1. Introduction
Coronavirus disease 2019 (COVID-19) was first reported in Wuhan, the capital of Hubei province, China, with the presentation of severe fatal respiratory illness in December 2019. Studies showed that the pathogenic agent is a novel coronavirus, named severe acute respiratory syndrome coronavirus-2 (SARS CoV-2). Soon, with dramatic worldwide spread, the World Health Organization (WHO) declared this condition a pandemic health emergency. To date, with more than 1.5 million affected people worldwide, a variety of respiratory and non-respiratory symptoms of this infection have been reported (1).
Fortunately, COVID-19 is less frequent and has a milder clinical course in children. However, the infection has been reported in all age groups even in the neonatal period. A few reports and guidelines have been published to date, demonstrating the epidemiologic and management protocols in children with COVID-19, of which almost none described the mortality rate among this group (2, 3).
In this article, we describe a series of nine pediatric patients admitted to our hospital with a diagnosis of COVID-19 as the cause of death. Although only two patients were tested positive for SARS-CoV-2 PCR and considered as definite cases, based on the importance of COVID-19 mortality, especially in children, the other patients were defined and presented as probable cases.
2. Case Presentation
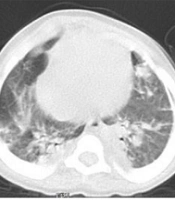
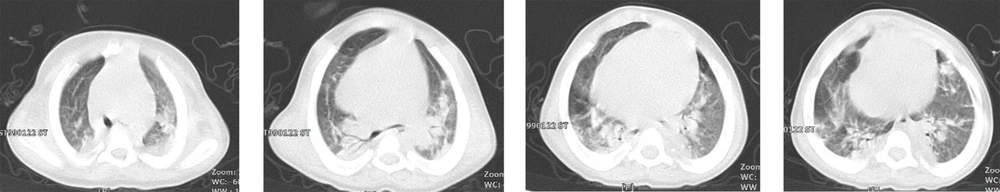
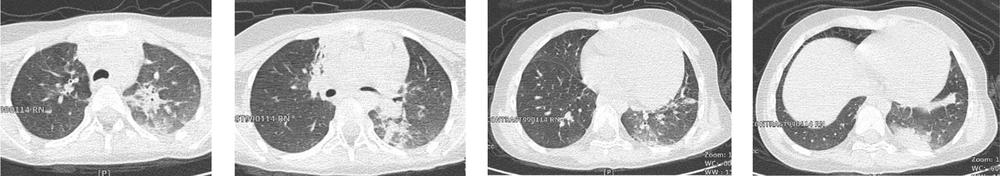
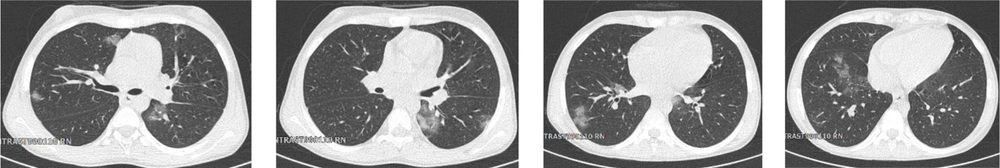
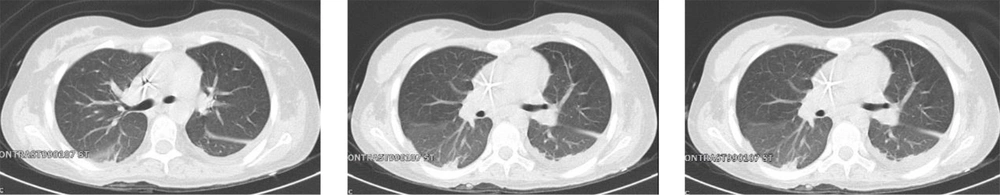
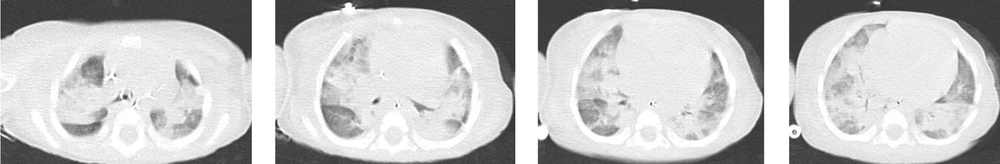
A total of 130 pediatric patients were admitted to Mofid children’s hospital from February to May 2020 suspected of or diagnosed with COVID-19 infection. Here, nine patients are reported with confirmed or suspected COVID-19 infection who died due to the complications of this disease. Patients’ clinical and paraclinical presentations are summarized in Table 1. Also, medical management and paraclinical findings are categorized in Table 2. Based on the national guideline for diagnosis and management of COVID-19, suspected cases are defined as patients with the presentation of dry cough, chills, or sore throat accompanied by dyspnea with or without fever. The probable cases are suspected patients with typical imaging findings in chest CT scans (ground-glass opacities, bilateral or unilateral peripheral chest infiltrations). Patients with positive PCR for SARS-CoV-2 were considered as confirmed cases (4). The chest CT scan cuts of five patients will be shown in Figures 1 to 5 later in the text. Despite the radiologic reports, other chest CT scan cuts were not available at the time of writing this article.
