1. Background
Sepsis is the third cause of death in the first month of life. A freshly cut cord is one of the entry points of bacteria for sepsis that can lead to neonatal death. Postpartum infection is a leading cause of newborn morbidity in undeveloped countries and the umbilical cord is an important source for sepsis. The most common umbilical cord problems are delayed separation and healing, bleeding, and swelling. The colonization of bacteria can also lead to omphalitis, cellulitis, thrombophlebitis, and even necrotizing fasciitis. Therefore, umbilical cord hygiene is essential, especially during the first week of birth (1, 2).
Bacterial colonization of the cord varies depending on the type of delivery and the place of hospitalization. The most common germs in vaginal deliveries are Escherichia coli, Group B streptococcus, Staphylococcus epidermis, Staphylococcus aureus, and Clostridium. In cesarean delivery, maternal skin flora, including Staphylococcus aureus and Staphylococcus epidermis, are more seen. In hospitalized neonates, Staphylococcus aureus, Gram-negative bacteria, and Klebsiella pneumonia are more common. In a home delivery, Gram-positive bacteria such as Staphylococcus epidermis and Clostridium are observed. In neonates with umbilical cord catheterization, coagulase-negative Staphylococcus is seen. Overall, the most common bacterium is Staphylococcus aureus (3).
There are different home strategies in developing countries to keep the cord clean. Some of them are harmful and some are useful by preventing the entry of bacteria. Agents used at home to keep the cord clean and prevent infection include alcohol, silver sulfadiazine, povidone-iodine, Eau de Dalibour, olive oil, sunflower oil, and human milk (4). Although the use of antibacterial agents can reduce cord infections, it can also cause the growth of resistant bacteria and increase the risk of neonatal infections (5). Due to different results obtained from the use of these agents, the World Health Organization recommends “dry cord care” and non-use of these compounds (2).
Skincare plays a crucial role in infants’ health. Bathing and cleansing of babies are of the most important issues after birth. Limited guidelines are available for skin health. In different countries with various cultures, use/non-use of bathing of neonates on the first days of birth, the best time of the first bath, use of soaps, and bathing intervals are different. Health workers, midwifery, mothers, and their relatives, especially grandmothers, in different societies have different points of view (6). There are different opinions for bathing the baby in the first days after birth. There have been many studies on the effect of bathing on infant skin hygiene, but the effect of bathing on umbilical cord hygiene has been rarely assessed.
2. Objectives
We decided to study the effects of bathing or not bathing on umbilical cord bacterial colonization, time to cord separation, antibiotics sensitivity, and cord complications to obtain evidence-based results to guide the best recommendations and practices in this regard to reduce parental concerns.
3. Methods
This quasi-experimental study assessed newborns and their mothers at Golestan hospital, Tehran, Iran, from February 2019 to January 2020. A convenience sampling method was used. The mothers who were willing to participate were included in the study. The inclusion criteria were healthy full-term babies and age of lower than 10 days. The exclusion criteria were low birth weight babies, maternal chorioamnionitis, premature rupture of the mother amniotic sac, existence of umbilical cord catheter, and antibiotic use during the study. Thus, 261 healthy full-term newborns were allocated to either of the study groups. Of 261 neonates, 21 were later excluded in the follow-up phase because they did not refer again to the hospital or used antibiotics during the study. Finally, 240 newborns completed the study. Mothers who believed in bathing in the first week of birth were allocated to one of the two groups. Group one (bath group, B) included neonates who were tub bathed with water once every two days (n = 90). Group two (clean product group, CP) included newborns who were bathed with cleaning agents (liquid baby shampoo) every two days (n = 87). The first bath began on the second day after birth, and there were four baths in total for each neonate. Mothers who did not believe in bathing before the umbilical cord separation were allocated to the third group (dry care cord, D). Their neonates were not bathed during the first days and only performed dry care cord (n = 63). A questionnaire including socioeconomic demographic information and cord clinical findings were prepared and completed on the phone once in every two days after discharge from the hospital. On the 10th day, mothers and their babies returned to the hospital laboratory, and umbilical cord swabs were done. A direct surface sampling method was used. A wet swab head was rubbed and rolled on the sampling area, then returned into the tube and labeled. Swabs were cultured in blood agar, and Eosin Methylene Blue (EBM) agar and bacterial sensitivity tests were done by disk diffusion.
3.1. Main Outcome Measure
The time of cord separation, bacterial colonization, antibiograms, and omphalitis were studied as the study outcomes. Omphalitis was defined based on redness, discharge, swelling, and tenderness around the umbilical cord (1).
