1. Background
Coronavirus disease 2019 (COVID-19) was declared a pandemic in March 2020 by World Health Organization (WHO), soon after the first reports in China (1). Its dramatic rapid spread with considerable mortality and morbidity affected healthcare systems worldwide, even in fields not directly related to this infection (2). To minimize COVID-19 burden, many countries exerted nationwide lockdowns restricting access to medical centers for conditions other than COVID-19 (3-5).
Despite a significant improvement in the management of premature neonates, the complication of low birth weight and preterm labor are still noticeable (6). Besides, common multi-organ complications of prematurity, prolonged hospitalization, mechanical ventilation, broad-spectrum antibiotic therapies, and prenatal nutrition have several adverse effects. Therefore, it is reasonable to delineate factors affecting the pregnancy period to design more effective preventive guidelines for premature births (7-9). Recently, a study showed a significant reduction in premature births during COVID-19 lockdowns. Some probable factors were suggested to explain this reduction; however, the main reasons remained unclear (10).
2. Objectives
This study aimed to determine the prevalence of preterm births and complications of prematurity during the first year of COVID-19 pandemic compared with the previous year.
3. Methods
3.1. Study Design and Setting
This cross-sectional study was conducted at Mahdiyeh hospital, Tehran, Iran. We included all live births recorded in the Mahdiyeh hospital from March 2019 to March 2021. Live births were recorded from March 2020 to March 2021 that occurred during the first year of COVID-19 pandemic.
3.2. Data Collection
Data were collected by the census method. We reviewed medical records to extract the prevalence of preterm births and prematurity complications. Neonates were categorized regarding their gestational age (GA) (weeks + days) as follows: extremely premature (< 27w + 6d), very premature (28w, 31w + 6d), moderate or late premature (32w, 36w + 6d), term (37w, 41w + 6d), and late term (> 42w). Also, the following complications of prematurity were reviewed: Sepsis, intraventricular hemorrhage (IVH), retinopathy of prematurity (ROP), and respiratory distress syndrome (RDS).
3.3. Data Analysis
Data were analyzed with SPSS (version 26). Descriptive data were reported as frequency and percentage. We used Chi-square test to compare variables between categories. Also, a P-value < 0.05 was considered statistically significant.
3.4. Ethical Considerations
This study was approved by the Institutional Research Ethics Committee Vice-Chancellor in Research Affairs of Shahid Beheshti University of Medical Sciences (approval ID: IR.SBMU.RETECH.REC.1399.1270). The study was a project based on the Helsinki Declaration 2000.
4. Results
A total of 10,830 live births were included in this study (5,232 were recorded after COVID-19 pandemic). Table 1 shows the prevalence of live births based on GA in detail. During COVID-19 pandemic, the prevalence of moderate or late prematurity had a 4.64% reduction compared with the previous year (P < 0.001). Besides, the prevalence of term labor during COVID-19 pandemic increased by 5.37% compared with the previous year (P < 0.001). In contrast, the prevalence of births among other GAs had no difference between the two periods. Overall, there was a significant association between the prevalence of births and gestational age (P < 0.001).
| Categories | Gestational Age; (Weeks + Days) | 2019 - 2020; No. (%) | 2020 - 2021; No. (%) | Risk Difference (%) a | P-Value b |
|---|---|---|---|---|---|
| Extremely premature | < 27 + 6 | 109 (1.95) | 81 (1.55) | -0.40 | 0.124 |
| Very premature | 28 - 31 + 6 | 146 (2.60) | 109 (2.08) | -0.52 | 0.072 |
| Moderate/ late premature | 32 - 36 + 6 | 948 (16.94) | 644 (12.30) | -4.64 | < 0.001 |
| Term | 37 - 41 + 6 | 4170 (74.5) | 4179 (79.87) | 5.37 | < 0.001 |
| Late term | > 42 | 225 (4.01) | 219 (4.20) | 0.19 | 0.676 |
| Total | - | 5598 (100) | 5232 (100) | - | - |
a Here we calculated the risk difference after-before.
b Data were analyzed with chi-square test.