| Case No. | Age | Sex | Fever | Cough | Dyspnea/ Distress | Sore Throat | Vomiting | Diarrhea | Anorexia | Abdominal Pain | Confusion | Other | History of Contact | Underlying Disease |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 14 (mon) | F | - | + | + | - | - | + | - | + | - | - | Krabbe syndrome | |
| 2 | 2 (y) | F | - | - | + | - | - | - | - | - | - | - | MPS | |
| 3 | 9 (y) | M | - | - | - | - | - | - | + | + | - | + | CP/Seizure | |
| 4 | 13 (y) | M | - | + | - | - | - | + | + | - | + | - | + | Hepatic failure |
| 5 | 14 (y) | F | + | - | + | + | + | + | + | - | - | - | + | Gunshot wound |
| 6 | 7 (mon) | F | - | + | - | - | - | - | - | - | - | - | - | VSD/heart failure |
| 7 | 17 (mon) | M | + | - | - | - | + | - | - | - | - | Conjunctivitis/oral ulcers/ hands and feet edema | - | Kawasaki disease |
| 8 | 3.5 (y) | F | + | + | + | - | - | - | - | - | - | - | - | Aplastic anemia |
| 9 | 5 (y) | F | - | + | + | - | - | - | - | - | - | - | + | NDD |
Patients Characteristics, Signs, and Symptoms
| Case No. | WBC 103/µL | Lymphocyte (%) | ALC 103/µL | Platelets 103/µL | ESR | CRP | AST | ALT | Ph. | PO2 | PCo2 | HCO3 | SARS CoV-2 RT-PCR | Chest CT Findings | Medications |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 13.6 | 16 | 2.1 | 236 | 35 | 2+ | 66 | 24 | 7.25 | 70 | 49.9 | 21.6 | Negative | Multifocal, peripheral GGO/linear opacities in RUL, RLL, LLL | Chloroquine; Oseltamivir; Azithromycin; Meropenem; Ribavirin; Oseltamivir |
| 2 | 11.7 | 50.7 | 5.9 | 180 | 3 | Negative | 43 | 15 | 7.42 | 114 | 38.8 | 22.8 | Negative | Multifocal, diffuse GGO/linear opacities in RUL, RLL, LUL, LLL | Chloroquine; Ceftriaxone; Vancomycin; Azithromycin |
| 3 | 7.4 | 32 | 2.3 | 200 | 5 | 1+ | 48 | 40 | 7.14 | 104 | 25. 8 | 8.9 | Negative | Mixed multifocal peripheral GGO/consolidation and linear opacity in LUL, LLL, RUL; Halo sign | Chloroquine; Meropenem; Vancomycin |
| 4 | 3.4 | 19 | 6.4 | 78 | 7 | negative | 392 | 234 | 7.3 | 110 | 48 | 20.1 | Positive | Mixed multifocal, peripheral GGO, round/linear opacities in RUL, RLL, LLL, LUL; Reversed halo sign | Chloroquine; Metronidazole; Cefotaxim |
| 5 | 10 | 9.4 | 0.94 | 58 | 18 | 4+ | 26 | 63 | 7.29 | 89 | 40 | 19.5 | Positive | Diffused, GGO/Consolidation in RLL, LLL; Bilateral Pleural effusion; Pericardial effusion | Chloroquine; Oseltamivir; Amikacin; Linezolid; Piperacillin/Tazobactam |
| 6 | 11.7 | 27 | 3.1 | 402 | 4 | 3+ | 32 | 33 | 7.25 | 75 | 33.1 | 14.3 | Negative | Diffused mixed GGO/Consolidation in RUL, RLL, RML, LUL, LLL | Chloroquine; Azithromycin; Amikacin; Ampicillin/Sulbactam |
| 7 | 7.1 | 17.3 | 1.2 | 262 | 60 | 4+ | 83 | 55 | 7.46 | 115 | 22.1 | 15.6 | Negative | mixed GGO/Consolidation in RUL, RLL, LLL | Chloroquine; IVIG |
| 8 | 0.3 | - | - | 6 | 25 | 1+ | 28 | 40 | 7.42 | 118 | 39 | 22 | Negative | Mixed multifocal peripheral GGO/consolidation and linear opacity in LUL, LLL, RUL | Chloroquine; Azithromycin |
| 9 | 16.2 | 21.2 | 3.4 | 344 | 60 | 3+ | 30 | 54 | 7.35 | 105 | 35 | 19.9 | Negative | Multifocal peripheral GGO/Consolidations in RUL, RML, RLL, LUL, LLL; Tree in bud nodules | Chloroquine; Oseltamivir; Ceftriaxone; Vancomycin |
Paraclinical Findings and Medications of Nine Pediatric Cases With COVID-19 Infection
2.1. Cases 1, 2, and 3
