1. Introduction
Pemphigus vulgaris (PV) is an autoimmune blistering disorder of the skin and mucous membranes, associated with the formation of autoantibodies against transmembrane glycoprotein components, including desmoglein-3 and/or desmoglein-1 (1). Moreover, PV is a rare skin disorder in the pediatric population, andonly1.4% - 2.9% of cases are reported in children (2). The youngest chronological age of PV is the first day of life in neonates who are born of mothers with a positive history of the disease. Most mothers with PV have a normal full-term pregnancy; however, stillbirth is reported in 1.4% - 27% of mothers with this autoimmune disorder (1). Close maternal and fetal contact leads to the transplacental passage of immunoglobulin G (IgG) autoantibodies from the mother’s blood to the fetus (3, 4). Statistics show that 30% - 45% of carriers of this autoantibody (IgG) present with the symptoms of PV during the neonatal period.
Skin blistering, resembling maternal lesions, develops within the first days or months of the neonate’s life. Although the autoantibodies disappear in the third to fourth months of life, the duration of symptoms is short in most neonates (2 - 3 weeks) (3). Diagnosis of PV is established, based on clinical manifestations and laboratory findings of immunofluorescence or enzyme-linked immunosorbent assays (ELISA), demonstrating the deposition of type1 and type 4 IgGs against desmogleins (3). Owing to the short and mild course of neonatal PV, its treatment is mainly supportive, and corticosteroid therapy is seldom needed for neonates (1).
The similarity of skin lesions in PV to other skin conditions, such as infectious diseases caused by bacterial, viral, and fungal pathogens or inherited bullous disorders, such as epidermolysis bullosa (EB) and incontinentia pigmenti (IP), leads to misdiagnosis, inappropriate hospital admission, and poorantimicrobial treatment of neonates. On the other hand, positive maternal history of the disease, besides laboratory examination, confirms the diagnosis.
Considering the rarity of PV in the neonatal period; herein, we present the case of a neonate with multiple pustular and bullous skin lesions who was born to a mother with a positive history of PV, initiated during pregnancy.
2. Case Presentation
A one-day-old male newborn was referred to the neonatal ward of Mofid Children's Hospital (Tehran, Iran) due to skin eruptions. He was born with a birth weight of 2,900 g, via cesarean section at 38 weeks of gestation to a 30-year-old woman (gravida 1, para 1 abort 0), without a consanguineous marriage. The mother had no history of intrauterine infection, prolonged rupture of membranes (PROM), chorioamnionitis, or other common problems of pregnancy.
During the first hours of life at the nursery, multiple pustules, blisters, and erosions appeared on the skin of the newborn. In terms of appearance, he had a good general condition with good tonicity, normal primitive reflexes, and a normal level of consciousness. His skin color was normal, with no jaundice, cyanosis, or mottling. Also, there was no mucosal involvement, lymphadenopathy, organomegaly, or signs and symptoms of sepsis.
Figures 1 and 2 showed pustular skin lesions on the arm of the neonate, and Figure 3 showed multiple erosive and pustular lesions on the head and neck and upper chest of the patient.
Owing to the generalized skin eruptions (Figures 1 - 3), he was admitted to the neonatal ward of maternity hospital. A sepsis workup, including blood sampling for blood culture, cell blood count (CBC), and C-reactive protein (CRP) was carried out, and systemic intravenous antibiotics were administered. The persistence of skin eruptions, despite antimicrobial therapy, led to his referral to our hospital.
