1. Introduction
In February 2020, the World Health Organization (WHO) declared coronavirus disease 2019 (COVID-19) as a pandemic. This disease was first seen in Wuhan, China, with a group of people who had pneumonia with an unknown cause, and then coronavirus was detected in the respiratory samples of these patients (1) and named the virus severe acute coronavirus 2 (SARS-CoV-2) (2).
The first published data focused on adults as the rate of infection in children was low, and the infected had a milder disease. Although myocardial involvement was reported from the beginning of the pandemic in adult patients, it was believed that pediatric patients are infected with a milder disease. Nonetheless, after a while cases of critically-ill children with COVID-19 who presented with Kawasaki-like symptoms were reported; thus, the WHO set a new definition as “multisystem inflammatory syndrome in children (MIS-C)” (3).
According to the definition, MIS-C is seen in children and adolescents aged up to 19 years, with a history of > 3 days fever, evidence of COVID-19 (positive RT-PCR or serology) or contact with positive cases of COVID-19, and two of the following diagnostic criteria: mucocutaneous symptoms (e.g., rash or bilateral non-purulent conjunctivitis), cardiovascular disorders (hypotension), myocardial dysfunction (according to ECHO findings or elevated troponin/NT-proBNP), hematology abnormalities (increased PT, PTT, and d-Dimers), acute gastrointestinal symptoms (diarrhea, vomiting, or abdominal pain), and laboratory data indicating inflammation (e.g., increased ESR, C-reactive protein, or procalcitonin), and with the exclusion of bacterial sepsis, toxic shock syndrome, Kawasaki disease, and other diseases (3).
Hypotension is seen in severe cases of MIS-C; myocardial involvement due to direct viral invasion, acidosis, hypoxemia, pulmonary hypertension, cytokine storm, or septic shock resulting in hypotension are some supposed etiologies for this condition (4).
To approach a pediatric patient with septic shock; generally, clinical assessment according to extremity temperature, capillary refill time, and pulses and pulse pressure has been recommended to differentiate “warm” versus “cold” shock. Warm shock is defined as normal or increased cardiac output (CO) and low systemic vascular resistance (SVR), which is most often seen in adult patients. Cold shock is described with low CO and increased SVR (5), and according to the type of shock, different strategies for resuscitation are used (e.g., vasopressors for warm shock and inotropes for cold shock) (6), but in the latest guideline issued by Surviving Sepsis Campaign recommended using advanced hemodynamic parameters (if available), in addition to bedside clinical variables to guide the resuscitation of children with septic shock (7).
The monitoring of hemodynamic status was performed by an arterial line in the femoral artery, and the catheter of central venous line was inserted into the internal jugular or subclavian vein. Then, they were linked to pulse contour cardiac output (PiCCO), which is an invasive monitoring device. Pulse Contour Cardiac Output uses a combination of two methods for progressive hemodynamic and volumetric monitoring as follows: transpulmonary thermodilution for volumetric quantities of preload and C.O and pulse contour analysis to run constant C.O, cardiac index (CI), SVR, MAP, pulse pressure variation (PPV), stoke volume variation (SVV), etc. (8).
Although it is assumed that children contract a milder disease, still our knowledge about the aspects of this disease, especially the severe forms, is lacking. Herein, we described the cases of three girls with COVID-19 presented with multi-system inflammatory syndrome and severe hypotension, who were treated successfully with the guidance of parameters derived from a continuous invasive hemodynamic monitoring device.
