT over each paravertebral muscle with no tension; Exp group, I-shaped KT over each paravertebral muscle with 10% - 15% of tension. | |||
| Exp group, n = 73 age (45): 56 (76) | ||||
| Renewal of taping: twice per week | ||||
| Duration: 4 wk | ||||
| Ctrl group, n = 72 age (45): 59 (80) | ||||
| Al-Shareef et al. (18) | 44 patients with chronic nonspecific LBP (12 wk) | 1) Pain-VAS | Ctrl group: sham taping | After KT, pain, and disability significantly improve. Significant between-group differences were reported at follow-up. Conclusion of the study: after two weeks KT, pain, and disability were reduced. However, these positive effects were very small to be considered clinically important when compared with sham taping. |
| (2) Disability-ODI; follow-up at 0/1 mo | Exp group: KT | |||
| Intervention protocols: Ctrl group, I-shaped KT over each paravertebral muscle with no tension; Exp group, I-shaped KT was attached over the skin in the paravertebral muscle up to the T12 vertebra at 10% to 15% of tension. The anchor of tape (4 - 5 cm) was applied directly above the transverse process of the T12 vertebra without tension. The same procedure was then performed on the opposite side. | ||||
| Exp group, n = 23 age (45): 37.55 (9.82) | ||||
| Ctrl group, n = 21 age (45): 35.55 - 8.04 | ||||
| Renewal of taping: twice per week | ||||
| Duration: 2 wk | ||||
| Luz Junior et al. (21) | 60 patients Chronic nonspecific LBP (12 wk) | (1) Pain-NRS | Ctrl group: no taping | After 48 hours taping, there was a significant difference between the KT group versus the control group but no significant difference between the KT group versus the placebo group. There were no significant differences for the other outcomes. Conclusion of the study: The KT was not better than placebo in individuals with chronic LBP. |
| Placebo group: Micropore taping | ||||
| (2) Disability-RMDQ; - Follow-up at 0 mo (1wk) | Exp group: KT | |||
| Exp group, n = 20 age (45): 44.3 (15.0) | Intervention protocols: Placebo group, The Micropore tape was attached over the paravertebral muscle in the stretched position; Exp group: The KT was attached over the paravertebral muscle with 10% - 15% of tension in the stretched position. | |||
| Ctrl group, n = 20 age (45): 48.1 (13.4) | ||||
| Renewal of taping: only one time applied | ||||
| Duration: 48hrs | ||||
| Placebo group, n = 20 age (45): 50.1 (17.5) | ||||
| Parreira et al. (23) | 148 patients with chronic nonspecific LBP (12 wk) | (1) Pain-NRS | Ctrl group: sham KT | There were no significant differences in pain and disability improvement after taping. No significant between-group differences were reported at follow-up. Conclusion of the study: KT with tension is not more effective than the tape without tension for pain and disability reduction. |
| Exp group: KT | ||||
| Intervention protocols: Ctrl group, I-shaped KT over each paravertebral muscle with no tension; Exp group: I-shaped KT over each paravertebral muscle with 10% - 15% of tension. | ||||
| (2) Disability-RMDQ; - Follow-up at 0/2 mo | ||||
| Exp group, n = 74 age (45): 56 (76) | ||||
| Renewal of taping: twice per week | ||||
| Ctrl group, n = 74 age (45): 59 (80) | Duration: 4 wk | |||
| Castro-Sanchez et al. (19) | 60 patients with chronic nonspecific LBP (12 wk) | (1) Pain-VAS | Ctrl group: sham KT | Pain and disability significantly reduced more in the KT group compared to the control group after taping. Significant between-groups difference sustained only for pain at follow-up. Conclusion of the study: KT improved disability and pain in individuals with chronic nonspecific LBP, but these positive effects may be very small to be clinically valuable. |
| Exp group: KT | ||||
| (2) Disability-ODI, RMDQ; follow-up at 0/1 mo | Intervention protocols: Ctrl group, single I-strip of the same material attached transversely immediately above the point with maximum lumbar pain; Exp group: four blue I-strips applied with 25% of tension in a star shape over the point with maximum lumbar pain. | |||
| Exp group, n = 30 age (45): 50 (15) | ||||
| Ctrl group, n = 30 age (45): 47 (13) | ||||
| Renewal of taping: no renewal | ||||
| Duration: 1 wk |
Abbreviations: Ctrl, control; Exp, experimental; KT, Kinesio taping; LBP, low back pain; MD, mean difference; NRS, Numerical Rating scale; ODI, Oswestry Disability questionnaire; RMDQ, Roland-Morris Disability questionnaire; VAS, visual analog scale.
