1. Introduction
The novel coronavirus, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which causes severe acute respiratory syndrome, was first identified at the end of 2019 (1). Initially, there was no evidence about coronavirus disease 2019 (COVID-19) infection in pediatrics (2). However, over time, children infected with COVID-19 were reported in various areas (3, 4).
According to the European Centre for Disease Prevention and Control (ECDC) and (5) Iranian Pediatric Association statement (6), a probable COVID-19 case is a patient with signs and symptoms of COVID-19 plus chest imaging is in accordance with COVID-19; however, the result of polymerase chain reaction (PCR) is inconclusive.
In April 2020, the World health organization (WHO) announced new criteria for diagnosing an illness that was observed among pediatric cases with COVID-19, named the Multisystem inflammatory syndrome in children (MIS-C). Some children with MIS-C have the signs and symptoms of complete or incomplete Kawasaki disease.
In the present study, we reported three pediatrics cases with the signs and symptoms of Kawasaki and their three-month follow-up.
2. Case Presentation
2.1. Case 1
An 11-years-old boy with a history of fever and diarrhea lasting for six days was admitted to the pediatric COVID-19 center. On admission, he was suffering from coughing and fever. Physical examination revealed tachypnea (36 times per minute) and low oxygen saturation (91% in room air). Laboratory tests showed lymphopenia and high C-reactive protein (CRP).
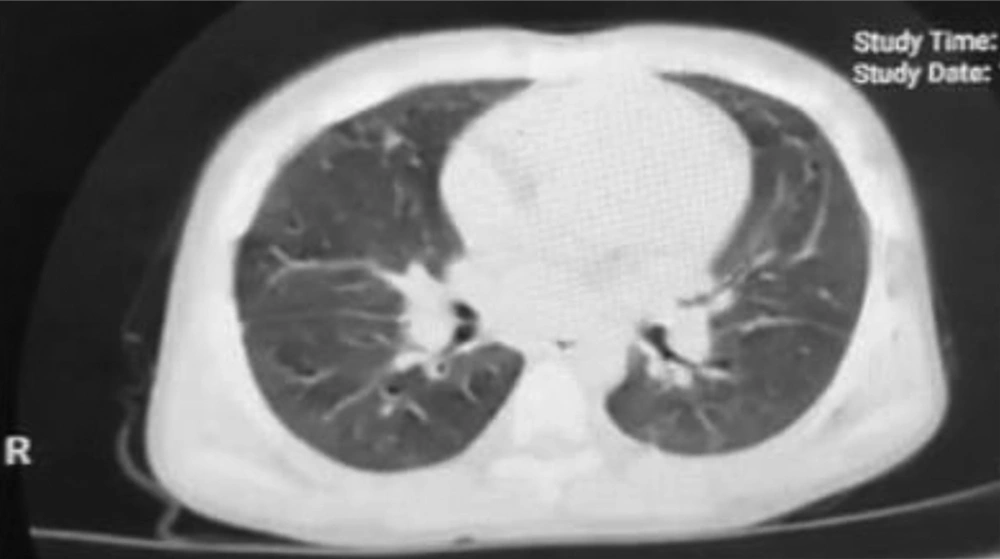
Based on the chest CT scan (Table 1 and Figure 1) as well as history and physical examination, he was triaged as a probable COVID-19 case. Therefore, following the Iranian Pediatric Association statement, he was treated with hydroxychloroquine and Lopinavir/Retinovir (5). On the second day of admission, physical examination showed nonpurulent bilateral conjunctivitis, maculopapular rashes on the trunk, red strawberry tongue, and severe nonpitting edema on his feet (Figure 2). Considering lab data and the presented signs, the patient was diagnosed with complete Kawasaki, and intravenous immunoglobulin (IVIG) and high-dose aspirin (ASA) were administered (7).
