1. Introduction
Coronavirus disease 2019 (COVID-19), causing acute pneumonia, has become a public health threat to people all over the world. It has been shown uncommon in children (1). Due to the lower prevalence in children, the current information on children is limited, which makes its diagnosis and treatment challenging in this group. Clinical manifestations of COVID-19 in children were generally less severe than those of the adult patients (2). Some patients are asymptomatic and accidentally diagnosed. In this case report, we described a 12-year-old patient suffering from chickenpox and COVID-19 pneumonia simultaneously. The patient’s consent was obtained for this study.
2. Case Presentation
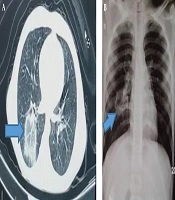
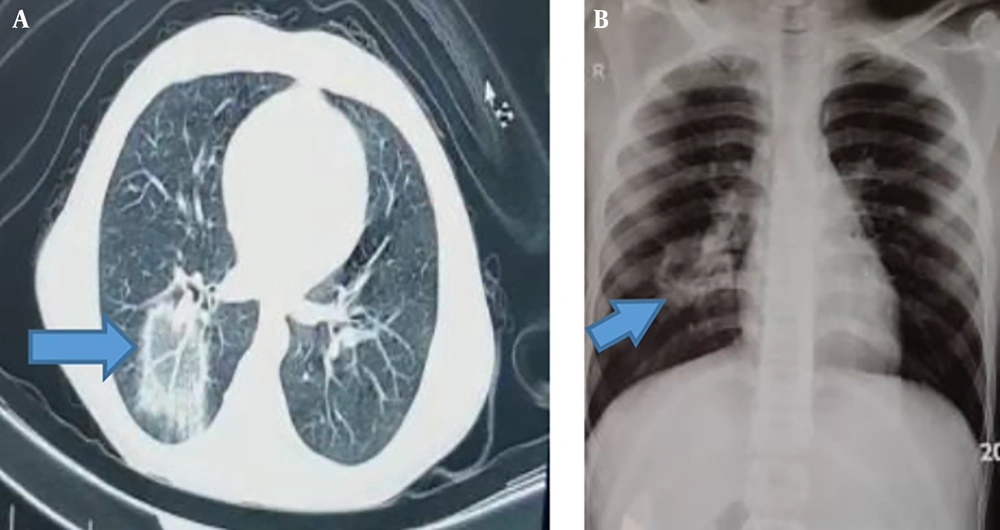
The patient was a 12-year-old boy with no underlying disease and with a normal body mass index Z-score. He had the symptoms of fever (body temperature of 40°C in physical examination), skin lesions, and mild respiratory symptoms, like dry coughs and chest discomfort. These symptoms were started simultaneously and became severe gradually. The skin lesions were diffuse papulovesicular itchy lesions (predominance of vesicles) localized into the trunk, face, and limbs. He had no history of taking new medications for the previous 15 days and also previous varicella-zoster virus (VZV). Due to the typical lesions (macular, popular, and vesicular) and history of contact with a chickenpox patient a few days ago, chickenpox was clinically diagnosed. Treatment with acetaminophen and acyclovir was done on an outpatient basis in a rural medical center. Ten days later, the patient referred to the Mofid Children’s Hospital due to persistent fever and severe respiratory symptoms, such as chest pain and severe dry coughs. Because of the COVID-19 epidemic, the patient was suspected of COVID-19 infection. The nasopharyngeal specimen tested by polymerase chain reaction (PCR) test was positive for COVID-19 and did not reevaluated because of a limitation in equipment. IgM and IgG antibodies response against COVID-19 was measured by enzyme-linked immunosorbent assay (ELISA), and the results were positive for IgM (5.8) and negative for IgG (0.1). The VZV infection was confirmed by measuring IgM and IgG antibodies against varicella virus (ELISA) and was positive. The patient’s parents refused a skin biopsy. The important laboratory results are available in Table 1. A radiologic evaluation was done. The finding of the CT scan was a focal centrally located parenchymal infiltration with reverse halo sign (RHS) in the right lower lobe along with engorged vessels within the parenchymal lesion. The chest x-ray finding was mass-like opacity with central lucency in the right middle zone. These radiographic findings were suspicious of COVID-19 (Figure 1).