3.2. Statistical Analyses
Data were analyzed by SPSS version 24 software (SPSS Inc., Chicago, IL, USA). The mean and standard deviations for quantitative variables, and the frequency and percentage for qualitative variables were calculated. The statistical analyses were done by the Student t-test for data on cord separation time and the Pearson Chi-square test for data on bacterial colonization, antibiograms, and omphalitis. P value < 0.05 was considered significance.
3.3. Ethical Considerations
In all stages of the study, ethical issues were observed, and the name and information of the participants were kept confidential.
4. Results
The mean age of the mothers was 27 ± 1.83 years. The majority of the mothers were primiparous (group B, 68.9%; group CP, 65.6%; group D, 76.1%). About one-third of them were employed, and most of them had a diploma degree (group B, 88.9%; group CP, 88.5%; group D, 95.2%). In terms of economic level, most of them were at a moderate level (group B, 81%; group CP, 80.4%; group D, 73%). The moderate economic status (4-7th deciles) included the monthly income of about 40000-70000 thousand Rials, according to the report of the central bank of Iran (https://www.cbi.ir and https://www.amar.org.ir). In terms of the type of delivery, there were 216 cesarean sections and 24 vaginal deliveries. Newborns were 121 boys and 119 girls. The demographic characteristics of the subjects were similar in the groups. The details are shown in Table 1.
| Variable | Group B (n = 90), No. (%) | Group CP (n = 87), No. (%) | Group D (n = 63), No. (%) | P Value |
|---|---|---|---|---|
| Mothers’ age years, (mean ± SD) | 26 ± 2 | 2 8± 1.5 | 27 ± 2 | 0.73 |
| Employed | 27 (30) | 29 (33) | 18 (28) | 0..81 |
| Education of mothers | 0.22 | |||
| Higher education | 9 (10) | 10 (11.5) | 2 (3.2) | |
| Diploma | 80 (88.9) | 77 (88.5) | 60 (95.2) | |
| Read and write | 1 (1.1) | 0 (0) | 1 (1.6) | |
| Parity | 0.12 | |||
| Primiparous | 62 (68.9) | 57 (65.6) | 48 (76.1) | |
| 2 - 4 | 28 (31.1) | 29 (33.3) | 14 (22.3) | |
| > 4 | 0 (0) | 1 (1.1) | 1 (1.6) | |
| Socioeconomic status | 0.53 | |||
| Good | 7 (7.8) | 8 (9.2) | 5 (8) | |
| Moderate | 73 (81) | 70 (80.4) | 46 (73) | |
| Low | 10 (11.2) | 9 (10.4) | 12 (19) | |
| Delivery | 0.61 | |||
| Cesarean section | 80 (88.9) | 81 (93) | 55 (87) | |
| Vaginal delivery | 10 (11.1) | 6 (7) | 8 (13) | |
| Gender | 0.78 | |||
| Boy | 45 (50) | 44 (50.6) | 32 (50.8) | |
| Girl | 45(50) | 43 (49.4) | 31 (49.2) |
Abbreviation: SD, standard deviation. Group B = tub bath; Group CP = bath with the clean product; Group D= dry clean care (without bath). Positive cultures were not significantly related to age, parity, employment, education, and type of delivery of mothers, as well as the gender of neonates (P > 0.05). However, economic status had a significant relationship (P = 0.001).
The mean time to umbilical cord separation was 8.2 days with a standard deviation (SD) of 1.74. This period was 9.1 ± 2.1 days for group B, 8.7 ± 1.82 for group CP, and 6.8 ± 1.3 days for group D. The time to cord separation was shorter in group D than in the other two groups, which was statistically significant (P = 0.048) (Table 2). Only two cases of omphalitis were seen, including one in group CP (1.15%) and one in group D (1.6%), which showed no statistical difference between the three groups (P = 0.83) (Table 2).
| Variable | Group B | Group CP | Group D | P Value |
|---|---|---|---|---|
| Cord separation time (day)±SD | 9.1 ± 2.1 | 8.7 ± 1.82 | 6.8 ± 1.3 | 0.048 |
| Omphalitis (n, %) | 0 (0) | 1 (1.15) | 1 (1.6) | 0.83 |
Abbreviation: SD, standard deviation. The time to cord separation was significantly shorter in group D than in the other two groups (P < 0.05).