Some studies were excluded from the current study, and the most important causes were not in the English language; pain and disability were not evaluated, KT alone were not applied, or CLBP patients did not participate. Also, the articles using KT for pregnant women were not evaluated.
3.1. Types of KT Methods
In the included studies, application forms of KT were various, but these methods were based on the principles of Kenzo Kase’s book (29). In total, there are various forms of KT application, including “Y”, “I”, “X”, “fan”, “web” (modified “fan”), and “donut” shapes that these forms were applied depending on the size of the treatment region and purpose of therapy. The purpose of treatment can be a change of muscle tone (inhibitory or facilitatory effect), improvement of pain and disability, support or correction of joint, lymphatic drainage (both “web” and “fan” ) (9).
There is no gold standard for the methods of KT for CLBP patients. In the included studies, three different methods of KT were used, including I shape (18, 21-24), Y shape (20), and star shape (19). In the I-shaped method, the KT was bilaterally applied to the lumbar paravertebral muscles up to the T12 vertebra in the stretched position. The initial anchor points of tape applied to the posterior superior iliac crest without stretch (Figure 2A) (18, 21-24). All included articles used this method except two articles. In one study, the star shape taping was used that four I-strips of KT was placed over the point of maximum lumbar pain (Figure 2B) (19). In another one, taping was started in a neutral spine position of the participant, and later the base of Y strip was attached to the sacroiliac joint area, then participants were asked to perform flexion with rotation to one side (for example right side) movement. The physiotherapist laid down the tail with no tension for the last approximately 5 cm. Also, the second Y tail was attached after the participant movement into flexion with rotation to the opposite side (Figure 2D) (20).
A, I-shaped Kinesio tape (KT) application technique applied bilaterally on the lumbar paravertebral muscles; B, star shape KT application that four I-strips of KT was placed over the point of maximum pain in the lumbar area; C, placebo taping that single I-strip applied transversely immediately above the point of maximum lumbar pain; and D, Y shape KT application that the base of Y strip was applied to the sacroiliac joint region and two tails over the lumbar paravertebral muscles.
For placebo or sham taping, three methods were used as an experimental group of the same material include I shape taping without tension (18, 21-24), single I-strip a transversely immediately above the point of maximum pain in the lumbar region (Figure 2C) (19) and “Y” strip on a part of the muscle without tension to sacroiliac joint (20).
Furthermore, various pain locations likely exist in CLBP patients, including point of maximum lumbar pain, paravertebral muscles, lumbosacral junction, or sacroiliac joint, but in none of the included studies, the pain location was not mentioned. Overall, the effect of I shape KT on pain reduction was significant in three of five studies (18, 21, 22), and for disability, the reduction was significant in two of five studies (18, 22). Patients with CLBP could gain from the overlapping application (star shape) (19), and in that way, decrease the pain and disability; also, Y shape taping can improve pain and disability in these patients (20).
3.2. KT Removing Method
The removing method of KT in the included articles was not mentioned.
3.3. Type of Applied Tension of KT
The tension of KT is explained as one of the key factors for successful treatment, where full tension is 100%, intense 75%, moderate 50%, light 15% - 25%, very light 0% - 15%, and no tension 0%. These forms of tension are used for support of weak muscle or correction of joint position (both 75% and 100%), muscle activation in weakened muscles positioned from the origin to the muscle insertion (25% - 50%), muscle inhibition caused by overuse or muscle overstretching applied from the insertion to the origin of muscle (15% - 25%) and reduction of edema (0% - 15%) (9, 30).
In the seven included studies, the I shape taping was applied with 10% - 15% tension in five studies (18, 21-24) also the star shape, and Y shape taping was used with 25% tension in the experimental group (19, 20), while no tension for sham, placebo, and control group (18-24).
In general, researchers of these studies used various methods of taping; for example, 10% to 25% of tension over the pain point or the paravertebral muscles These ranges of tension could relieve the pain (18-22) and improve disability (18-20, 22). Based on the original KT method, convolutions enhance blood and lymphatic flow that it can reduce pain (9). So, using proper tension of KT is one of the critical factors for effective implementation.
3.4. The Duration of KT Application
Around 10 minutes, the participant will not feel the KT on the skin, and in approximately 20 minutes, it will adhere to the skin. Afterward, the decreasing of the elastic polymer function occurs, and the application shall last for 3 - 5 days (30). In the assessed studies, the short-term effect of KT on pain and disability was evaluated (48 hours to 1 week) (19, 21, 22). Also, the medium-term effect of KT was evaluated for 2 - 4 weeks (18, 23, 24); however, only one of them investigated the effect of KT for six months (20).
