1. Introduction
In December 2019, a disease presented mostly by respiratory symptoms begun to spread around the world from Wuhan, Hubei Province, China. The World Health Organization announced “COVID-19” as the name of this new disease (COVID-19). It causes by severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) (1).
According to case series on pediatrics infected with SARS-CoV-2, common symptoms of COVID-19 in children are fever, dry cough, and dyspnea (2). Meanwhile, some epidemiological studies have also mentioned to gastrointestinal symptoms, including diarrhea, vomiting, gastrointestinal bleeding, and abdominal pain (3). According to the best knowledge of the authors, this is the first case report in children with acute abdomen signs.
In this article, we reported four children infected with COVID-19 who, during their hospital stay, developed acute abdominal pain, which led to the diagnosis of acute abdomen.
2. Case Presentation
To observe ethical principles, written informed consent was obtained from parents of children who participated in the current study. Also, the privacy of the participants was respected.
2.1. Case 1
A four-month-old boy with a history of hospitalization due to severe pneumonia who was using bi-level positive airway pressure (BiPAP) machine developed fever, poor feeding, and dyspnea (Table 1). His arterial oxygen saturation was 75% (Table 2).
| Parameters | Case 1 | Case 2 | Case 3 | Case 4 |
|---|---|---|---|---|
| Age | 4 months | 10 years | 5 years | 45 days |
| Sex | Boy | Boy | Girl | Boy |
| Fever | Yes | No | Yes | No |
| Abdominal signs and symptoms | Abdominal tenderness and bilious vomiting | Abdominal pain, tenderness and guarding | Abdominal pain, tenderness and guarding and vomiting | Oral intolerance, abdominal distention and irritability |
| Imaging finding | Coffee-bean view in X-ray | Appendicitis in ultrasonography | Appendicitis in ultrasonography | Coffee-bean view in X-ray |
| Parameters | Case 1 | Case 2 | Case 3 | Case 4 |
|---|---|---|---|---|
| PR, /min | 123 | 120 | 110 | 162 |
| RR, /min | 38 | 30 | 28 | 45 |
| O2 sat with BIPAP, % | 92 | 96 | 96 | 98 |
| Axillary temperature, °Celsius | 37.5 | 36.8 | 37.7 | 37 |
| CRT, s | < 2 | < 2 | < 2 | < 2 |
| AVPU | A | U | A | A |
| Ability to drink | Not good | Not good | Good | Not good |
Abbreviations: AVPU, a scale to record level of consciousness including alert (A), verbal (V), pain (P), unresponsive (U); CRT, capillary refill time; O2 sat, oxygen saturation; PR, pulse rate; RR, respiratory rate.
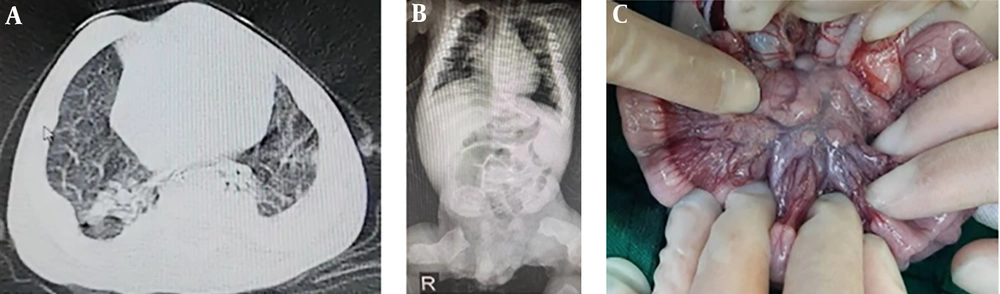
He was suffering from ontogenesis imperfecta and had a history of contact with a COVID-19 confirmed case while hospitalized at the pediatric intensive care unit (PICU). Physical examination revealed subcostal retraction and crackle in both lungs. Laboratory examination showed increased LDH and decreased hemoglobin concentration, while other tests were normal (Table 3). The diagnosis of COVID-19 was confirmed by detection of SAR-CoV-2 RNA and typical lesions in the chest after performing computed tomography (CT) (Figure 1). Following the Iranian pediatric protocol, he was treated with hydroxychloroquine and lopinavir/ritonavir. During the hospitalization, a new-onset abdominal tenderness and bilious vomiting appeared. The abdominal X-ray showed a coffee-bean view in the left upper quadrant (Figure 1). By considering signs and symptoms, the patient underwent laparotomy with suspicion of volvulus. Laparotomy revealed several large lymph nodes in the peritoneum (Figure 1).
