1. Background
Advanced liver failure is a devastating health condition with significant morbidity, mortality, and healthcare expenses. Cholestatic diseases, metabolic disorders, drug-induced or viral acute liver failure, chronic hepatitis, and malignancies are the leading causes of liver failure in pediatrics. Liver transplantation (LT) is the single effective cure for end-stage liver failure, dramatically increasing the life expectancy of the patients (1). Infections comprise a considerable proportion of post-transplantation complications. Post-transplantation infections considerably prolong hospitalization and increase mortality and morbidity, which is even comparable to graft rejection (2, 3). The rate of pediatric post-LT infections varies in different studies from 21% to 47% (4-6).
Bacteria are the most frequently isolated pathogens, followed by viruses and fungi (7, 8). Bacterial infections constitute a spectrum of disease severity ranging from superficial wound infections to sepsis (4). Due to the limitations of antibiotic therapy, the emergence of multidrug-resistant (MDR) organisms is of particular concern. Recurrent and prolonged hospitalizations, impaired immunity, and frequent previous use of antibiotics predispose pediatric liver recipients to colonize MDR species (9). Since there are significant differences among pediatric and adult patients regarding their susceptibility to various organisms and infection courses, caution is warranted in extrapolating the results of adult studies to pediatrics (10).
The proper antibiotic selection is based on the specific antibiotic resistance of pathogens and susceptibility patterns of centers. Therefore, the evaluation of infection rates among pediatric liver recipients is justified. This retrospective descriptive study was designed to provide an overview of bacterial infections during a one-year experience focusing on the incidence and type of isolated pathogens and infection risk factors in pediatric liver recipients in Shiraz Organ Transplant Center, Abu-Ali Sina hospital, as the single pediatric LT center in Iran.
2. Methods
2.1. Study Design and Patient Population
This retrospective descriptive study examined clinical and laboratory records of pediatric LT recipients in Abu-Ali Sina hospital, Shiraz, Iran, from April 2019 to February 2020. Inclusion criteria consisted of all children under 18 years of age who had undergone LT in the mentioned period and had been hospitalized for at least 48 hours after LT. Patients were excluded in the case of mortality under 48 hours after LT and simultaneous kidney and LT. All patients' medical and laboratory data were extracted from the hospital's electronic inpatient medical records. Demographic data, etiology of end-stage liver disease, and pediatric end-stage liver disease (PELD) (11) score or the model for end-stage liver disease (MELD) (12) score were recorded. The details of the LT technique were also noted, including the joining of the recipient vein inferior vena cava (IVC) to the donor IVC (Piggyback) for IVC reconstruction and biliary reconstruction performed via a duct-to-duct choledochocholedochostomy or Roux-en-Y hepaticojejunostomy. The other variables were the mean operating time, immunosuppressive regimens, length of ICU and hospital stay, readmission, rejection or re-transplantation episodes, and clinical outcome after transplantation. Furthermore, the clinical and laboratory data of the patients were evaluated and followed for one year after transplantation. The Ethics Committee of Shiraz University of Medical Sciences approved the study. All of the protocols were based on the ethical guidelines of the 1975 Helsinki Declaration (13). Written informed consent was obtained from all patients' parents or guardians.
2.2. Antibiotic Prophylaxis
After surgery, all patients were given ceftizoxime (150 mg/kg/day) and ampicillin-sulbactam (150 mg/kg/day) for three days. Prophylactic antibiotics were given to those who had bilioenteric anastomosis for five days. For the first six months following LT, all patients received trimethoprim/sulfamethoxazole (TMP/SMX) prophylaxis with 2 - 3 mg/kg TMP for Pneumocystis jiroveci prevention. Ganciclovir (10 mg/kg/day) and fluconazole (3 - 5 mg/kg/day) or valganciclovir (13 mg/kg/day) were used for fungal and viral (Cytomegalovirus) prophylaxis, respectively (14).
2.3. Immunosuppressive Regimen
A combination of tacrolimus, prednisolone, and mycophenolate mofetil was prescribed. Doses were adjusted considering the condition of the transplanted graft, drug plasma level, and the time passed from LT.
2.4. Microbiological Evaluation
Microbiological surveillance cultures of blood, sputum, urine, and abdominal fluid were based on clinical and laboratory results. A chest X-ray was taken for those suspected of having pneumonia. A conventional technique was used to obtain a blood culture. the BacT/ALERT 3D-automated blood culture system (bioMérieux, Durham, NC, USA) and the BACTEC FX (BD Diagnostic Systems, Sparks, MD, USA) (FX) were used for rapid microbial detection The Clinical and Laboratory Standards Institute (CLSI) guideline was used to interpret the results (15). The antibiotic resistance/sensitivity results in this study are based on the disk diffusion test.