| Results | |
|---|---|
| WBC | 3.8 × 105 (neut: 45.7%, lymph: 40.7%) |
| Hb, mg/dL | 11.9 |
| Plt | 233000 |
| ESR | 8 |
| CRP | 33 |
| LDH | 394 |
| CPK | 154 |
| LFT, Electrolytes and biochemistry | Normal |
| COVID-19 IgM (EIA) | 5.8 (positive > 1.1) |
| COVID-19 IgG (EIA) | 0.1 (negative < 0.9) |
| VZV Ab (IgM) (EIA) | 10.6 (positive) |
| VZV Ab (IgG) (EIA) | 20.8 (positive) |
We suspected to atypical pneumonia and COVID-19 infection; therefore, treatment with azithromycin and hydroxychloroquine was started. He was discharged a few days later with significant improvement of general condition. After a ten-day follow-up, all symptoms disappeared.
3. Discussion
The occurrence of multiple virus infections in a patient is not an unusual finding, but this condition is more common in patients with primary or secondary immunodeficiencies (3). Varicella is an acute febrile rash illness that was common in children. The diagnosis of varicella is made primarily by the typical clinical presentation. The complications of VZV infection occur with varicella, more commonly in immunocompromised patients. Pneumonia is a serious and rare complication of varicella (4).
Cutaneous manifestations associated with COVID-19 have been recently reported. In an Italian study, 20.4% of the COVID-19 patients had cutaneous manifestation. These manifestations were erythematous rash (15.9%), widespread urticarial (3.41%), and chickenpox-like vesicles (1.4%). Skin manifestations are similar to other cutaneous involvements occurring during common viral infections (5). Genovese et al. (6) (Italy) reported an 8-year-old girl with COVID-19 infection and chickenpox-like skin manifestations. This patient had a history of chickenpox infection a few years ago. Skin biopsy and serological tests for VZV were not carried out in this case. Although their results do not prove that this rash is caused by or definitively associated with COVID-19, they suggest that papulovesicular eruptions are included in the spectrum of exanthems possibly associated with COVID-19 (6). A case series of 22 patients (21 adults and one child) with varicella-like exanthema associated with COVID-19 was reported by an Italian dermatologist. Its typical features were frequent trunk involvement, usually scattered distribution, and mild/absent pruritus. Demonstration of SARS-CoV-2 presence by PCR in lesional skin was not possible because of specific primer unavailability. They did not perform the serological or microbiological evaluation for detecting VZV infection (7).
In justifying the concomitant occurrence of these two diseases, we have three hypotheses. (1) It can be inferred that VZV infection causes a secondary immunodeficiency and predisposes the patient to COVID-19 pneumonia; (2) Frequent hand-to-face contact due to itchy lesions has predisposed the patient to the COVID-19 disease; and (3) The coincidence of these two diseases was accidental. The VZV infection in children aged over 12 years may cause serious infection and must be treated with antiviral medications. It should be considered that COVID-19 may be presented with varicella-like manifestation or be concomitant with chickenpox infection. The lesions associated with COVID-19 are less itchy and are mostly found in trunk and limbs and rarely in the face. History of previous VZV infection and performing the post-immunization serological test may help to diagnose VZV infection.
The most common imaging finding in COVID-19 is multifocal peripheral ground-glass opacity in the lungs on CT scan. Other features include consolidation, interlobular septum thickening, a crazy-paving pattern as a signal of progressive disease, and RHS. Vascular enlargement with parenchymal lesion has also described in COVID-19, but it is rare. Pleural effusion, pericardial effusion, and lymphadenopathy (LAP) are rare in COVID-19 and suggest bacterial superinfection or another diagnosis (8). The RHS is characterized by a central ground-glass opacity surrounded by a ring of consolidation on high-resolution CT. RHS has been reported in association with a wide range of pulmonary diseases, including invasive pulmonary fungal infections, paracoccidioidomycosis, pneumocystis pneumonia, tuberculosis, community-acquired pneumonia, lymphomatoid granulomatosis, Wegener granulomatosis, lipoid pneumonia, and sarcoidosis. It is also seen in pulmonary neoplasms and infarction, as well as following radiation therapy and radiofrequency ablation of pulmonary malignancies (9).
Our patient had two rare manifestations of COVID-19 infection simultaneously, RHS and vascular enlargement, which are not seen in varicella pneumonia, Other CT scan findings are uncommon for varicella pneumonia, as well. COVID-19 was confirmed in this patient by RT-PCR and serological test.