1. Introduction
Since the emergence of the novel coronavirus disease 2019 (COVID-19) pandemic, several associated neurological manifestations have been reported in the related literature. Regarding a cohort study conducted on severely ill admitted COVID-19 patients, neurological complications have been documented in 45.5% of infected patients 1 - 14 days after the onset of infection (1, 2). Reportedly, neurological manifestations of COVID-19, which are assumed to be caused by exaggerated immune-mediated response, are a frequent complication to be expected following infection. It seems about 36% of pediatric patients with COVID-19 have neurological involvement attributable to either peripheral or central nervous systems. Sixth nerve palsy in viral infections may be due to either direct invasion or indirect immune mechanisms (3). One of the uncommon features of COVID-19 infection is IIH (4-7).
Pseudotumor cerebri is a clinical condition which presents with headache, papilledema, increased blood pressure, and normal cerebrospinal fluid analysis. There are some causes that have been attributed to these signs and symptoms, such as venous sinus thrombosis, toxicity of some medications such as tetracyclines, vitamin A, contraceptives, and sepsis (8, 9). Furthermore, sixth nerve palsy has been related to some viral infections in children, including enterovirus and Epstein-Barr, as well as vaccinations. Although sixth nerve palsy is not well studied in children, its incidence is low among them. Some important causes of abducens nerve palsy include multiple sclerosis (MS), vasculopathies, tumors, and inflammatory conditions such as viral infections. However, if accompanied by papilledema, it strongly suggests increased intracranial pressure (ICP) associated with IIH among COVID-19 patients (3).