2.5. Definition of Antibiotic-resistant Bacterial Species
The European Centre for Disease Prevention and Control's Consensus Statement was used to identify multidrug-resistant (MDR) and extended drug-resistant (XDR) microorganisms (14).
2.6. Statistical Analysis
All statistical analyses were performed using the statistical package for social sciences (SPSS Inc., Chicago, Illinois, USA) version 26.0. Descriptive statistics were presented as mean ± SD or proportions, as appropriate. Factors affecting the difference between the infected and non-infected groups were compared using a binary logistic regression model and multivariate analyses. The chi-square test or Fisher's exact test was used to compare the categorical data. The statistical tests used in the univariate analysis were Student's t-test and the Mann-Whitney U test. The multivariable linear regression included covariates significant (P < 0.05) in the univariate model. The possible associations between different demographic, clinical, and paraclinical characteristics of the study population and the development of infection were assessed by multivariate logistic regression analysis. In the first step, each independent variable was entered into the univariate model. In the next step, those with P < 0.05 in the univariate model were selected and entered into the final multivariable regression model.
3. Results
3.1. Patients
During the one-year examination, 84 pediatric patients had undergone LT, four of whom were excluded due to incomplete clinical records. Of 80 enrolled patients, 52 were male, and 28 were female, with a median age of 60 months. Fifty-five (67.9%) patients had at least one bacterial infection during hospital admission within one year after LT. Table 1 shows the demographic data, underlying liver disease, and important clinical variables in infected patients compared to non-infected ones (Table 1). The length of ICU stay, hospitalization period, mechanical ventilation duration, and re-hospitalization were significantly higher in the infected group than in non-infected pediatrics (P-value < 0.05). Multivariate regression analysis showed that the only risk factor for bacterial infections after LT was the length of ICU stay (Table 2).
| Variables | Total, N = 80 | Groups | ||
|---|---|---|---|---|
| Infected, N = 55 | Non-infected, N = 25 | P-Value | ||
| Age (mo) | 72.18 ± 48.48 | 70.18 ± 4971 | 88.40 ± 42.18 | 0.42 |
| Gender | 0.96 | |||
| Male | 52 (65) | 35 (67.3) | 17 (32.7) | |
| Female | 28 (35) | 19 (67.9) | 9 (32.1) | |
| BMI (kg/m2) | 18.00 ± 3.68 | 18.05 ± 3.81 | 17.88 ± 3.47 | 0.43 |
| Exploration surgery after Tx | 0.37 | |||
| Yes | 27 (33.8) | 20 (74.1) | 7 (25.9) | |
| No | 53 (66.2) | 34 (64.2) | 19 (35.8) | |
| Rejection | 0.25 | |||
| Yes | 22 (27.5) | 17 (77.3) | 5 (22.7) | |
| No | 58 (72.5) | 37 (63.8) | 21 (36.2) | |
| Underlying liver Dx | 0.08 | |||
| PFIC | 13 (16.3) | 11 (84.6) | 2 (15.4) | |
| Crigler-Najjar | 6 (7.5) | 3 (50) | 3 (50) | |
| Biliary atresia | 12 (15) | 11 (91.7) | 1 (8.3) | |
| Cryptogenic | 7 (8.8) | 5 (71.4) | 2 (28.6) | |
| Wilson disease | 15 (18.8) | 8 (53.3) | 7 (46.7) | |
| Others | 26 (32.5) | 15 (57.7) | 11 (42.3) | |
| Type of anastomoses | 0.50 | |||
| Duct to duct | 57 (72.2) | 37 (64.9) | 20 (35.1) | |
| Roux‐en‐Y hepaticojejunostomy | 22 (27.5) | 16 (72.7) | 6 (27.3) | |
| Type of surgery | 0.56 | |||
| Piggy back | 72 (91.1) | 49 (68.1) | 23 (31.9) | |
| Standard | 7 (8.9) | 4 (57.1) | 3 (42.9) | |
| Type of liver donors | 0.77 | |||
| Living donors | 69 (86.25) | 37 (53.6) | 32 (46.4) | |
| Cadaver | 11 (13.75) | 8 (72.7) | 3 (27.3) | |
| Re-transplantation | 3 (3.89) | 2 (66.6) | 1 (33.3) | 0.975 |
