1. Background
Acute appendicitis (AA) is the most frequent cause of emergency conditions of the abdominal cavity. However, unfortunately, appendicitis is still an intricate illness entity (1). Regarding the lack of widespread investigations in this entity, there are several vague points for clinicians worldwide (2). Diagnostic errors for appendicitis are relatively common in childhood, thereby resulting in a delay for surgery or negative appendectomies.
Acute appendicitis is uncommon in children younger than 3 years, but the rate of perforation is much higher in young children.
Regarding the importance of AA diagnosis in children and the presence of numerous misdiagnoses for this condition, there are some scoring systems for early identification of acute abdomen in the literature. We used the Alvarado scoring system (3) to evaluate the value of this diagnostic way in improving preoperative diagnosis of AA. Alvarado scoring system identifies pediatric patients with suspected appendicitis. Parameters for evaluation of appendicitis in the Alvarado score include migration of pain, anorexia, nausea or vomiting, right lower abdominal quadrant tenderness, rebound tenderness in the right lower quadrant, increase of temperature, leukocytosis, shift to the left of neutrophils.
2. Objectives
We aimed to investigate retrospectively the diagnostic effectiveness of the preoperative tests based on histopathologic consequences.
3. Methods
In this cross-sectional study performed from October 2016 to October 2017, ten provinces out of 31 provinces in Iran were randomly selected. A total of 631 patients referring to the specified hospitals with the suspicion of acute appendicitis were assessed. The data were gathered and entered into the checklist by reviewing the hospital recorded files.
3.1. Selection of Patients for Study and Data Collection
This study was designed for Children between 3 to 18 years of age, with acute abdominal pain suspected of appendicitis that at first were visited by a pediatrician in the pediatric emergency medical center and then required surgical consultation for possible appendicitis before request radiologic investigations. Cases with a history of previous abdominal surgery who had chronic medical conditions, or underwent multiple radiologic investigations of the abdomen within the previous last week were excluded. About 20 cases were excluded. A total of 631 patients who were referred to the specified hospitals with the suspicion of acute appendicitis and had surgical consultation for probable appendicitis were assessed. The data were gathered and entered into the checklist by reviewing the hospital recorded files.
The patient’s medical records were investigated for symptoms and signs and physical examination recorded by a pediatrician and all data registered based on a non-surgeon examiner who consulted with a surgeon. Laboratory, pathology, and operative reports were noted frankly from the electronic laboratory information. Operative information was evaluated for the occurrence or lack of appendicle perforation. Reports of pathology were analyzed whether there was appendicitis. Appendix pathology reports such as “early appendicitis”, “appendicitis”, “gangrenous”, “perforated appendix”, all of which were considered appendicitis. Another impression registered was the absence of appendicitis. Cases with missing data were excluded. The manuscript was accepted by the Institutional Board Review and the Medical Ethics Committee of Shahid Beheshti University of Medical Sciences.
3.2. Methods of Outcome Measurement
The final diagnosis was confirmed either by pathologic details if the patient underwent an operation in the same center or by follow-up telephone calls if the patient did not have an operation history. Telephone call revealed further diagnostic evaluation or operative management in another center for two weeks after the initial visit to the primary center. Data used for the assessment of Alvarado’s scoring system (3) are summarized in Table 1. Alvarado scoring system was used to include cases for the assessment of the accuracy of this test for diagnosing appendicitis in our centers.
| Characteristic | Point Assessment | Suggested Management |
|---|---|---|
| 1. Migration of pain | 1 | |
| 2. Anorexia | 1 | |
| 3. Nausea/vomiting | 1 | |
| 4. RLQ tenderness | 1 | |
| 5. Rebound pain | 2 | |
| 6. Fever (> 37.3) | 1 | |
| 7. Leukocytosis (L) (10,000/-µL) | 2 | |
| 8. Left shift: neutrophil > 75% | 1 | |
| Points of Alvarado Scoring system | ||
| 5 - 6 likelihood of appendicitis | Observe | |
| Sum of 7 and more suggests appendicitis | Surgery |
Alvarado Scoring System for Pediatric Appendicitis (3)
3.3. Data Analysis
Data were analyzed with SPSS version 17. Patients with missing data (for any component of the Alvarado scoring system) were removed. The computed scores were employed to evaluate the Alvarado score greater than or equal to seven for establishing risk for appendicitis. In addition, receiver operator characteristic curves (ROC) were used for all scores to graphically characterize ROC curves and evaluation of the diagnostic value of the documented parameters in acute appendicitis.