Based on the included studies, KT could reduce pain and disability for a short time (19, 21, 22), while the results of medium effect studies (18, 23, 24) are more in favor of no improvements of pain and disability after applying KT. Also, only one long-term effect study showed a positive effect of KT on pain and disability reduction (20).
3.5. Safety
None of the seven included articles reported any allergic response or skin irritation after KT (18-24).
3.6. Effect on Pain and Disability
All included studies had moderate to large sample sizes in both genders. Regardless of the type of KT method, tension, pain measurement tools, and follow-up time after KT application, KT reduced pain intensity after its application in five (18-22) out of the seven included studies. In three studies (18-20), pain intensity has been measured by VAS that their results showed pain reduction after KT.
The KT decreased disability after its application in four (18-20, 22) out of the seven studies, regardless of the type of KT method and tension, disability measurement tools, and follow-up time after KT application. In only two studies (18, 19), disability has been measured by ODI that their results showed disability reduction after KT.
In 2015, Luz Junior et al. (21) randomized 60 middle-aged men and women into three groups. One group (20 patients with nonspecific CLBP) was treated by the I shape KT with 10% - 15% of tension as the KT group, and the placebo group was received Micropore tape with no tension. The control group had no taping. The authors reported that although disability was reduced in the KT group 2 days after taping, these changes were so small and were not clinically significant. Between-group differences for pain and disability were not statistically significant (21). This study had the shortest assessment time after taping (2 days) and follow-up time (7 days) among the included studies. Based on the previous studies, differences more than two and five points for the pain and disability, respectively, are clinically important (31) that in Luz Junior’s study (21) were not observed even after a seven-day follow-up. They concluded that how the taping applied may influence the results. Similar to Luz Junior’s study, there was another study (19) with a longer follow-up period (four weeks). In this study, the star shape of KT at 25% of tension versus a placebo taping was used in 60 patients with non-specific CLBP. The tension of placebo taping was not reported. The results showed that pain and disability improved in the KT group at one week, but the effect was small, and after four weeks, there was no significant difference. In this study, other outcomes, including trunk flexion range of motion (ROM) and trunk endurance test, were measured that only trunk muscle endurance was significantly better at one week.
In another RCT study, 60 patients with non-specific CLBP, including both genders, were evaluated in either intervention or placebo groups (20). Y shape KT with 15% - 25% of tension was applied versus placebo taping without a tension. They showed significant pain and disability reduction after one month of taping in the KT group. Also, they measured trunk flexion, extension, and lateral flexion ROM. The significant improvements in ROM and disability were maintained after a long-term period (six months). They concluded that these results might be due to the application of the taping method. The Y strip of KT with a particular tension may enhance inputs of cutaneous receptors and facilitated muscle function.
Similarly, Araujo et al. (24) evaluated the effect of KT on pain and disability in 148 patients with non-specific CLBP at long-term follow-up (six months). Only these two studies (20, 24) had the longest follow-up time (six months) among the included studies. However, the results of this study were contrary to the former study (20). The tension and method of taping were different from the former study (23). In this study, I shape taping was used over the paravertebral muscles with 10% - 15% of tension in the KT group and without tension for the control group. They reported that four weeks of KT application was not better than placebo taping for these patients, while six months follow-up showed that these effects are due to placebo.
Before, this study was performed in 2014 with the same participants and protocol at four and twelve weeks (23). The results were the same too, and there were no significant between-group differences. In two other studies (18, 22), the short to medium effects of I shape taping similar to the previous studies were evaluated in 108 and 44 patients with nonspecific CLBP, respectively. Macedo et al. (22) showed that KT reduces pain and improves disability in these patients.
After three days of taping, the results showed reduced pain in both KT groups (with and without tension). Also, after 3 and 10 days, disability improved only in the KT with tension group. Other outcome measures were such as trunk ROM, trunk extensor strength, and electromyographic amplitude. Between-group differences were not statistically significant, and the hypothesis of a placebo mechanism should be considered. Luz Junior et al. (21) found the same results for Micropore tape as Macedo et al. (22). Mecado’s et al. (22) study revealed no significant differences between the control and Micropore tape group, and between the Micropore tape and KT group.
In the second study, Al-Shareef et al. (18) treated the experimental group by KT with tension, whereas the placebo group was without tension. Pain intensity, functional disability, and trunk flexion ROM were assessed before and after the 2-week intervention and at a 4-week follow-up. These results showed improvements in pain, disability, and trunk flexion ROM after 2-weeks taping. These improvements persisted for a 4-week follow-up in the KT group. However, there were no significant differences between groups. The results of this study were similar to the finding of Parreira et al. (23), and the protocol of these RCT studies was the same.