| PELD score | 20 | 21.52 ± 9.37 | 20.63 ± 13.3 | 0.762 |
| MELD score | 19.5 | 18 ± 1.41 | 25 ± 7.07 | 0.997 |
| CMV infection | 6 (7.78) | 4 (66.6) | 2 (33.3) | 0.999 |
| Length of hospital stay (days) | 24.01 ± 16.99 | 27.18 ± 18.69 | 17.42 ± 10.24 | 0.022 |
| Length of ICU stay (days) | 22.75 ± 15.87 | 26.62 ± 17.62 | 14.69 ± 6.11 | 0.003 |
| Length of mechanical ventilation after Tx (days) | 3.14 ± 2.39 | 3.88 ± 3.07 | 1.88 ± 0.77 | 0.016 |
| Length of operation (min) | 269 ± 60.15 | 274 ± 59.63 | 258 ± 60.79 | 0.245 |
| Re-hospitalization after Tx | 19 (23.75) | 18 (94.7) | 1 (5.3) | 0.017 |
| Tacrolimus level (ng/dL) | 10.33 ± 4.34 | 10.75 ± 4.20 | 9.36 ± 4.5 | 0.204 |
| Positive history of antibiotics usage in the past week before Tx | 27 (33.75) | 19 (70.37) | 8 (29.63) | 0.696 |
| Positive history of hospitalization in the past three months before Tx | 21 (26.25) | 13 (61.9) | 8 (39.1) | 0.525 |
| Immune suppressive regimen | 0.428 | |||
| Tacrolimus + prednisolone | 30 (78.94) | 21 (70) | 9 (30) | |
| Tacrolimus + prednisolone + cellcept | 38 (47.5) | 12 (31.57) | 26 (68.42) | |
| Cellcept + prednisolone | 30 (38) | 11 (36.7) | 19 (63.3) | |
| Prednisolone | 1 (1.3) | 1 (100) | 0 | |
| Cellcept + prednisolone + cyclosporin | 1 (1.3) | 1 (100) | 0 | |
| WBC count on admission | 9.03 ± 4.25 | 8.73 ± 4.09 | 9.96 ± 4.59 | 0.372 |
| WBC count after one week | 10.32 ± 5.79 | 10.37 ± 5.47 | 10.18 ± 6.61 | 0.898 |
| Positive stool VRE | 16 (25) | 13 (31.7) | 3 (13.04) | 0.199 |
| Death | 18 (22.5) | 10 (55.55) | 8 (44.44) | 0.008 |
Demographical and Clinical Features of Bacterial Infections Following Pediatric Liver Transplantation a
| Variables | OR | 95% CI | P-Value |
|---|---|---|---|
| Age | 1.009 | 0.996 - 1.021 | 0.176 |
| Length of ICU stay | 0.687 | 0.506 - 0.933 | 0.016 |
| Length of hospital stay | 1.232 | 0.948 - 1.601 | 0.118 |
| Length of mechanical ventilation | 1.211 | 1.00 - 1.519 | 0.124 |
| Re-hospitalization | 5.377 | 0.947 - 30.525 | 0.058 |
| Re-transplantation | 1.982 | 0.876 - 1.664 | 0.078 |
| Vascular anastomotic stenosis | 2.221 | 0.678 - 1.113 | 0.066 |
Multivariate Linear Regression of the Association Between Qualitative and Quantitative Variables and Infection Rate Among Pediatric Liver Transplant Patients (N = 80)
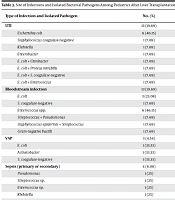
3.2. Infection Types and Isolated Bacteria
The mean time of infection after LT was 7.87 ± 3.32 days. Intra-abdominal surgical site infection (SSI) (24.24%), co-infection (19.69%), urinary tract infection (UTI) (19.69%), and bloodstream infection (19.69%) were the most common recorded infections. More than 64.06% of the isolated pathogens were Gram-negative, and 35.93% were Gram-positive. The most isolated pathogens were Escherichia coli (n = 19), Enterococcus spp. (n = 9), Staphylococcus spp. (n = 8), Pseudomonas spp. (n = 7), Streptococcus spp. (n = 6), Klebsiella spp. (n = 6), Acinetobacter spp. (n = 4), Enterobacter spp. (n = 2), Proteus mirabilis (n = 2), and Citrobacter spp. (n = 1). Besides, 24.39% of the isolated Gram-negative bacteria were extensively drug-resistant (XDR). Furthermore, 30.43% of Gram-positive bacteria were vancomycin-resistant Enterococci (VRE), and 8.69% were methicillin-resistant Staphylococcus aureus (MRSA). The most frequent site for isolated XDR pathogens was the abdomen (Table 3). Intra-abdominal SSI was the most common type of infection, which was detected during < 1 month and 1 - 6 months after LT, while UTI was more prevalent after six months of LT. The most isolated type of microorganisms during the first month after LT was E. coli spp. followed by Enterococci.