Data were measured with student t-test and chi-square test for acute appendicitis and non-appendicitis groups. Quantitative data were described as mean and standard deviation (SD), which were compared with t-test. Qualitative data were compared with the chi-square test with frequency and percentage of description. A P-value of less than 0.05 was considered statistically significant.
4. Results
4.1. Demographic Characteristics of the Patients
The mean age of eligible patients was 9.3 ± 3.21 years ranged from three to 18 years, of which 380 (60.5%) were male. During the period of October 2014 and October 2015, 631 patients had a surgical consultation for probable appendicitis among patients with abdominal pain. Of all 631 patients who were suspected of appendicitis, definitive diagnosis was confirmed in 168 with the prevalence rate of 27% that perforated appendicitis was found in 22 patients, infectious appendicitis in 14 patients, and gangrenous appendicitis in 11 patients. The mean age of patients without appendicitis was 108 ± 38.81months, and the mean age of patients with acute appendicitis (AA) was 111 ± 39.92 months.
4.2. Patients’ Symptoms and Signs
Migratory pain was present in 41% of patients without appendicitis and in 53.2% of patients with AA (P-value = 0.040). In this study, there were no significant differences for migratory pain between the two groups. Nausea or vomiting was noticed in 70% of patients without appendicitis and 75% of patients with AA (P-value = 0.392). In this study, there were no significant differences in nausea or vomiting between the two groups. Anorexia existed in 62% of patients without appendicitis and was present in 70% of children with AA (P-value = 0.069). In this study, there were no significant differences for anorexia between the two groups.
4.3. Patient’s Physical Examination
Tenderness in the right iliac fossa was found in 42% of the patients without appendicitis and was found in 67% of the patients with AA (P-value = 0.000). In this study, there were no significant differences for tenderness in RLQ between the two groups. Rebound tenderness in the right iliac fossa was found in 42% of patients without appendicitis, and it was found in 68% of the patients with AA (P-value = 0.000). In this study, there were no significant differences for Rebound tenderness between the two groups. An increase in auxiliary temperature > 37.3°C was noticed in 2.35% of the patients without appendicitis and was present in 3.5% of the children with AA (P-value = 0.386). In this study, there were no significant differences for fever between the two groups.
4.4. Laboratory Findings
Leukocytosis > WBC = 10,000/L was noticed in 71% of patients without appendicitis and was present in 72.8% of children with AA (P-value = 0.629). In this study, there were no significant differences for leukocytosis between the two groups. Left shift with neutrophil > 75% was presented in 60.2% of the patients without appendicitis and was present in 50% of the children with AA (P-value = 0.016). Moreover, there were no significant differences for shift to the left between the two groups. Clinical characteristics of the cases with and without appendicitis are summarized in Table 2.
| Feature (Total = 631) | No Appendicitis, N = 463 (73) | Appendicitis, N = 168 (27) | P-Value |
|---|---|---|---|
| Mean age, mo | 108 ± 38.81 | 111 ± 39.92 | 0.000 |
| Migration of pain, % | 41 | 53.2 | 0.040 |
| Anorexia, % | 62 | 70 | 0.069 |
| Nausea/vomiting, % | 70 | 75 | 0.392 |
| RLQ tenderness, % | 42 | 67 | 0.000 |
| Rebound pain, % | 46 | 66.5 | 0.000 |
| Increase in temperature > 37.3°C, % | 2.3 | 3.5 | 0.386 |
| Leukocytosis > WBC = 10,000/µL, % | 71 | 72.8 | 0.629 |
| Shift to the left, % | 60.2 | 50 | 0.016 |
Clinical Characteristics of the Patients with Suspected Appendicitis
4.5. Alvarado Scores
Alvarado scores for Appendicitis group: anorexia (70% of patients), nausea/vomiting (75%), RLQ tenderness (67.3%), differential WBC count (50%), migration of pain (53.2%), rebound pain (66.5%), presence of fever (3.5%), and increase in leukocyte count (72.8%). When the Alvarado system was used, regarding the cut-off point of 7 to decide for operation, the positive predictive value (PPV) was 32.6% and negative predictive value (NPV) was 76.73%, with sensitivity of 44.05% and, specificity of 66.95%. See Table 3 for sensitivity, specificity, NPV, PPV, accuracy, and the ratio for clinical Alvarado scoring systems.