| Markers | Case 1 | Case 2 | Case 3 | Case 4 |
|---|---|---|---|---|
| WBC count, cells/µL | 5500 | 11400 | 6100 | 14000 |
| Lymphocyte percent, % | 58.9 | 27 | 8 | 66.9 |
| Hb, g/dL | 8.4 | 11.5 | 12.7 | 15 |
| PLT count, cells/mL | 245000 | 252000 | 63000 | 65000 |
| AST, U/L | - | - | - | 110 |
| ALT, U/L | - | - | - | 80 |
| Alb, g/dL | 4.3 | - | 2.7 | - |
| Qualitative CRP | ++ | + | + | + |
| ESR, mm/h | 26 | 38 | 26 | 11 |
| PCT, µg/L | 2.5 | - | - | 0.5 |
| BUN, mg/dL | 13 | 11 | - | 14 |
| Cr, mg/dL | 0.4 | 0.5 | - | 0.6 |
| LDH, U/L | 1080 | - | - | - |
Abbreviations: Alb, albumin; ALT, alanine aminotransferase; AST, aspartate aminotransferase; BUN, blood urea nitrogen; Cr, creatinine; CRP, C-reactive protein; ESR, erythrocyte sedimentation rate; Hb, hemoglobin; LDH, lactic acid dehydrogenase; PCT, procalcitonin; PLT, platelet; WBC, white blood cell.
2.2. Case 2
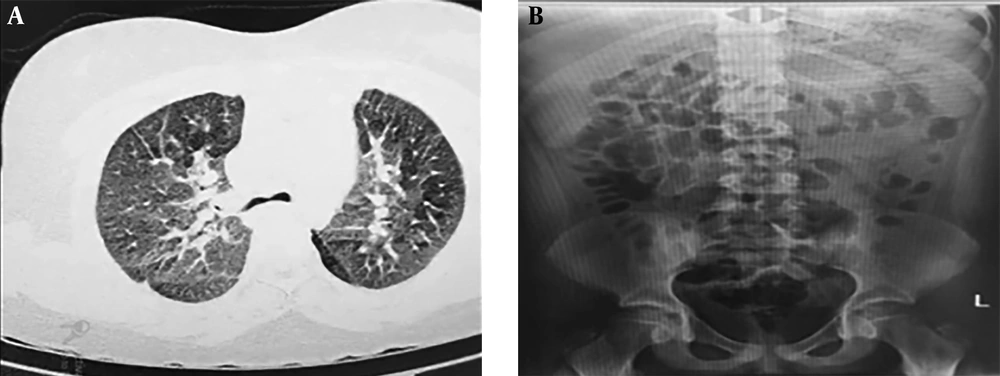
A 10-year-old boy was admitted to the pediatric COVID-19 center with loss of consciousness and its associated respiratory distress (Table 1). During physical examination, his oxygen saturation was 80%, measured by a pulse oximeter, the respiratory rate was 45 per minute, and subcostal and intercostal retraction was also observed (Table 2). Laboratory exams showed leukocytosis, lymphopenia, and elevated C-reactive protein (CRP) (Table 3). Due to his respiratory distress, intubation was needed. The chest CT scan was highly suggestive for COVID-19 (Figure 2). Besides, the result of the polymerase chain reaction (PCR) for SARS-CoV-2 RNA was positive. Thus, he was treated according to the Iranian pediatric protocol for treating COVID-19.
After the respiratory condition has stabilized, he was extubated and went on a Bi-PAP machine. Also, the symptoms gradually disappeared. He developed abdominal pain, guarding, and tenderness during the hospital stay. As the first step of a diagnostic approach, an abdominal X-ray was done, and no abnormal finding was observed (Figure 2). In the next step, the ultrasonography was performed, and the patient was diagnosed with appendicitis. Therefore, he went on an appendectomy. During the surgery, the patient’s Meckel’s diverticulum and peritoneal lymphadenopathy were identified and resected.