| Type of Infection and Isolated Pathogen | No. (%) | Frequency During Follow-up After LT | ||
|---|---|---|---|---|
| First Month | 1 to 6 Months | 6 to 12 Months | ||
| UTI | 13 (19.69) | 8 | 2 | 3 |
| Escherichia coli | 6 (46.15) | 4 | 1 | 1 |
| Staphylococcus coagulase-negative | 1 (7.69) | 0 | 1 | 0 |
| Klebsiella | 1 (7.69) | 1 | 0 | 0 |
| Enterobacter | 1 (7.69) | 1 | 0 | 0 |
| E. coli + Citrobacter | 1 (7.69) | 1 | 0 | 0 |
| E. coli + Proteus mirabilis | 1 (7.69) | 1 | 0 | 0 |
| E. coli + S. coagulase-negative | 1 (7.69) | 0 | 0 | 1 |
| E. coli + Enterococcus | 1 (7.69) | 0 | 0 | 1 |
| Bloodstream infection | 13 (19.69) | 7 | 4 | 2 |
| E. coli | 3 (23.08) | 0 | 2 | 1 |
| S. coagulase-negative | 1 (7.69) | 0 | 0 | 1 |
| Enterococcus spp. | 6 (46.15) | 4 | 2 | 0 |
| Streptococcus + Pseudomonas | 1 (7.69) | 1 | 0 | 0 |
| Staphylococcus epidermis + Streptococcus | 1 (7.69) | 1 | 0 | 0 |
| Gram-negative bacilli | 1 (7.69) | 1 | 0 | 0 |
| VAP | 3 (4.54) | 2 | 1 | 0 |
| E. coli | 1 (33.33) | 1 | 0 | 0 |
| Acinetobacter | 1 (33.33) | 0 | 1 | 0 |
| S. coagulase-negative | 1 (33.33) | 1 | 0 | 0 |
| Sepsis (primary or secondary) | 4 (6.06) | 3 | 0 | 1 |
| Pseudomonas | 1 (25) | 0 | 0 | 1 |
| Streptococcus sp. | 1 (25) | 1 | 0 | 0 |
| Enterococcus sp. | 1 (25) | 1 | 0 | 0 |
| Klebsiella | 1 (25) | 1 | 0 | 0 |
| Gastroenteritis | 4 (6.06) | 2 | 1 | 1 |
| Intra-abdominal surgical site infection | 16 (24.24) | 11 | 5 | 0 |
| E. coli | 2 (18.75) | 1 | 1 | 0 |
| Pseudomonas | 4 (37.5) | 3 | 1 | 0 |
| Streptococcus spp. | 2 (18.75) | 2 | 0 | 0 |
| Klebsiella | 1 (6.25) | 0 | 1 | 0 |
| S. epidermis | 1 (6.25) | 0 | 1 | 0 |
| Streptococcus + Pseudomonas | 1 (6.25) | 1 | 0 | 0 |
| Acinetobacter | 2 (18.75) | 2 | 0 | 0 |
| E. coli + Klebsiella + Enterococcus + P. mirabilis | 1 (6.25) | 1 | 0 | 0 |
| E. coli + Klebsiella + Enterobacter | 1 (6.25) | 1 | 0 | 0 |
| Acinetobacter + Klebsiella | 1 (6.25) | 0 | 1 | 0 |
| Coinfection | 13(19.69) | 8 | 2 | 3 |
| GE + VAP | 1 (7.69) | 1 | 0 | 0 |
| SSI + BSI | 4 (30.77) | 2 | 1 | 1 |
| VAP + BSI | 2 (15.38) | 1 | 1 | 0 |
| UTI + SSI | 3 (23.08) | 2 | 0 | 1 |
| BSI + SSI + VAP | 2 (15.38) | 1 | 0 | 1 |
| UTI + VAP | 1 (7.69) | 1 | 0 | 0 |
Site of Infections and Isolated Bacterial Pathogens Among Pediatrics After Liver Transplantation (N = 80)
4. Discussion
Bacterial infections are frequent and potentially life-threatening events following pediatric LT. This one-year retrospective study evaluated bacterial infections in 80 pediatric post-LT patients. In this study, a 67.9% bacterial infection incidence was observed, which was higher than in a previous study from Iran, reporting an incidence of 54.3% among pediatric LT patients (16). Our findings are nearly the same as the reports from other centers regarding LT in pediatrics (70.8% in France, 70% in Canada, and 51.9% in Germany) (17-21). In a 23-year, retrospective, single-center study conducted by Kukreti et al., 28% of the pediatric LT patients developed infections during their early critical care course; meanwhile, 79% of the infections were of bacterial source (22). The incidence of bacterial infections, especially in the early post-LT period, is of significance. In another study of 2,291 pediatric LT patients, infections were the most common cause of overall mortality, causing more deaths than rejection (5.5% vs. 0.6% of patients). In the study, 38% of patients developed serious fungal and bacterial infections during the first six months after LT. Bacterial infections constituted the majority of documented infections. Interestingly, Shepherd et al. assessed risk factors for rejection and infection in pediatric LT, showing that a reduced size or split donor's liver was associated with an increased risk of bacterial infections (23).