| Alvarado | All Patients (N = 661) |
|---|---|
| Sensitivity, % | 44.05 |
| Specificity, % | 66.95 |
| Accuracy, % | 60.86 |
| Negative predictive value (NPV), % | 76.73 |
| Positive predictive value (PPV), % | 32.60 |
Presentation of the Alvarado Scores More Than or Equal to 7
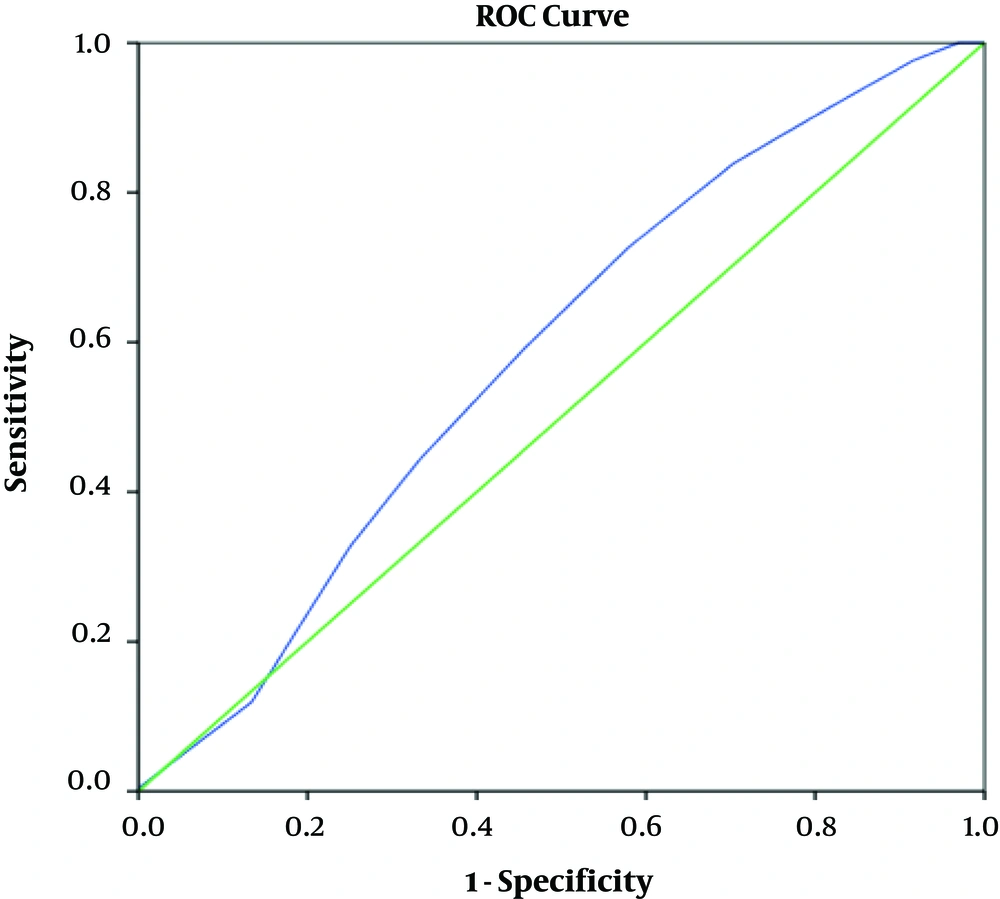
In this study, there were no significant differences between the values of the Alvarado score and the occurrence of AA. Also, ROC curves were created for Alvarado scores to symbolize the whole score presentation (Figure 1). The area under the curve was 0.58 (0.54 to 0.63) for Alvarado. The area under the curve is very low; so there is no value for diagnosis of appendicitis.