Herein, we describe a 10-year-old girl with confirmed COVID-19 infection by reverse transcription polymerase chain reaction (RT-PCR) presented with headache, diplopia, severe bilateral papilledema, and sixth nerve palsy due to IIH.
2. Case Presentation
A 10-year-old female referred to pediatric neurology clinic with headache and diplopia since three days ago. The patient had a history of fever, chills, myalgia, and respiratory symptoms about two weeks ago, which had recovered after a week. Her parents also had a history of COVID-19 infection about two weeks ago that was confirmed by nasopharyngeal RT-PCR. The patient had no remarkable history of medical problems, including endocrinopathy, hematologic disorder, obesity (BMI = 21), and use of any medications.
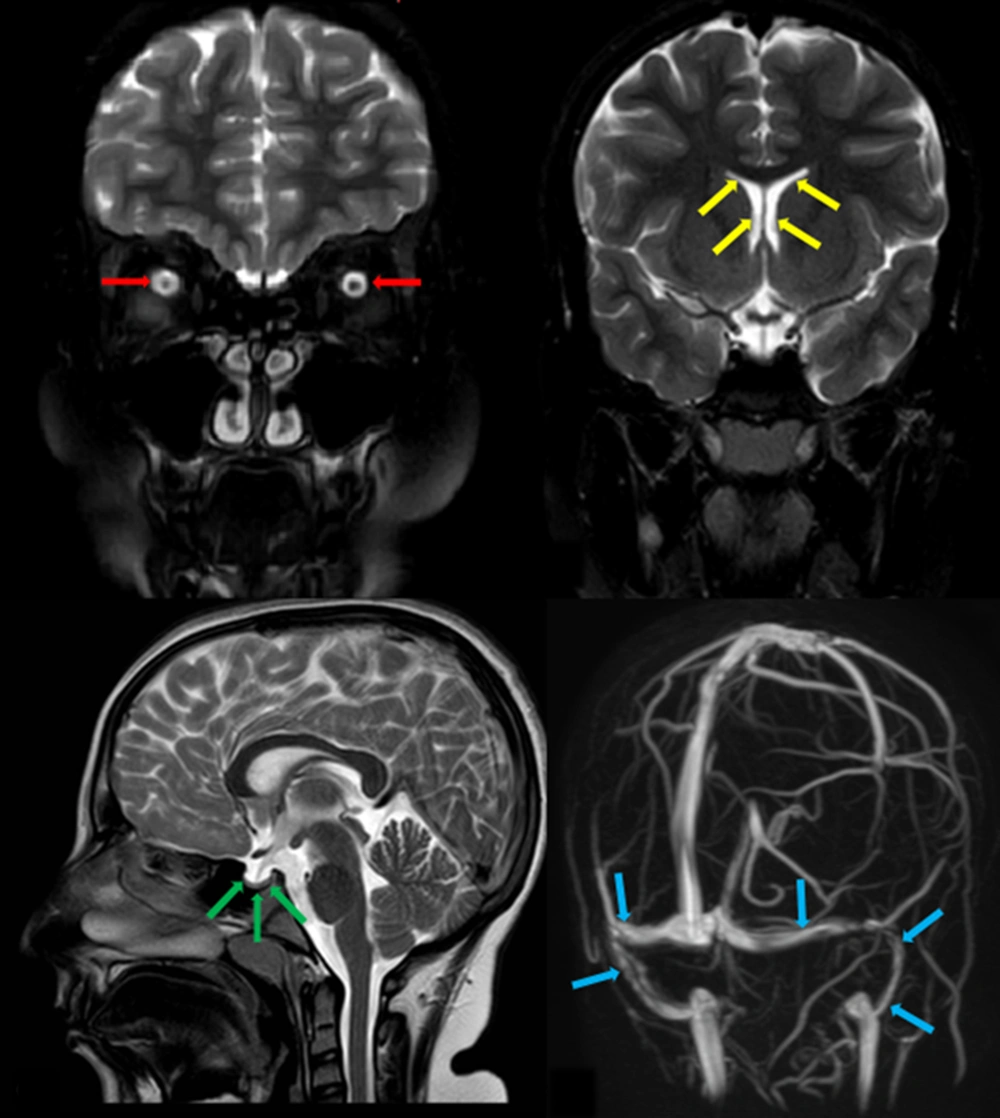
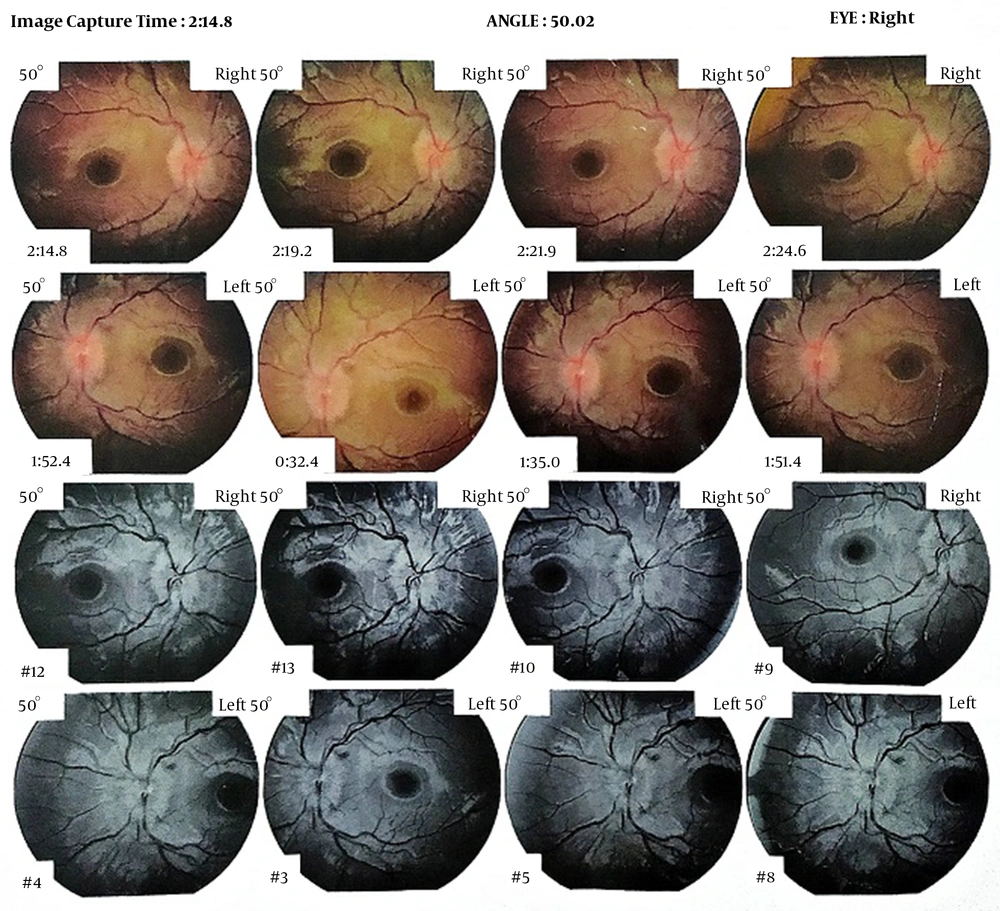
On physical examination, the patient was completely conscious and well-developed. An ophthalmologic exam revealed severe bilateral papilledema, and in neurological examination, she had bilateral sixth nerve palsy. Motor, sensory, and cerebellar examinations were normal. Brain magnetic resonance imaging (MRI) showed no evidence of space occupying lesion or hydrocephalus, but there was evidence of bilateral optic nerve sheath hydrops, slit-like lateral ventricles, and pituitary gland compression against pituitary. Although brain MR venography showed no evidence of sinus venous thrombosis, narrowed transverse/sigmoid sinuses were indicated (Figure 1). Blood test results were included: WBC = 6500/mm3 (PMN = 45%, lymph = 55%), Hb = 13.5 g/dL, PLT = 260000/mm3 , ESR = 36, CRP = 45 mg/L, Na = 141 mmol/L, K = 4.2 mmol/L , Ca = 9.5 mg/dL , P = 4 mg/dL, ALT = 35 IU/L, AST = 40 IU/L, ALP = 350 IU/L, BS = 85 mg/dL, BUN = 13 mg/dL, Cr = 0.5 mg/dL, T4 = 10.5 µg/dl (5 - 14.5), TSH = 3.5 mIU/L (0.35 - 5.1), PTH = 32 Pg/mL (10 - 65). Lumbar puncture was performed; the cerebrospinal fluid (CSF) analysis was normal, and CSF opening pressure was 56 cmH2O. Retinography indicated bilateral optic disc swelling, paleness, and blurred borders. Optic nerve head ocular coherence tomography (OCT) revealed papilledema and decrease in nerve fiber layer thickness in both eyes (Figure 2). Considering the history of a febrile illness in our patient and positive history of COVID-19 infection in her parents, RT-PCR for COVID-19 was obtained by nasopharyngeal swab, which was positive. CSF RT-PCR was negative for COVID-19. We ruled out other differential diagnoses of IIH by laboratory tests, ophthalmologic evaluations, and neuroimaging modalities. Due to the positive history of COVID-19 infection in parents and positive COVID-19 RT-PCR in our patient, we did not perform other virology tests.
A and B, Coronal fat suppressed SE T2WI. Red arrows in A indicate optic nerve sheath hydrops and yellow arrows in B show slit-like lateral ventricles; C, Midsagittal SE T2WI. Partial empty sella, as pituitary gland compressed against pituitary fossa, is noted (green arrows); D, 3D phase contrast MRV. Blue arrows delineate narrowed transverse and sigmoid sinuses bilaterally.
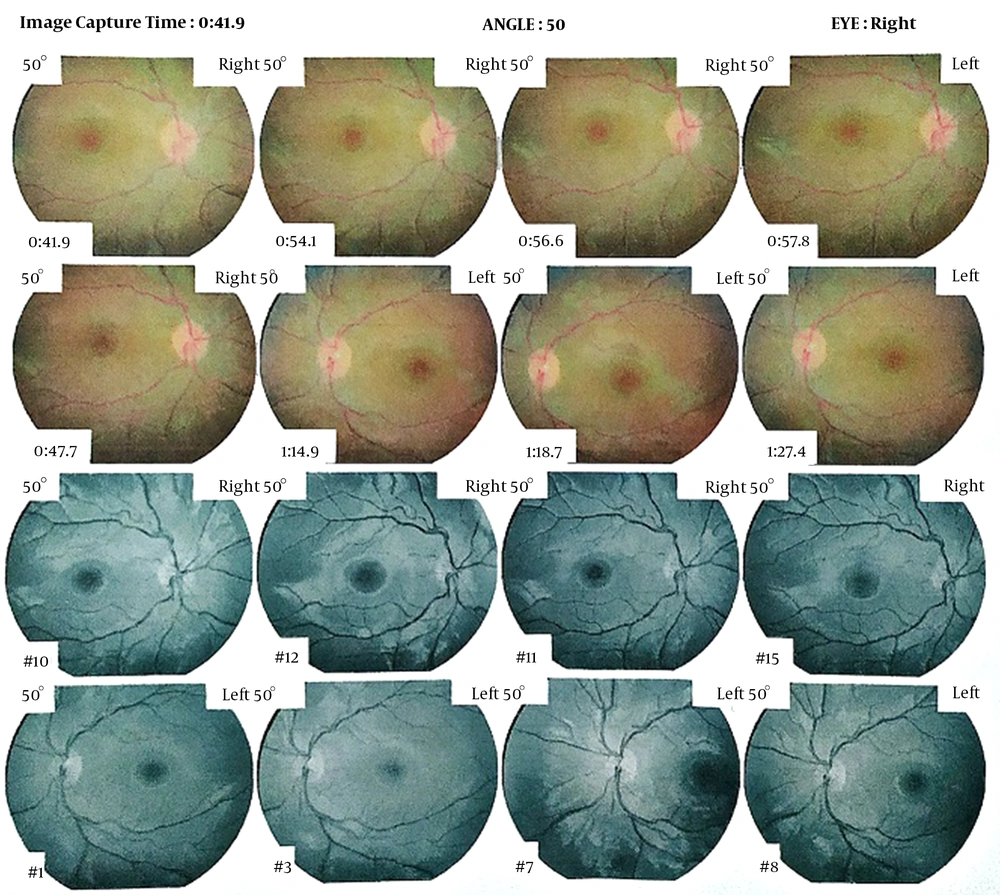
Based on the findings on physical examination and paraclinical evaluations (OCT, retinography, brain MRI, and lumbar puncture), the most probable diagnosis was IIH. The patient was admitted for three days. Medical treatment with oral acetazolamide 1000 mg daily was started. After three weeks of medical treatment, in clinical exam, we found that sixth nerve palsy was remarkably subsided, and ophthalmoscopy showed a significant remission of papilledema (Figure 3). Acetazolamide was continued about eight weeks, and the patient had no problem during this period.