Case 1 was a 14-month-old girl with Krabbe syndrome and a history of seizure and recurrent pneumonia. She was referred to our hospital with severe respiratory distress and cyanosis who had been intubated at a previous medical center due to cardiopulmonary arrest. She had a history of cough and increased respiratory rate a month before admission. Based on chest CT scan findings, she was diagnosed with COVID-19. Despite immediate initiation of both anti-viral and antibiotic therapies, she passed away with the clinical picture of ARDS and cardiogenic shock five days after admission.
Case 2 was a two-year-old girl, a known case of mucopolysaccharidosis, visiting our emergency ward with respiratory distress and knee swelling. The symptoms had emerged five days before visiting the hospital. Chest CT scan revealed multifocal, diffuse ground-glass opacities and consolidations in both lungs; thus, she was admitted to the COVID-19 ward. Even after hydroxychloroquine and intravenous antibiotic initiation, oxygenation worsened during her clinical course, necessitating invasive mechanical ventilation (IMV). She finally expired with cardiac arrhythmia and shock one week after admission.
Patient 3 was a nine-year-old boy with cerebral palsy and controlled seizures. He was first presented with loss of consciousness and respiratory distress that occurred on the day of referral. Cardiopulmonary resuscitation was performed before being referred to our hospital. At the time of admission, he was on mechanical ventilation. Parents stated a history of cough and myalgia in family members 10 days ago. Chest CT scan findings were compatible with the COVID-19 pattern. Soon after diagnosis, wide-spectrum antibiotics and hydroxychloroquine were initiated. Ultimately, six days later, the patient passed away secondary to cardiac arrest.
2.2. Cases 4, 5, and 6
Cases 4, 5, and 6 were all hospitalized in our center because of their underlying diseases. Case 4 was a 13-year-old boy with hepatic failure and a history of close contact with a suspicious person two weeks before symptoms onset. Case 5 was a 14-year-old girl with extensive shotgun wounds, and Case 6 was a seven-month-old girl admitted with a complicated ventricular septal defect (VSD). Case 5 was admitted and hospitalized in our center for eight months. They had all experienced cough. The first two cases also had gastrointestinal symptoms, and the PCR tested positive for COVID-19. Except for patient 6 with congenital heart disease, echocardiography showed no abnormality. Case 4 died with the picture of LOC and encephalopathy one month after diagnosis. Cases 5 and 6 passed away two weeks after symptoms initiation, and the results of DIC and cardiac arrhythmia with wide QRS complex and bradycardia led to asystole, respectively.
2.3. Cases 7, 8, and 9
Case 7 was a 17-month-old boy with complaints of fever, non-purulent conjunctivitis, nausea, and vomiting four days before admission. Chest CT scan showed peripheral ground-glass opacities in the upper and lower lobes of both lungs. Also, he fulfilled atypical Kawasaki disease criteria and underwent IVIG transfusion. Fever disappeared after IVIG administration. Echocardiography revealed coronary artery involvement. He was discharged from the hospital after recovery one week later. However, two days after discharge, he was expired with the presentation of respiratory distress, cyanosis, and cardiac arrest at home despite resuscitation operations delivered by emergency service.