High immune-suppressive doses in response to rejection, lengthy and complicated surgical procedures, multiple microorganism access routes (e.g., drainage tubes, catheters, and incisions), and the patient's poor health state are risk factors associated with bacterial infections in pediatric LT patients, particularly in the early postoperative period (6, 17, 18, 22, 24).
When we compare our study with other national studies of adult patients, the rate of bacterial infections after LT is higher in children than in adults. In this regard, Jafarpour et al. and Shafiekhani et al. studies reported the incidence of infections following LT as 38.6% and 25.4%, respectively. One of the reasons for this difference is the variation in causal pathogens, which may fluctuate based on age range or different LT methods used for pediatrics compared to adults, which requires additional manipulation in the abdominal cavity, subsequently predisposing the patient to more abdominal and SSIs (25, 26).
In our study, 64.06% of the isolated pathogens were Gram-negative, and 35.93% were Gram-positive, which is inconsistent with a previous study from Iran (49% Gram-negative vs. 51% Gram-positive organisms). In a previous Iranian study, Enterococcus spp. (36.1%) and Staphylococcus spp. (11.1%) were the predominantly isolated Gram‐positive bacteria, and Enterobacteriaceae (21.3%) and Acinetobacter spp. (16.7%) were the most prevalent Gram‐negative ones (27-29). Gram-negative predominance may have various reasons, including longer ICU stay, longer duration of mechanical ventilation, the possibility of post-LT renal failure and hemodialysis, history of preoperative broad-spectrum antibiotics in recurrent hospitalizations, and biliary tract manipulation during surgery (27, 28). In contrast, some studies showed the predominance of Gram‐positive bacteria (18, 30, 31). For instance, in a study by Bouchut et al. in France, 78% of the isolated bacteria from pediatric post-LT patients were Gram-positive, with S. aureus (32%) and Staphylococcus epidermidis being the most prevalent ones (32% and 26%, respectively). In the mentioned study, all patients had received gentamicin, polymyxin, and nystatin during their ICU stay for selective intestinal decontamination. The administration of these antibiotics could have altered the bacterial prevalence (18).
The emergence of antibiotic-resistant bacterial species such as MDR, XDR, and VRE in post-transplantation infections is of great concern. Our study showed that about 25% of the isolated Gram-negative bacteria were of XDR type, confirming the results of previous studies (26, 32, 33). The increasing prevalence of resistant pathogenic species not only affects the efficiency of common antibiotic regimes but also increases the mortality rate (34-36). Inappropriate empirical administration of antibiotics, long hospital and ICU stays, frequent use of broad-spectrum antibiotics such as carbapenems and fluoroquinolones for treating spontaneous bacterial peritonitis before LT, and hemodialysis or Continuous Renal Replacement Therapies (CRRT) after LT are among the risk factors for emerging resistant pathogens after transplantation (27, 34). Among Gram-positive bacteria, 31% belonged to VRE in our study. In a study by Pouladfar et al. conducted in the previous pediatric LT center in Shiraz, Iran, 82% of the isolated Enterococcus species were VRE (16). The high prevalence of VRE and other antibiotic-resistant pathogens indicates an increase in nosocomial infections.