| Findings | Case 1 | Case 2 | Case 3 |
|---|---|---|---|
| Age | 11 years old | 9 months old | 14 months old |
| Sex | Male | Female | Female |
| Physicalexamination | |||
| PR | 100 | 110 | 110 |
| RR | 36 | 40 | 45 |
| O2sat | 91% | 95% | 94% |
| T | 38c | 38.7 | 38.9 |
| CRT | < 2 second | < 2 second | < 2 second |
| AVPU | A | A | A |
| Ability to drink | Good | Good | Good |
| Labdata | |||
| Lymphocyte (%) | 7.8 | 6, 25 | 17.3 |
| Hb | 12 | 11, 9.4 | 9.7 |
| PLT | 173000 | 592000, 521000 | 599000 |
| AST | 49 | 56, 137 | 83 |
| ALT | 18 | 37, 184 | 55 |
| Alb | 2.8 | 3, 3 | 3.5 |
| Na | 123 | 134, 132 | 126 |
| CRP | 23 | 183, 97 | 50 |
| ESR | 64 | 55, 46 | 66 |
| U/A(WBC) | 5 | 0, 0 | 0 |
| Echocardiography | Minimal MR, TR, pericardial effusion | Mild MR, TR, PI | Normal |
| Imaging | |||
| One side involvement | - | - | _ |
| Two side involvement | + | + | + |
| Ground glass opacity | + | + | + |
| Subpleural opacity | + | + | + |
| Consolidation | - | - | _ |
| Hallo sign/ Reverse hallo sign | - | - | - |
| Micro nodules | - | - | _ |
| Crazy patching | - | - | _ |
Abbreviations: PR: pulse rate, RR: respiratory rate, BP: blood pressure, O2 sat: oxygen saturation CRT: capillary refill time, AUPU: a scale for recording the patient's level of consciousness, WBC: white Blood cells, PLT: platelet, AST: Aspartate aminotransferase, ALT: Alanine aminotransferase, Alb: albumin, ESR: erythrocyte sedimentation, CRP: C-reactive protein, U/A: urine analysis, MR: mitral regurgitation, TR, tricuspid regurgitation, PI: pulmonary regurgitation
The echocardiography for the first time showed mild mitral and tricuspid regurgitation plus pericardial effusion. Seven days later, the echocardiography revealed right atrium and ventricle enlargement with good ejection fraction. Although our patient was admitted before April, according to the currently available guidelines, it can be said that he had MIS-C, mainly because of diarrhea, skin manifestations, and cardiac involvement with the presentation of typical Kawasaki. On follow-up examinations, the peeling was considerable (Figure 2) on the 10th day of illnesses. On the 15th day, the left coronary artery (LCA) ectasia was seen and the enlargement of the right side was the same as the 7th day. Low-dose ASA was continued until the third month after the admission until echocardiography became normal. After two months, the COVID-19 IgG titer was 1.8 with an index > 1.
2.2. Case 2
A 9-months-old girl presented to the pediatric COVID-19 center with a complaint of two days of fever and cough. Her mother was among the health staff of the center. The mother had a fever and cough one week ago. Her physical examination showed fever (38.2) and tachypnea (40 times per minute). Leukocytosis with lymphopenia, normochromic normocytic anemia, high level of CRP, and erythrocyte sedimentation rate (ESR) were detected in the lab study (Table 1). According to signs, symptoms, and chest CT scan, she was a probable COVID-19 case (Figure 3), (6). Therefore, she was treated with hydroxychloroquine (6).
On the 3rd day of her illness, nonpurulent bilateral conjunctivitis plus maculopapular rushes were the main signs observed on physical examination. On the 4th day of fever, because of previous signs, echocardiography was performed, and lab tests were repeated. Moderate mitral regurgitation, tricuspid, and pulmonary regurgitation were the echocardiography findings. She was treated with IVIG and high-dose ASA as a case of incomplete Kawasaki (7). According to new data, she was also a case of MIS-C with a presentation of atypical Kawasaki because of skin and cardiac manifestation. On the follow-up examination, echocardiography revealed LCA ectasia on the 15th day of follow-up, and on the 30th day, the right heart size was enlarged. After three months, the ectasia was improved, but the enlargement was persistent, and low ASA was continued. The parents of the child did not allow us to check the COVID-19 IgM and IgG antibodies.