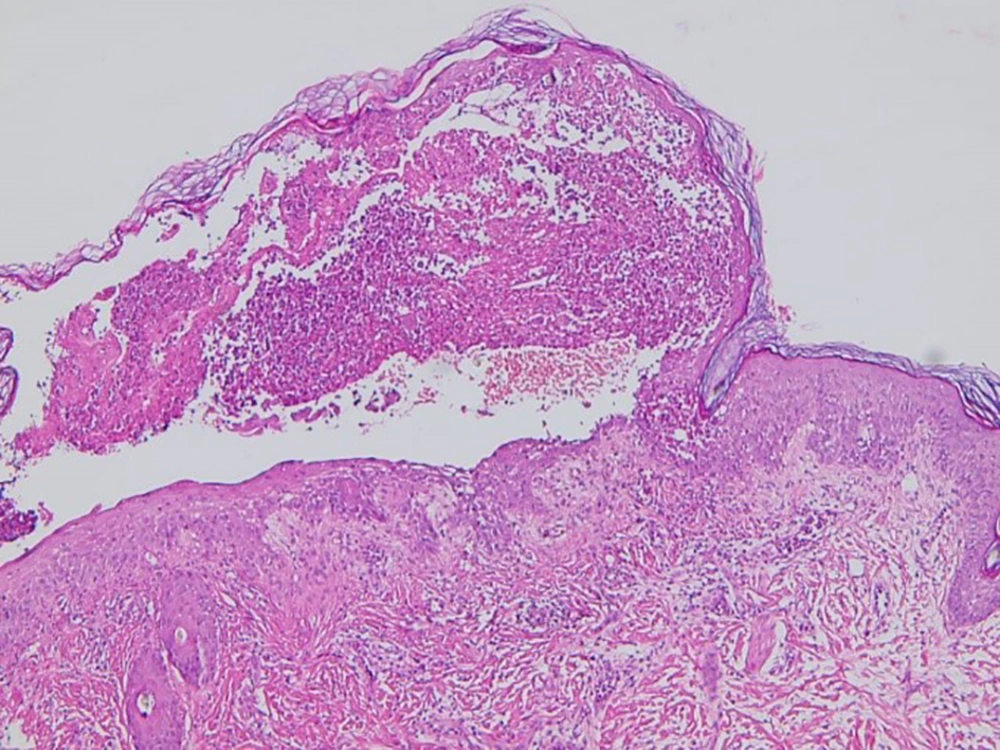
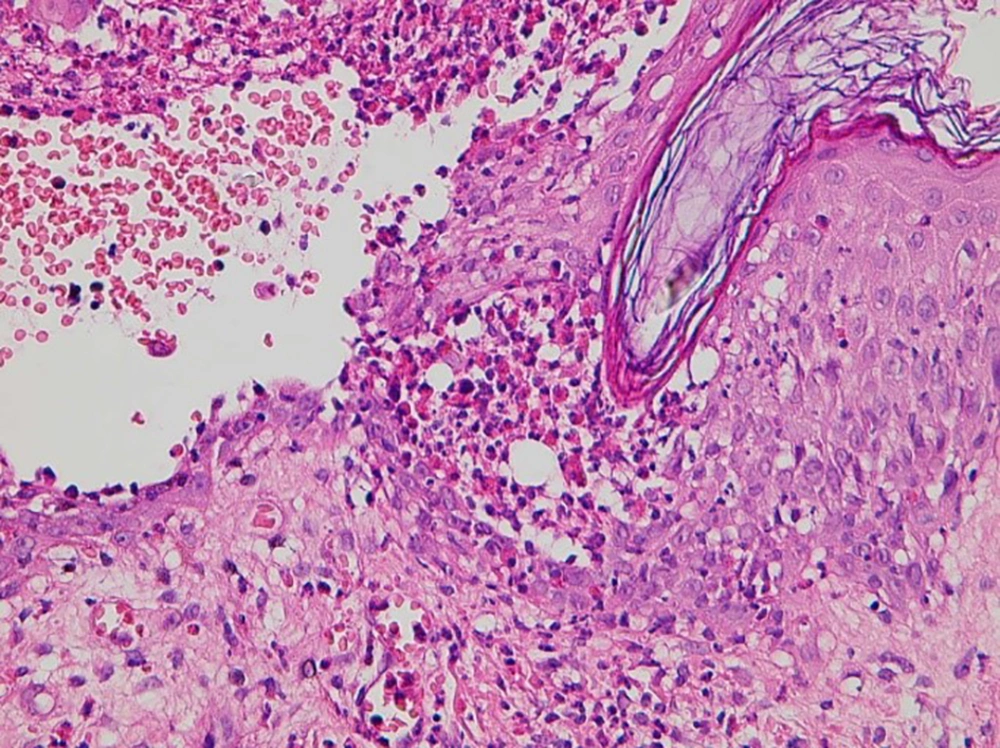
A detailed history-taking of the patient revealed similar skin blisters to the mother’s eruptions, initiated in the second trimester of pregnancy. After histopathological and immunofluorescence evaluations of the mother’s eruptions, a diagnosis of PV was made, and oral prednisolone was prescribed for the treatment. Based on the maternal history, our first diagnosis was a transient form of pemphigus in the neonate, acquired from the mother; skin biopsy also confirmed this diagnosis. Figures 4 and 5 showed the suprabasal blister, acantholysis, and inflammatory cell infiltrates in the histopathology evaluation of the skin lesion of our patient.