2. Case Presentation
2.1. Case 1
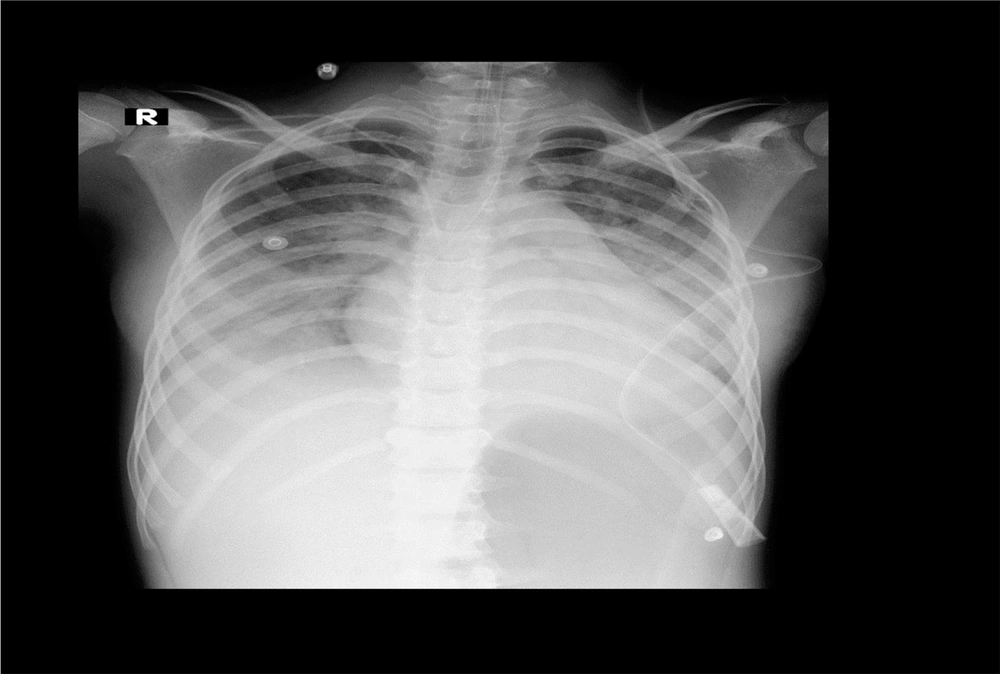
A 10-year-old previously healthy girl was referred to the emergency room (ER) of her local town’s hospital due to prolonged fever, diarrhea, and lethargy. A week before hospital admission, she had fever and abdominal pain and received some medications, but her condition did not improve, and three days before admission, she developed diarrhea and her condition aggravated. Thus, she was taken to the hospital. In the ER, her vital signs were as follows: blood pressure (BP): 90/40, heart rate (HR): 135, and respiratory rate (RR): 32. On physical exam, she had bilateral non purulent conjunctivitis, cervical lymphadenopathy, strawberry tongue, and erythema of the hands. Thus, with the diagnosis of atypical Kawasaki disease, she was moved to our pediatric intensive care unit at Nemazee Hospital, in Shiraz (Nemazee Hospital is a tertiary hospital with 750 beds that is located in south of Iran and has an 18-bed medical PICU and a 9-bed surgery PICU). On arrival, her vital signs were: BP:55/30, HR:158, RR: 35, and Glasgow coma scale (GCS): 7/15. She was intubated and inotrope was started, and RT-PCR for COVID-19 with nasopharyngeal swab was sent for her, the result of which was positive. Laboratory data is listed in Table 1. Her clinical criteria fulfilled the criteria of MIS-C (Figure 1).
| Patient# 1 | Patient# 2 | Patient#3 | |
|---|---|---|---|
| Ferritin (ng/mL), M: 22.81 - 275, F: 4.63 - 204 | > 2000 | 539 | |
| COVID realtime PCR | Positive | Positive | Positive |
| Typical chest CT finding | Patchy infiltration | Bilateral patchy ground glass | Diffuse and bilateral opacities |
| White blood cells (count/mL) | 25900 | 3300 | 22000 |
| Lymphocyte count | 950 | 260 | 1100 |
| Procalcitonin, ≤ 0.3 | 14.2 | 89.9 | 1.8 |
| C-reactive protein, < 6 (mg/L) | 150 | 105 | 30 |
| Creatine phosphokinase (U/L), M: < 171, F: < 145 | 322 | 2470 | 264 |
| Lactate dehydrogenase (U/L), < 480 | 664 | 1240 | 1350 |
| Troponin (ng/mL), < 19 | 62.5 | 1163 | 450 |
| D-Dimer (ng/mL), < 500 | 5193 | 2754 | 638 |
| Total bilirubin, 0.1 - 1.2 | 0.9 | 0.6 | 0.2 |
| Direct bilirubin, < 0.3 | 0.5 | 0.2 | 0.1 |
| Aspartate transaminase (U/L), M: < 37, F: < 31 | 55 | 114 | 97 |
| Alanine aminotransferase (U/L), M: < 41, F: < 31 | 37 | 42 | 13 |
| Albumin | 2.8 | 2.9 | 2.5 |
| Blood urea nitrogen (mg/dL), 8 - 20 | 24 | 30 | 53 |
| Creatinine, M: 0.8 - 1.3, F: 0.6 - 1.2 | 0.8 | 1 | 4.8 |
| Pt /INR | 17.1/1.27 | 24.1/1.79 | 17.9/1.33 |
| Ptt | 32 | 31.9 | 35 |
| Blood culture | Negative | Negative | Negative |
| ESR | 78 | 54 | 48 |
| Fibrinogen (200 - 400) | 426 | 411 | 580 |
| Stool culture/urine culture | Negative | Negative | Negative |
| SCVO2 | 78 | 91 | 68 |
The Initial Laboratory Data and Chest CT Scan Findings
Echocardiography findings indicated borderline left ventricle function and dilated inferior vena cava (IVC) (it was performed while high-dose inotrope was infusing).