2.3. Case 3
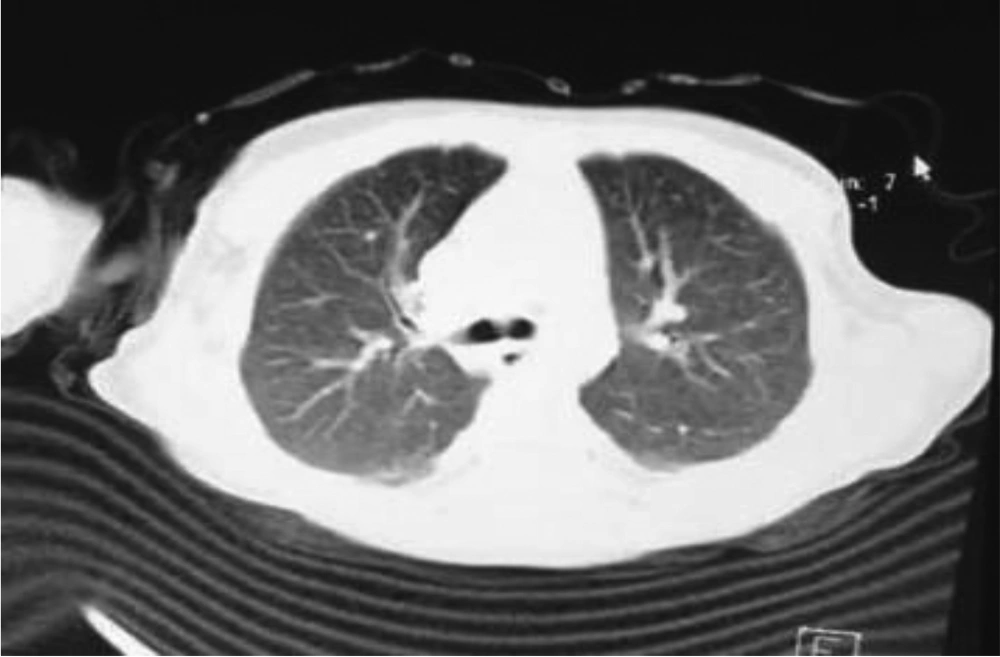
A 14-months-old boy presented with a history of five days of fever and rhinorrhea. The physical examination revealed tachypnea (45 times per minute), normal oxygen saturation in the air room (93%), bilateral nonpurulent conjunctivitis, maculopapular rashes in his feet and hands, strawberry tongue, and edema of hands and feet. The laboratory tests showed Lymphopenia, high levels of CRP, ESR, and alanine aminotransferase (ALT) (Table 1). Hence, he was treated as a probable case of COVID-19 similar to Kawasaki disease (Figure 4), (7) with high-dose ASA and IVIG. Nevertheless, the echocardiography was normal. The patient was discharged after six days with a good health condition. Unfortunately, when we called them for follow-up a week later, the parents told us he died three days after discharge at home.
3. Discussion
COVID-19 is a pandemic disease caused by the novel coronavirus, named SARS-CoV-2. The sensitivity of PCR is not high (8). The Iranian Pediatric Infectious Diseases Society, in its statement on COVID-19 management, defined a probable COVID-19 case as follows: when laboratory and imaging findings are in accordance with COVID-19 but the nasopharyngeal PCR for SARS-CoV-2 is negative. The exact cause of Kawasaki disease is not clear yet, and further studies are needed.
Infection agents, such as retroviruses and parvovirus B19, can cause Kawasaki disease (9, 10). In 2005, Esper et al., in a case-control study, reported an association between coronaviruses and Kawasaki disease (11). The acute onset of Kawasaki disease and its wavelike spread reported in winter can indicate the Kawasaki disease caused by infectious diseases (12).
Another study has mentioned the expansion of CD8 lymphocytes as one of the pathogeneses of Kawasaki due to infectious diseases (13). It has been demonstrated that patients infected with COVID-19 have lower levels of CD8 lymphocyte (14); however, the exact cause is not clear, and further studies are needed. Some studies have reported that SARS-CoV-2 can cause capillary inflammation and endothelial dysfunction in many organs, such as kidney and skin (15). Therefore, the manifestation of Kawasaki disease may be due to this capillary inflammation. After time passed from April 2020, some studies have been conducted on the pathophysiology of SARS-CoV-2 and MIS-C and Kawasaki features of this syndrome. Children with a special genetic variant in regulatory T and B cells, which destroys the immune complex, have a higher chance of suffering from MIS-C with Kawasaki features (16).
Apart from the pathophysiology of this syndrome, the effect of this inflammatory process in different organs is important. In the introduced cases, two of three patients reported normal heart function after three months. Case 3 died. Thus, follow-up of the patient's organs function, especially cardiac follow-up after discharge, is suggested. Recording the data of these patients is helpful to understand the long-term follow-up effect of this inflammatory process in different organs of children and indicate the times of different organ evaluation by the physician in pediatric patients with MIS-C.