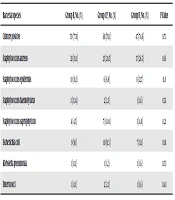
Positive culture and colonization rates were not significantly related to maternal age, parity, employment, education, type of delivery, and neonate gender (P > 0.05). However, bacterial culture was significantly related to economic status (P = 0.001). Positive culture rates were 77.8% in group B, 78.1% in group CP, and 74.6% in group D, which showed no significant differences between the three groups (P = 0.073). Bacterial species isolated in each group are shown in Table 3. Staphylococcus aureus was the most common species in the three groups (group B, 31.1%; group CP, 28.5%; and group D, 26.5%), which were not significantly different between the three groups (P = 0.061). Staphylococcus epidermis and Escherichia coli were the other most common species.
| Bacterial species | Group B, No. (%) | Group CP, No. (%) | Group D, No. (%) | P Value |
|---|---|---|---|---|
| Culture positive | 70 (77.8) | 68 (78.1) | 47 (74.6) | 0.73 |
| Staphylococcus aureus | 28 (31.1) | 25 (28.5) | 17 (26.5) | 0.61 |
| Staphylococcus epidermis | 10 (11.1) | 6 (6.9) | 8 (12.7) | 0.8 |
| Staphylococcus haemolyticus | 3 (3.34) | 2 (2.3) | 1 (1.6) | 0.51 |
| Staphylococcus saprophyticus | 4 (4.5) | 7 (8.04) | 3 (4.8) | 0.21 |
| Escherichia coli | 9 (10) | 10 (11.5) | 7 (11.1) | 0.81 |
| Klebsiella pneumonia | 1 (1.11) | 1 (1.2) | 1 (1.6) | 0.53 |
| Enterococci | 1 (1.11) | 2 (2.3) | 1 (1.6) | 0.43 |
aIn all cultures collected, mixed species were seen in 25.51% and one species in 51.29%. Staphylococcus aureus was the most common species in the three groups, which showed no statistically significant differences between the three groups (P > 0.05). Staphylococcus epidermis and Escherichia coli were the other most common species.
Staphylococcus aureus was sensitive to vancomycin (91%), cyprofloxacilin (89%), amikacin (71%), chephalexin (69%), and ceftizoxim (61%). Staphylococcus epidermis was sensitive to vancomycin (89%), cyprofloxacilin (74%), amikacin (60%), chephalexin (59%), and ceftizoxim (49%). Escherichia coli was sensitive to cyprofloxacilin (87%), amikacin (90%), chephalexin (13%), and ceftizoxim (84%). Klebsiella pneumonia was sensitive to cyprofloxacilin (76%), amikacin (92%), chephalexin (61%), and ceftizoxim (92%). Enterococci were sensitive to vancomycin (88%), cyprofloxacilin (26%), chephalexin (7%), and ceftizoxim (42%).
5. Discussion
Bathing of neonates on the first days of birth, the best time of the first bath, the use of soaps, and bathing intervals are different in different countries. Due to the importance of bacterial colonization on the umbilical cord and its infection, we studied the effects of bathing or not bathing on umbilical cord separation time, bacterial colonization, antibiotics sensitivity, and omphalitis. The time to cord separation was shorter in group D than in the other two groups, but positive cultures were not significantly different between the three groups.
Dermatologists and pediatricians do not have the same opinion about babies’ skin health, and different views have been reported. They believe that bathing with immersion in tub water is better than washing (dip the cotton wool in the water and wipe gently around the face, neck, hands, and bottom) (7). However, a systematic review showed that washing with wet cotton is a safe practice that better acts than bathing in tub water for skin hygiene. Using mild liquid cleaners would be better than water alone (8). However, a study showed that water bathing with or without liquid cleaners made no difference in neonatal skincare (9). On the other hand, qualitative research in some cultures showed that water alone was more acceptable for mothers in neonates skincare than emollients such as sunflower and olive oil, and there was no advantage for using these agents (10).
Less than 5% of neonates in a study in Bangladesh and more than 10% of neonates in a study from Malawi were never bathed in the first days, which were related to their socioeconomic status (11). In our study, mothers who did not believe in bathing their newborns in the first week of birth were very few. It took about a year for group D (no bathing) to collect, but the other two groups were collected quickly. Concerning demographic factors, only the socioeconomic status was significantly related to bacterial cultures.
The effects of bathing with water alone and bathing with cleansers twice a week were studied on dryness and transdermal water loss. The study showed that the rate of dryness was lower in the first group (12). However, our study assessed the effect of water bathing with/without cleaners and dry care without bathing on bacterial colonization and time to cord separation.