All probable cut-off points, with their related sensitivity and false-positive rate, are shown in Table 4. Scores of 7 (Alvarado) have been determined in studies to discriminate cut-off points for diagnosing appendicitis. In the present study, the cut-off point of 4.5 was considered for children with a sensitivity of 73% and specificity of 58%.
| Positive if Greater Than or Equal To | Sensitivity | 1-Specificity |
|---|---|---|
| -1.00 | 1.000 | 1.000 |
| 0.50 | 1.000 | 0.970 |
| 1.50 | 0.976 | 0.916 |
| 2.50 | 0.929 | 0.840 |
| 3.50 | 0.839 | 0.704 |
| 4.50 | 0.726 | 0.579 |
| 5.50 | 0.583 | 0.449 |
| 6.50 | 0.440 | 0.330 |
| 7.50 | 0.327 | 0.251 |
| 8.50 | 0.119 | 0.134 |
| 9.50 | 0.006 | 0.002 |
| 11.00 | 0.000 | 0.000 |
Demonstrates Cut-off Points for All Probable Scores
Other diagnosis have been included: Mesenteries lymphadenitis, Meckel’s diverticulitis, abscess of the ovary, torsion of ovarian cyst, ruptured ovarian cyst, and two cases without any recognized anomaly.
5. Discussion
Appendicitis is a prevalent disorder with a chance of occurrence about 7 percent for everybody in all lifetime (4) the most important symptoms are pain in the right lower quadrant, anorexia, and vomiting. The reliable physical exams are tenderness, rebound tenderness, and guarding in the iliac fossa. Practical investigations for suspicious appendicitis include complete blood count and urinalysis. Although the main diagnostic way remains physical examination, the use of imaging studies is growing more than before because of frequent misdiagnosis, especially in young patients (5). Recent studies showed that inflammatory markers, including white blood cell (WBC), C-reactive protein (CRP), or pro-calcitonin are valuable to recognize appendicitis with significant sensitivity and specificity (6, 7).
Unfortunately, the vague signs and symptoms in young children lead to increasing the risk of appendicle perforation and related morbidity and mortality (8). Perforation of appendix reported 20% to 90% in various studies (9). The rate of negative appendectomy reported about 20%. So, to diagnose appendicitis, especially in the pediatric group, imaging can be a critical tool for decreasing misdiagnosis (9, 10). Ultrasonography has been verified as an early diagnostic tool in young patients to avoid radiation exposure and risk of cancer secondary to CT (11, 12). Routinely, CT scan results in extensive cost too.
Scoring systems are simple and can be used independently of particular tools, and they do not require novel abilities (7). On the other hand, these scorings are not employed regularly, so the results are not clear, especially in children. In different scoring systems for judgment of AA, the Alvarado is shown to be more successful. A score of more than seven points is reported with a sensitivity of about 88% to 90%, but the specificity is usually under 80% and is particularly low in young patients and women (7). Alvarado at first manuscript (3) retrospectively studied 305 cases with acute abdominal pain indicative of appendicitis. The tests showed sensitivity of 81%, specificity of 74%, PPV of 92%, and NPV of 46%. In the present study, 631 patients, aged 3 to 18 years, with suspected appendicitis were assessed. Twenty-seven percent of cases had appendicitis. Moreover, PPV was 32.6%, and NPV was 76.73%, with a sensitivity of 44.05% and specificity of 66.95%.