2.3. Case3
A five-year-old girl who suffered from fever, cough, myalgia, and abdominal pain was admitted to the pediatric COVID-19 center (Table 1). Her grandmothers were suspected for COVID-19, and she had a history of contact with them.
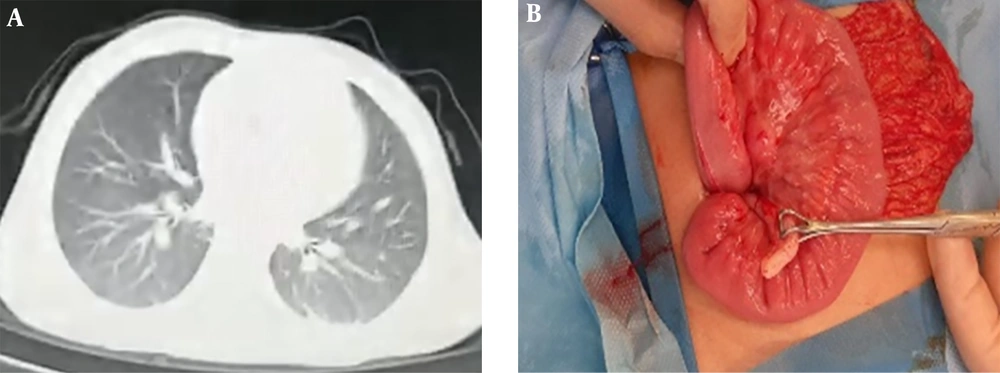
In physical examination, tachypnea, 40 per minute, subcostal retraction, and abdominal tenderness were detected (Table 2). Her laboratory examination revealed thrombocytopenia, lymphopenia, decreased serum albumin, and elevated CRP (Table 3). The chest CT scan showed typical lesions of COVID-19 (Figure 3). According to signs, symptoms, and suggestive chest CT scan, she was a probable case of COVID-19. Therefore, her therapy begun based on the Iranian pediatric protocol. Since she had vomiting, abdominal pain, tenderness, and guarding, an ultrasound was performed, and appendicitis was established as the probable diagnosis. Serous secretion around the appendix and several large lymph nodes were observed during the appendectomy (Figure 3).
2.4. Case4
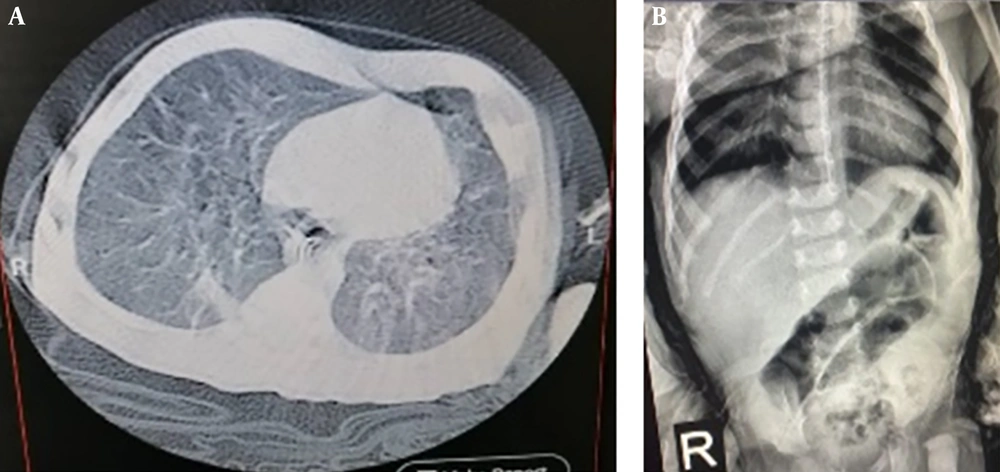
A 45 day-old-infant living in a nursery was admitted to the pediatric COVID-19 center with cough and respiratory distress (Table 1). He was a known case of cerebral palsy and a seizure disorder. In his physical examination, decreased arterial oxygen saturation, 75% in room air, nasal flaring, and suprasternal retraction were seen (Table 2). In laboratory study, thrombocytopenia, normal lymphocyte count, and elevated CRP was detected (Table 3). Diagnosis of COVID-19 was made after a positive result of the PCR test, and typical chest CT scan lesions (Figure 4). The patient received antiviral and antibacterial therapies, according to the Iranian pediatric protocol. On the third day of hospitalization, he developed oral intolerance, abdominal distention, and irritability. In his abdominal X-ray, a coffee-bean view was seen (Figure 4). Because of the severe illness and critical condition of the patient, the medical team decided to exclude surgery from therapeutic choices; the patient was treated by medical management. Gradually with the improvement of the patient’s respiratory condition, the gastrointestinal symptoms disappeared.