In our center, intra-abdominal and SSI was the most common site of infection in post-LT patients (24.24%). The urinary tract (19.69%) and bloodstream (19.69%) were the other common sites of bacterial infections. Previous studies have reported the abdomen and bloodstream as the two most common bacterial infection sites in pediatric patients hospitalized shortly after LT. Complex surgical procedures, the requirement to insert intra‐abdominal drainage tubes, and central venous catheters are the major causes facilitating bacterial entry to the abdomen and blood (18, 21, 22).
In our study, the length of ICU and hospital stay, duration of mechanical ventilation, re-hospitalization, and mortality rate were significantly higher in the infected group than in the non-infected one. Furthermore, multivariate regression analysis showed that the only risk factor for bacterial infections in pediatric post-LT patients was the length of ICU stay. Longer hospitalization and ICU stay have been formerly shown to be associated with increased incidence of infection in post-LT patients (16, 37, 38).
Our study demonstrated that mortality was higher among the infected group than in the non-infected group, in line with other reports demonstrating that bacterial and viral infections were important causes of mortality after LT (39). This issue is important when some studies have suggested multidrug-resistant pathogens are the leading cause of death due to infection (4). Therefore, it is essential to establish and implement antibiotic stewardship programs to reduce MDR and XDR pathogens.
Although our study revealed that the tacrolimus level was higher in the infected group than in the non-infected group, no statistical significance was observed. Dohna Schwake et al. stated that tacrolimus levels of 20 ng/ml or higher were associated with an increased risk of bacterial infections, especially sepsis, septic shock, and SSI. However, this may be due to the complete avoidance of steroids in the absence of rejection in their study; consequently, tacrolimus level targets might have been higher (4). Some studies have also shown that the living donor versus the deceased one may be a risk factor for infection, but the effect of this risk factor was not observed in our study. Although there is more concern about viral infectious disease transmissions such as CMV and HSV, bacterial pathogens can also be transmitted through donors. Some studies have reported that the rate of post-transplant infections in the deceased donor was higher than in the living donor because when active donors are used, active surveillance is more likely to detect bacterial and viral infections. In this way, infections transmitted through the donor can be minimized, but when using a deceased donor, there might not be enough time to evaluate active infections because the organ must be removed in the shortest possible time. On the other hand, because the donor has a long history of hospitalization before death, there is an increased chance of colonization with resistant pathogens (40, 41). However, our center prioritizes the first living relative donor over deceased donors for pediatric LT; therefore, it is impossible to accurately distinguish between these two types of donors regarding the risk of bacterial infections after transplantation. Our results demonstrated no significant association between CMV infection with the rate of bacterial and other infections among pediatrics, contradicting reports from several studies. This may be due to the low sample size and one-year follow-up of our patients (42, 43).
To sum up, this study warns of an increasing trend in the prevalence of nosocomial antibiotic-resistant bacterial infections among pediatric LT patients. Gram-negative bacteria exceed the Gram-positive ones in the early post-LT period in pediatrics of our center. The length of ICU stay was associated with bacterial infections. Excessive empirical use of antibiotics leads to the development of antibiotic-resistant bacteria. Intra-abdominal and SSIs were the most common sources of bacterial infections in our pediatric LT recipients.
In re-transplant patients, the risk of infection may expectedly increase due to repeated surgery with all accompanying risks and the increasing use of immunosuppressive drugs after the second transplantation to prevent relapse (44). Because only three patients were re-transplanted, it was practically impossible to study this variable in our study.
However, our study has some limitations. One of them is the use of the disk diffusion method to measure the pattern of antibiotic susceptibility/resistance, while more accurate results would be achieved with the ETEST method. The design was retrospective, which was accompanied by incomplete data in hospital records. Some cases are not observed in hospital records because of asymptomatic infection or no need for hospitalization. Furthermore, we did not evaluate our patients' long-term outcomes and prognoses. Also, it should be noted that viral and fungal infections were not assessed in our study. Another limitation is the absence of donor-related infectious information.
4.1. Conclusions
Pediatric patients in the immediate postoperative period after LT have a high risk of bacterial infections, increasing their morbidity and mortality. In the early days after LT, there was a significant rate of bacterial infections among hospitalized children. Longer hospital stays were linked to these infections. However, there was no other risk factor associated with contracting an infection in multivariate analysis.