Ohle et al. (13) performed a review article and evaluated the diagnostic accuracy of the Alvarado score. The investigation was designed with paying attention to three sub-groups: women, men, and children. They suggested the cut-off point of five is suitable for ‘ruling out’ appendicitis (sensitivity 99% overall, 96% in men cases, 99% for woman cases, and 99% in children). The cut-off point of seven, as suggested by Alvarado for the need to attempt surgery, had poor results for each subgroup (with specificity overall about 81%, for men 57%, women cases 73%, and children cases 76%). Similarly, in the present study, 4.5 is suggested as the cut-off point for children with a sensitivity of 73% and specificity of 58%.
So it is better that a cut-off point score is used for predicting the likelihood of appendicitis in high-risk groups such as children lower than seven. As studies showed a high chance of perforation followed appendicitis in children, so we suggest that the Alvarado score is used at the cut-off point of 4.5 to 5 to establish a rule-out point for appendicitis in children for preventing from misdiagnosis and catastrophic morbidity and mortality in children. However, we recommend the use of other investigation tools for proper diagnosis to prevent negative operation in young children.
Singla et al. (14) designed a cohort study on the Asian population for two years. They studied 50 adult cases with Right lower quadrant pain and used a modified Alvarado score (modified Alvarado score excludes shift to the left for neutrophil maturation more than 75%). Also, PPV was reported 100 %, and the rate of negative appendectomy was 0% (no false-positive patients, while 21 false-negative patients). In contrast, Khan and ur Rehman study (15) demonstrated a PPV of 83.3% with 15.6% negative appendectomy.
Goyal et al. (16) designed a study on patients supposed to acute appendicitis through one year by, Modified Alvarado score (as told above). The study explained making use of the Modified Alvarado Score in cases with suspicion of appendicitis with an acceptable amount of sensitivity and specificity. They advised Modified Alvarado scores in men and children; however, supplementary employing of ultrasonography or diagnostic laparoscopy in women is suggested to diminish the incorrect rate of false-positive in them. However, in our study, shift to the left with neutrophil > 75% was presented in 60.2% of the patients without appendicitis and was present in 50% of the children with AA (P-value = 0.016). We have a statistically significant difference in the occurrence of shift to the left in the patients with AA compared with the cases without AA. Therefore, we do not recommend a modified Alvarado Score in children.
Toprak et al. (17) assessed the combination of Alvarado score with ultrasonography results in children suspected of appendicitis. They achieved 92% specificity, 93% sensitivity, and 92% accuracy for the US in diagnosis of appendicitis; but confirmed a few obstacles and limits for the US that led to false-positive or -negative consequences. So they employed Alvarado score integration with the US according to recognize the chance of appendicitis in children. They achieved a cut-off of 6 for Alvarado score as a good predictor of appendicitis in children. All patients with an Alvarado score ≥ of 7 had a diagnosis of acute appendicitis. The present study proposes that if the Alvarado score is more than 6 scores and US does not show any compressible appendix, surgery is suitable management without the need for additional imaging techniques, particularly CT. They recommended that in the patients with an absence of none compressible appendix with a low Alvarado score, appendicitis can be securely ruled out. Further, CT is suggested to be helpful in children with moderate scores and vague US results (18-20). The negative appendectomy and complicated appendicitis rates are both vital for superiority measures of the management of appendicitis, especially in children (21, 22). On the other hand, these two items have an opposite correlation. In our study, as the cut-off point of 7 for the Alvarado score is not suitable for suggestion of appendicitis, appropriate diagnosis needs other investigations accompanied with Alvarado score.
5.1. Conclusions
In summary, although impression to clinical Alvarado score system can be an influential guideline in decision for cases with acute abdomen suspected of appendicitis in adults, judgment on examination of abdomen is complex in children, especially in young children. Furthermore, although these scores are attractive in conception, pediatric clinicians- in the fashion of deciding on the diagnosis of the disease in children- should observe the precautionary measures and examine them very comprehensively. Furthermore, although the Alvarado system scoring supplies obviously helpful diagnostic information in adult patients but in children supposed to appendicitis, this method lonely affords not sufficient positive predictive value (PPV) for determining the necessitate of operation .so It is healthier that cut off point score for expecting the possibility of appendicitis in children judge lower than 7.