3. Discussion
When the WHO declared a global pandemic on 11 March 2020, the seriousness of the COVID-19 was revealed. Until 4 May 2020, there were 3,435,894 confirmed cases of COVID-19 and 239,604 deaths (1, 4).
According to recent studies, most of the COVID-19 patients are adults with predominant symptoms of cough, fever, fatigue, sputum production, shortness of breath, myalgia or arthralgia, sore throat, headache, nausea, vomiting, and diarrhea (5, 6).
Our literature review showed that respiratory-related symptoms are the most common symptom of COVID-19 among adults (6). In addition, COVID-19 patients may manifest other presentations, such as cardiac and gastrointestinal signs and symptoms. Based on a systematic review and meta-analysis study, only 12% of COVID-19 patients develop gastrointestinal symptoms (1). For instance, acute abdomen rarely occurs in adults infected with COVID-19 and even more uncommon in children (7-9).
On 11 February 2020, the Chinese Center for Disease Control and Prevention reported 44,672 confirmed cases of COVID-19, who only 416 (0.9%) of them were children aged 0 to 9 years and 549 (1.2%) were adolescents aged 10 to 19 years (10).
According to our literature review about abdominal signs in children with COVID-19, a case series by Cabrero-Hernandez et al. (8) reported five children infected with SARS-CoV-2 who were suspected of an acute abdomen. This article demonstrated that all patients had fever and abdominal pain, 60% presented with vomiting and diarrhea (simultaneously), and the rest were suffering only from vomiting (8). Another study conducted in May 2020 in the United Kingdom on the gastrointestinal presentations of COVID-19 has reported eight children presented at a single center in the UK with symptoms of atypical appendicitis. The most common gastrointestinal symptoms were abdominal pain, diarrhea, and vomiting (11). In the present study, out of four cases, only 2 (1 and 3) developed fever (Table 2). Also, cases 2 and 3 complained of abdominal pain, while cases 1 and 4, who could not complain about abdominal pain, showed oral intolerance, abdominal distension, and tenderness.
The next step of the diagnostic approach is abdominal imaging, i.e., ultrasonography or CT scan. Also, a study conducted in the UK recommended abdominal imaging when investigating for possible appendicitis in children with COVID-19, and all children in this study had imaging confirming terminal ileitis. Cabrero-Hernandez et al. (8) used imaging tools for participating patients, and the results showed inflammation of the intestine without surgically treatable disease. In this study, the abdominal X-ray of cases number one four revealed a coffee-bean view (Figures 1 and 4); ultrasonography was also performed for cases 2 and 3 and suggested appendicitis.
Still, there is no confirmed treatment for COVID-19 infection and its complications. In the study performed by Cabrero-Hernandez’s, the results of the CT scan didn’t suggest surgically treatable disease. Therefore, all cases received non-surgical treatment, including antibiotic therapy, lopinavir-ritonavir, tocilizumab, heparin, and hydroxychloroquine. All cases were discharged from PICU with a good overall health condition. Also, in the UK study, no surgical intervention was required, and all children were treated with non-surgical treatment. In our study, case 1 underwent laparotomy because of suspected volvulus. Also, appendectomy was done for cases 2 and 3 due to the results of ultrasonography. Diffuse peritoneal lymphadenopathies were detected for all three cases (Figures 1 and 3). Due to the critical condition of case 4, medical therapy was provided instead of surgery. All patients were also discharged with good condition.
3.1. Conclusions
According to our current knowledge, respiratory signs and symptoms are the most common presentations of the SARS-CoV-2. In this study, we reported four children presented with gastrointestinal symptoms that were later diagnosed with COVID-19. Therefore, pediatricians need to distinguish GI symptoms from COVID-19 manifestations.