Two other patients presented with respiratory distress and cough. Case 8 suffered from aplastic anemia, and the last patient was a five-year-old girl with severe neurodevelopmental delay and swallowing problems, living in a nursing center. The caregiver of the last patients stated a history of upper respiratory infection symptoms in some other children in their centers. Case 8 died one week after hospitalization with the presentation of respiratory distress and cardiac arrest. Eleven days after the beginning of the symptoms and four days after hospitalization, despite antiviral initiation from the first day, Case 9 passed away with respiratory failure and irreversible shock.
3. Discussion
By November 8, the COVID-19 pandemic caused > 49,000,000 infections and > 1,000,000 deaths globally. Children in all age groups seem to be susceptible to this infection although mortality rates were less than 1% in previous reports (5-7).
In this article, we presented nine children with probable or confirmed COVID-19 infection, admitted to our pediatric tertiary center. Their age ranged between seven months and 14 years. All had underlying diseases and three of them were hospitalized at the time of diagnosis due to their previous conditions. Only two of these patients had positive RT-PCR for COVID-19 from nasopharyngeal sampling. However, due to some limitations, we only had one PCR sample for each patient, for whom radiologic findings could not be explained with conditions other than COVID-19. This finding is compatible with a previous report in our country and could be explained by sampling errors or inadequate test sensitivity (8). Cough (55.5%) and fever (33%) were the most common findings in their history. Chest CT scans of our patients showed mostly ground-glass opacities with both mixed or separated consolidations. Both lungs were involved in all cases. Halo sign and reversed halo sign were seen in the patient with positive RT-PCR for SARS-CoV-19. Lymphopenia was observed in 45.5% of the patients. Also, Thrombocytopenia and elevated CRP were detected in 33.3% and 77.7% of the cases, respectively. Most of the cases (66%) eventually warranted invasive mechanical ventilation for breathing support and oxygenation.
Case 7, a 17-month-old male with atypical Kawasaki disease presentations, died with symptoms of cardiac involvement. In this case, echocardiography during hospitalization showed no abnormalities, and he became symptom-free after IVIG infusion. He was being managed with hydroxychloroquine for COVID-19. It seems that late-onset cardiac involvement of COVID-19 or arrhythmogenic effects of hydroxychloroquine in this vulnerable patient may have been the cause of death.
Patient No. 2 was a two-year-old child with MPS. Patients with this lysosomal storage disease are more susceptible to chronic lung infections due to their chest deformity and subsequent defective ventilation. This condition would lead to more serious SARS-CoV-2 infection and less compliance to COVID-19 complications. Also, due to the deformities of the oropharyngeal and laryngeal area, ventilation supportive care was more difficult and demanded critical consideration.
Most pediatric cases with COVID-19 to date have been reported from China, the United States, and Italy. Fortunately, these groups account for less proportion of infected population and mortality. Fever, cough, malaise, and gastrointestinal manifestations were the main clinical features of COVID-19 in children. In the report of the United States, one-third of the pediatric cases were aged 15 - 17 years. Also, in this study, children less than one-year-old age had the highest rate of hospitalization. Imaging findings have not been described specifically in children, although bilateral or unilateral involvement, including ground-glass opacities or patchy infiltrations were previously reported in some articles. Studies in China, the United States, and Italy showed that the mortality rate increases with age substantially. Due to fewer reported cases in patients under the age of 20, the exact etiology for these findings needs to be clarified (9-15).
The low rate of positive SARS CoV-2 RT-PCR in this report may be explained by the low sensitivity of this test. Due to false-negative results of RT-PCR in the diagnosis of COVID-19, several studies suggested chest CT scan for the early detection of the disease. It seems that typical clinical presentations with characteristic imaging findings could confirm the diagnosis despite a negative RT-PCR test (16-19).
This study has some limitations, as mentioned before. The lack of test availability and accuracy at the time of diagnosis is the most important limitation of this study. Also, other confirmation tests such as antibody level measurement were not available at that time. Today, with better diagnostic facilities, more confirmed patients will be detected.
At last, it should be considered that although the mortality rate of COVID-19 is lower in children, it could lead to serious conditions in patients with underlying diseases. Also, hospital staff or caregivers could be potential infection carriers for hospitalized patients in medical centers. In conclusion, we recommend that children and adolescents with underlying diseases who are suspected or confirmed cases of COVID-19 should be hospitalized and vigorously treated. Also, since medical management is not specific yet, tight monitoring of vital signs and multi-organ functions must be considered according to their underlying conditions during the treatment process.