3. Discussion
We reported a 10-year-old girl with symptoms and sings of IIH associated with a history of COVID-19 infection for about two weeks. COVID-19 infection is not just a respiratory system infection, and it can result in some extrapulmonary involvement. They can result from several mechanisms: first, in COVID-19 infection, a “cytokine storm” may develop, and pro-inflammatory cytokines are abundant in circulatory system. These cytokines can result in systemic inflammatory response and tissue injuries subsequently (10). Second, COVID-19 can result in hypercoagulable state, either by direct attachment to endothelial cells via angiotensin converting enzyme-2 (ACE-2) receptor and subsequent endothelial damage or as a result of systemic inflammatory response and activation of coagulation system. Endothelial dysfunction and hypercoagulable state change blood supply of various organs by causing vasoconstriction and thrombosis, which eventuate ischemia and tissue damage (11). Third, COVID-19 can directly attack cells causing cell injury and ultimate organ dysfunction (4).
One of the systems affected by COVID-19 is nervous system (either peripheral or central). As aforementioned, some mechanisms contribute to systemic organ dysfunction in COVID-19 infection. Neurological complication is caused by various mechanisms including neurotropic or neuroinvasive effect of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), systemic inflammatory response, thrombotic events, and also post-infectious autoimmune effect of COVID-19 (12, 13). According to these mechanisms, different neurological manifestations can occur, including ageusia, anosmia, encephalopathy, vascular events, and Guillain-Barre syndrome (14, 15).
IIH is a condition presented with headache, bilateral papilledema, bilateral sixth nerve palsy, normal CSF profile, and a normal neuroimaging (except non-specific findings such as prominent subarachnoid space around optic nerve, vertical tortuosity of optic nerve, and superior compression of hypophysis) (8, 9). Other etiologies of pseudotumor cerebri include sepsis, long-term corticosteroid consumption or corticosteroid withdrawal, use of contraceptives, tetracyclines, hypervitaminosis A, etc. (8, 16). The pathogenesis of IIH is not definitely known yet. The probable mechanisms include venous outflow abnormalities, raised intracranial venous pressure, altered production and absorption of CSF, low-grade inflammation, intracranial vascular clotting, and cerebral edema (17).
Mechanisms of IIH in COVID-19 infection are somehow similar to those contributing to COVID-19 neurological complications that include low-grade inflammation accompanied by hyperviscosity and hypercoagulable state (18). The patients who meet the criteria of IIH with CSF pleocytosis most likely have secondary increased ICP due to infectious agents rather than true IIH, including bacterial, fungal, tuberculous meningitis (TBM), viral encephalitis or meningitis, and Lyme disease (19). According to normal CSF profile in our case, the most probable cause of sixth nerve palsy is increased intracranial pressure due to IIH.
The main strength of our case report is complete work up of the patient, such as performing brain MRI and magnetic resonance venography (MRV), retinography and fluorescein angiography of eyes. However, the main limitation is the lack of investigating viral causes other than COVID-19.
3.1. Conclusions
In any child with clinical manifestation of IIH we should suspect COVID-19 infection besides ruling out other etiologies. In this issue, taking the history of contact with COVID-19 infected patients and performing virology tests are mandatory.