In total, the pain intensity was significantly decreased after the intervention in five studies (18-22) as disability was significantly improved in patients with CLBP in four studies (18-20, 22). Overall, five studies support the use of this therapeutic option in CLBP (18-20, 22, 23), while only one study suggested that KT is better than a placebo in patients with CLBP (22).
4. Discussion
The previous reviews did not investigate the effect of KT based on methods of taping. Therefore, we performed a review study to investigate the efficacy of KT alone in CLBP patients regarding pain and disability. We searched the scientific literature (from 1990 up to January 31, 2020) regarding the effect of various methods of lumbar KT on pain and functional disability in patients with CLBP. Seven studies related to the efficacy of three types of KT on pain and disability in people with CLBP (18-24).
Recent systematic review and meta-analysis reported KT is a convenient application; therefore, it could be used for individuals with CLBP in some patients, especially when the cases could not get other physical therapy programs (15). In the current review, the effect of KT was not evaluated in conjunction with other therapies such as traditional physical therapy and exercise.
The effects of KT in comparison to the placebo taping or no taping may be attributed to the differences in taping application; for example, I-strip taping (18, 21-24), Y-strip (20), and star taping (19). Previous studies suggested that I-strip, Y-strip, and star shape taping could increase lumbar ROM, stimulate correct movements, extensibility, and fatigue delay in healthy subjects and improve the pain and anticipatory postural control in patients with LBP (32-35).
There are several assessment tools such as pain VAS (18-20), NRPS (21-24), and functional disability using the ODI (18, 19) or RMDQ (20-24). Also, the positive effects of KT depend on various factors such as methods of taping, duration of use, the tension of KT, other physical therapy treatments, and severity of pain and disability in individuals with LBP. It seems that every three methods (I shape, star shape, and Y shape) of KT can be effective in reducing pain and disability, but because of limited studies with star and Y shape of KT, we cannot judge the best method of KT based on the included studies. However, based on included studies, it seems that 10% - 25% of tension of KT may be more effective for pain and disability improvements than the other tensions in patients with CLBP. Previous studies reported that 0% to 25% of tension of KT, stretch over pain region could relieve the pain, increase muscle endurance, and promote mobility (19, 32, 36, 37).
Also, it seems that based on the results of the included studies, the short-term effect of KT on pain reduction is positive, while the medium- and long-term effects of it are controversial. A systematic review that evaluated the short-time effects of KT in people with CLBP reported that the efficacy of KT is due to a placebo effect (8). Some physiological mechanisms of KT in pain reduction have been proposed. Applying KT with tension causes lifting the skin and increasing subcutaneous space and as a result, decreased activation of pain receptors, also possibly activates descending inhibitory system. One theory that has been reported is the gate control theory of pain. In this theory, tactile stimulation of KT application over the skin would decrease the afferent signal of large-diameter non-nociceptive fibers resulting in pain reduction (19, 30, 38, 39) Another theory has been proposed that keratinocytes, which are found in the skin, may represent the primary transduction of mechanical non-neuronal stimuli. These mechanisms would activate cascade processes such as intracellular Ca2+ flows, evoking a response from nociceptive fibers (38, 40). Also, there are other positive effects of KT, such as normalize muscle function, improvements of postural control, range of motion increasing, improving circulatory, lymphatic function, and proprioception that these effects indirectly help pain and disability reduction (9, 10, 23, 33, 41, 42). In addition, disability has a direct relationship with pain (43), so the improvement of anyone can improve another one.
This review has some limitations. First, this review included two outcome measures; therefore, future systematic reviews are needed to investigate similar treatment protocols for CLBP. Second, owing to the limited number of studies, this review included only seven articles; thus, the conclusion was unclear and difficult. Therefore, future systematic reviews and meta-analyses are needed on this topic. Third, two of the three KT methods (star shape and Y shape) were investigated only in one study; consequently, the findings of this review should be interpreted with caution.
5. Conclusions
In a nutshell, the KT is suggested as an alternative or complementary treatment. In seven included studies, three methods of KT, including star shape, I shape, and Y shape, were applied, and they differed regarding frequency, tension, and duration of KT. The results of the included studies showed KT could reduce pain and disability in patients with non-specific CLBP. These positive effects may sustain at medium- and long-term periods. These results indicated that KT is a safe method with minimum side effects; however, due to limited included studies, they cannot be compared, and the best method is unclear in this review. Therefore, more high-quality studies regarding various methods of KT and longer follow-up are needed.