A study in Iran was carried out on the effect of alcohol (n = 94) and Eau de Dalibour (n = 84) on umbilical separation time and omphalitis. Separation time was 6.3 ± 1.82 days in the first group and 4.04 ± 1.61 days in the group of Eau de Dalibour, which showed a significantly shorter time. There was no case of omphalitis. Bacterial colonization was not evaluated in this study (13). On the other hand, our study assessed the effects of dry care and water bath on 240 babies on the separation time and bacterial culture of the cord. The time to umbilical cord separation was 6.8± 1.3 days in the dry care group, which is consistent with the results of the alcohol group of the above study. Also, we observed two cases of omphalitis, although it did not show statistically significant differences between the three groups.
In another study in Spain, the mean of cord detachment time was 6.61 ± 2.33 days in dry care, which is consistent with the results of our study. Omphalitis was seen in 3.7%, but in the present study, it was 1.6% (14). Erenel et al. in Turkey studied the effect of olive oil and dry care on cord separation time. They showed that the average time was 9.46 days (olive oil: 9.1 days; dry care: 9.8 days), with no significant difference. Bacterial culture was seen in 35.9% in the olive oil group and 33.5% in the dry care group (15). In our study, the average time was 8.2 ± 1.74 days. The separation time was 6.8±1.3 days in the dry care group, and positive culture was seen in 74.8%. We also studied the effect of bathing with or without cleaners on the rate of positive culture and cord detachment, which was not performed in the mentioned study.
Quinn et al. in the USA studied bathing once every two days (n = 28) versus every four days (n = 25) in preterm babies. They found that skin flora and colony counts were similar in the two groups (16). In a similar study in Korea, 32 preterm neonates were studied, and their results were similar to the Quinn study (17). But in our study, bathing was performed every two days in 177 term healthy neonates in the first two groups, and we assessed the cord flora, as well.
Group B streptococcus is usually found in vaginal delivery, especially in premature infants (18). But in our study, it was not observed. This may be due to that we studied only term infants; another reason may be that the number of vaginal deliveries was low in the present study (24/240; 10%). Rush studied the Staphylococcus aureus colonization rate in the umbilical cord in two groups of daily baths with water and soap (n = 95) and a no-bath group (n = 86). There were no statistical differences between the two groups. The colonization rates were 38% and 41% in the two groups, respectively. However, the rate of colonization was higher in cesarean sections (59%) than in vaginal deliveries (9%) (19). But our study was done in three groups, and bathing without cleaners was also studied. The Staphylococcus aureus colonization rates were 28.5% and 26.5% in the water bath with cleaners and no-bath groups, respectively. The colonization rates were not statistically different between the groups, which was in line with the results of the above study.
In another study in Turkey, bacterial cord colonization was not significantly different between the three groups: group A, dry care; group B, 70% alcohol and group C, 10% povidone-iodine; the most common bacterial cultures were Staphylococcus aureus, Escherichia coli, and enterococci (20). The effect of a water bath with or without cleaners on cord culture was not studied. In our study, the most common bacteria in the dry care group were Staphylococcus aureus, Staphylococcus epidermis, and Escherichia coli. Also, enterococci were seen only in 1.6% of the cultures.
As mentioned above, the umbilical cord is a good place for bacterial growth. The recommendation of the World Health Organization is “dry cord care” and the non-use of any agents (2). Skincare plays an important role in infants’ health. Bathing of babies is one of the most important issues after birth. Bathing or not bath of neonates on the first days of birth, the best time of the first bath, the use of soaps, and bathing intervals are different in different countries, and there are no standard guidelines for them.
One of the limitations of this study was the low number of vaginal deliveries that may be effective in the rate and type of bacterial species in the umbilical cord. Umbilical cord swabs were only done on the 10th day. Due to the possibility of non-cooperation and concerns of parents, we took one sample at the end of the 10 day. It was very difficult to get parental consent, and if repeated sampling was done, they might be worried about their babies.
In conclusion, any suggestion should be simple, easy to use, practical, low-cost bearing, and evidence-based to reduce parental concerns and be psychologically acceptable to parents and babies. No-bath and water bath with or without cleaners had no difference in the rate and type of bacterial culture in umbilical cord but the cord separation time was shorter in the no-bath group. Therefore, if a mother does not believe in bathing her baby, she should not be denounced and told that she did something wrong with the umbilical cord hygiene. In addition, most mothers tend to bathe, which may reduce parental concerns and bring psychological benefits for parents and babies. Bathing with or without cleaners is safe. However, the results should be confirmed by further studies.