Arterial and central venous lines were inserted and connected to the PiCCO. According to the hemodynamic data (Table 2), inotropes (dopamine and epinephrine) were increased, and vasoconstrictor was started; in addition to parenteral hydrocortisone, ascorbic acid, and thiamine were administered (HAT protocol). Fortunately, the patient responded well, the inotrope was tapered and discontinued, and she was discharged in an acceptable state.
| Normal Range | Patient#1 | Patient#2 | Patient#3 |
|---|---|---|---|
| Sys BP (mmHg) | 72 | 77 | 72 |
| Dia BP (mmHg) | 43 | 42 | 42 |
| MAP (mmHg) | 53 | 55 | 53 |
| CI (L/min/m2) | 4.39 | 4.34 | 2.6 |
| ITBI | 979 | 680 | 500 |
| ELWI (cc/kg) (3 - 7) | 14 | 6 | 11 |
| GEDI (cc/m2) (680 - 800) | 420 | 340 | 332 |
| SVRI (1700 - 2400) | 690 | 530 | 2240 |
| PPV (%) (0 - 10) | 9 | 12 | 11 |
| SSV (%) (0 - 10) | 11 | 17 | 22 |
| PVPI (1 - 3) | 3.9 | 2.2 | 1.9 |
The Initial PiCCO Parameters
2.2. Case 2
A 13-year-old girl was taken to the ER with the complaint of diarrhea, abdominal pain, and fever; three days before admission she presented with fever and abdominal pain, and on the day of admission, she presented with watery diarrhea. Her parents gave history that she had had up to 10 times watery diarrhea in the last hour, and she was taken to the hospital due to fecal incontinence. On arrival at the ER, vital signs were: BP: 110/65, HR: 152, RR: 22, and temperature: 40°C. She had GCS:13/15 and weak central pulses, so the infusion of dopamine was started, but due to the worsening of her condition (GCS dropped to 11 and BP to 90), she was intubated and transferred to the PICU (in ER, RT-PCR for COVID-19 with nasopharyngeal swab was taken, which showed positive results, and chest CT scan was done that was in favor of COVID-19).
Laboratory data (Table 1) and clinical signs and symptoms were in favor of MIS-C. In the PICU, C.V catheter was inserted, and epinephrine infusion was added. Echocardiogram revealsed poor left ventricle systolic function and borderline right ventricle systolic function with dilated IVC.
For constant hemodynamic observation, arterial line was placed into the femoral artery and connected to the PiCCO. According to low SVR, norepinephrine was started (HAT also was started) and titrated to acceptable MAP, and then vasopressin was added (the parameters are listed in Table 2).
Gradually, dopamine and epinephrine were tapered to discontinuation on day two, followed by norepinephrine and vasopressin. On the fifth day, she only received 0.2 µg/kg/min norepinephrine infusion, but due to severe ARDS, still, she needed mechanical ventilation till the 12th day that she was extubated and tolerated oxygen via non-rebreathing mask, and three days later she was transferred to the ward with a stable and acceptable condition.
2.3. Case 3
An 8-year-old girl was taken to the ER due to prolonged fever (four days), convulsion, and decreased level of consciousness (LOC). She also had a previous history of asthma.
On arrival to the ER: GCS:9/15, BP:85/40, HR:138, and RR:42 (laboratory data are listed in Table 1). The echocardiogram revealed fair left ventricle systolic function and moderate right pleural effusion. In the ER, her BP decreased to 55/20; thus, inotrope (dopamine) was started, and the patient was intubated and transferred to the PICU (RT-PCR for COVID-19 was positive).
In the PICU, she was connected to PiCCO with both arterial and C.V catheters; according to its data (Table 2), hydration and inotrope(epinephrine) were started. The inotrope was titrated, and the patient was extubated after four days. On the fifth day, inotrope was discontinued and the patient was discharged on the seventh day.
3. Discussion
In this report, we described successful treatment of three children with MIS-C and severe shock with the guidance of PICCO monitoring. This device defines our options for choosing inotropes or hydration for successful treatment.
Patients admitted to ICUs are at risk or have single or multiple organ failure. In such cases, we can use the traditional method: “HR, BP, central venous O2 saturation, central venous pressure (CVP), and urine output” or use the non-invasive or less invasive methods to direct our treatment (8).
Pulse contour cardiac output is a less invasive method with significant value when its variables are added to clinical variable in the right way and at the right time, and the patient has regular sinus rhythm and is fully sedated under controlled mechanical ventilation (6, 8, 9). In pediatric patients, intensivists typically treat septic shock with aggressive fluid administration and achieving the therapeutic goal of CI: 3.3 – 6.0 L/min/m2 (CI is generally low in pediatric septic shock with high SVR); in contrast to adult patients that have low SVR but CO is usually maintained or increased (6-10). As mentioned, we had a different plan for inotrope and hydration for each of our cases.