All other laboratory findings were in the normal ranges, with no evidence of systemic infectious diseases.
Because of the lack of secretion in the skin lesions, we could not collect a reliable bacterial culture from the skin eruptions. Since we did not have access to a polymerase chain reaction (PCR) in our hospital to detect herpes simplex virus (HSV), and the patient’s parents were uncooperative, we could not monitor this laboratory marker. During seven days of admission, his skin eruptions disappeared, and he was discharged from the hospital at the age of 10 days. The follow-up visit in the third month of life revealed suitable growth and development. Maternal disease was also controlled by corticosteroid therapy.
3. Discussion
In this case report, we described a neonate with pustular and bullous skin lesions in the first hours of life. Regardless of the maternal medical history, this type of skin eruption on the first day of the neonate’s life has differential diagnoses, such as neonatal HSV infection or bacterial skin infections caused by staphylococci, streptococci, listeria monocytogenes, as well as Gram-negative bacteria (4). Considering the early presentations of skin lesions (in the first day of life), co-occurrence of maternal infection (e.g., chorioamnionitis, PROM, or other infections) with early-onset sepsis is highly probable. However, the mother of our patient did not have a positive history of any infectious diseases during pregnancy.
The development of blistering and pustular skin lesions in the first days or weeks of life necessitates the neonate’s admission for a sepsis workup and administration of appropriate antimicrobial agents (5, 6). Regarding the probability of bacteremia, viremia, or systemic diseases, even with focal dermal involvement in the neonatal period, there is a risk of over-diagnosis and over-treatment in all nurseries and neonatal wards around the world (7). Although PCR and bacterial, fungal, or viral culture can help us determine the microbial cause of these skin lesions accurately, we did not have access to these laboratory tests, which is the limitation of our study.
Neonatal pemphigus is a rare disease, which presents soon after birth as cutaneous or mucocutaneous erosions. Besides the positive maternal history of PV, histological and immunofluorescence studies can confirm the diagnosis in neonates. These studies can help clinicians avoid other laboratory examinations and treatment modalities, such as prolonged antibiotic or antiviral therapies for microbial coverage, and prevent the prolonged hospital stay of neonates. Some inherited bullous disorders, such as EB and IP on the first day of life, are also important differential diagnoses for blistering eruptions in neonates (8). Incontinentia pigmenti, a lethal antenatal neurocutaneous disorder in male neonates, is only observed in a live female neonate with vesicular skin lesions and ophthalmologic, neurologic, and dental manifestations (9).
In this study, the maternal history of pemphigus during pregnancy helped us exclude differential diagnoses and prevented excessive evaluations. Skin biopsy and immunofluorescence assays confirmed the diagnosis of neonatal pemphigus in our patient. Similar to our case, Carvalho et al. also reported a male newborn with vesiculobullous lesions on the chest and abdomen, born to a mother with PV. This patient required no treatment, and supportive care was adequate (10). In another case report by Kodagali et al., a male newborn, born to a mother with pemphigus, presented with skin lesions who was recovered at the end of the first week of life with supportive therapy. The mother had developed oral pemphigus lesions eight months before pregnancy and was treated with oral steroid therapy (11).
In this regard, Guang-Wen Yin reported the case of a male neonate with blistering lesions on the neck, which appeared 10 hours after birth and distributed within 15 hours on the groin and perineum, with no mucosal involvement. Regarding the maternal history of similar lesions and diagnosis of pemphigus from four years ago (confirmed by histopathological and immunopathological examinations), no treatment was prescribed for this patient, and in the 30-day follow-up, all skin lesions disappeared (12). Unlike the mentioned case of blistering lesions, the pustular form was detected in our patient, and there were no blistering lesions.
3.1. Conclusions
For each neonate with pustular and blistering skin lesions on the first day of life, pemphigus should be considered as an important differential diagnosis. An accurate maternal history-taking may help eliminate the need for additional diagnostic and therapeutic measures.