In the latest surviving sepsis guideline for critically-ill adult patients with COVID-19, it is recommended to use dynamic variables for hydration and norepinephrine infusion as the first-line vasoactive agent in adult patients with COVID-19 presenting with shock and vasopressin as the second line (11); our first two patients had vasodilatory shock although clinical data and diastolic pressure did not show that.
In our cases, we used the data derived from PiCCO in addition to frequent bedside echocardiography to decide about hydration and inotrope (Figure 1). The parameters of our patients were unique because there are no reported data of hemodynamic parameters in pediatric patients with MIS-C. Therefore, we compared our data with pediatric patients with septic shock.
In a study by Deep et al., non-invasive ultrasound cardiac output monitor device (USCOM) was used in 36 pediatric patients with either community-acquired or hospital-acquired sepsis; all of the hospital-acquired septic patients and three of community-acquired ones had low SVR, and the remaining had low cardiac output shock (CI < 3.3) (12).
Lee et al. conducted a study with PiCCO in 37 septic patients, the mean CI was 3.75 ± 1.08, the mean SVRI was 1327.34 ± 705.48, and SVV was 15 ± 6.5 (13). Ranjit et al. evaluated fluid refractory pediatric septic shock patients with clinical assessment, bedside echocardiography, and invasive BP monitoring. They found that 56.3% of the patients had warm shock, 85.5% had vasodilatory shock on invasive BP, and 29% initially presented with cold shock (14).
Ceneviva et al. reported 50 children with fluid-refractory (≥ 60 mL/kg in the first hour), dopamine-resistant shock. More than half of the patients (58%) showed a low CO/high SVR state, and 22% had low CO and low vascular resistance (15). Abdalaziz et al. studied 45 patients with community-acquired septic shock by bedside echocardiography and reported that 82% of their cases had the echocardiographic criteria of cold septic shock with low normal or low CI (≤ 3.3 L/m/m2) and normal or high SVRI (≥ 1,600 dyn-sec/cm5 /m2), whereas the remaining had the echocardiographic criteria of warm septic shock (high CI > 6 L/m/m2) with low normal or low SVRI (≤ 800 dyn-sec/cm5/m2) (16).
Hydration in the management of septic shock is a double-edged sword; it can correct relative hypovolemia, which is due to capillary leakage, not taking enough fluids, and fluid losses and maintain organ flow (9); on the other hand, overhydration may cause pulmonary edema or increase mortality (17).
The patients No. 1 and 2 had dilated IVC and low SVV and PPV; thus, there was no need for hydration; the initial CI was 4.39 in case 1 and case 2’s was 4.34, and SVRI was low in both patients (case 1: 690 dynes/seconds/cm5 vs 530 dynes/seconds/cm5 in case 2). Accordingly, norepinephrine was our first choice and was started and titrated up to 1.6 µg/kg/min in addition to vasopressin that was titrated to a high dose to taper norepinephrine. Although we used high doses of these vasoconstrictors, neither liver nor renal function impairment was seen in our patients, but the patient No. 3 was volume responsive (increased SVV,PPV) with low CI. Thus, the patient was hydrated, and epinephrine was started as an inotrope.
A vasodilatory shock associated with COVID-19 is seen in adult patients, which may be due to the dysfunction of angiotensin-converting enzyme (ACE) resulted from severe pulmonary endothelial damage in COVID-19 patients with acute respiratory distress syndrome (ARDS). Thus, some centers use angiotensin II infusion in vasodilatory shock in COVID-19 patients (18, 19), which can be one of the mechanisms used for hypotension in pediatric patients.
In the reported articles, PICU intubation rate in pediatric COVID-19 patients was 15 - 47% (20), while all of our patients were intubated in spite of not complaining of respiratory problem or respiratory symptoms in the first two patients. Only patient number 3 has refractory hypoxemia. PaO2/FiO2 ratio before intubation in case 1 was 273, and in case 2, it was 220 (but in case 2, 24 hours later it dropped to 112 and 62 on the third day), but patient No. 3 had a low PaO2/FiO2 ratio (150). On day three, patients No. 1 and 2 needed increased ventilator support, and the condition of case 2 worsened (PaO2/FiO2 ratio: 56). Patient No. 2 needed to increase peak end expiratory pressure up to 15 centimeters of water, and the median peak pressure reached 38 cm of water. The main problem in all of our patients was refractory hypoxemia.
In sum, we cannot solely rely on our traditional shock management that starts with dopamine or epinephrine, instead we should use methods to direct us in choosing the best inotrope or time for hydration. By increasing number of COVID-19 pediatric patients, PiCCO could be used successfully in critically-ill cases complicated with MIS-C for the appropriate management of shock and severe dehydration and judicious inotrope use. Additional studies are required on larger groups and with more accurate devices to provide further parameters to help clinicians in better hemodynamic management of this disease.