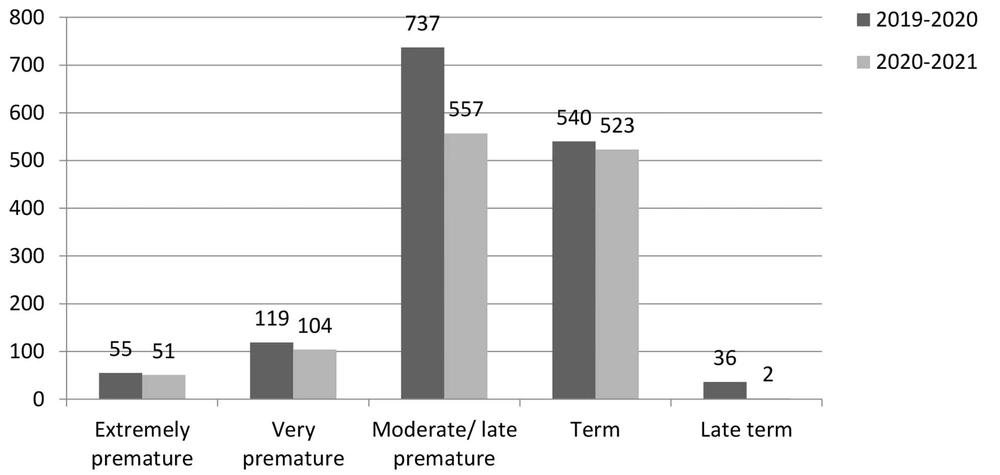
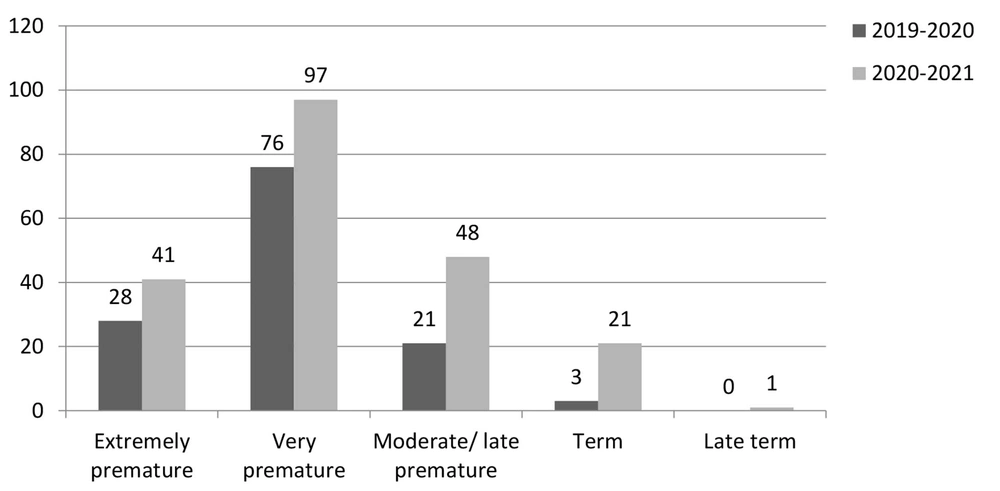
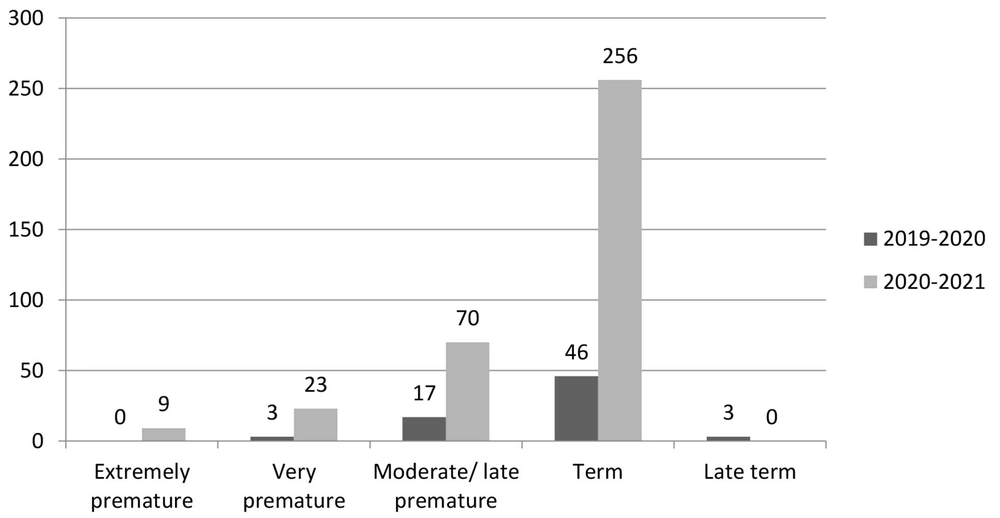
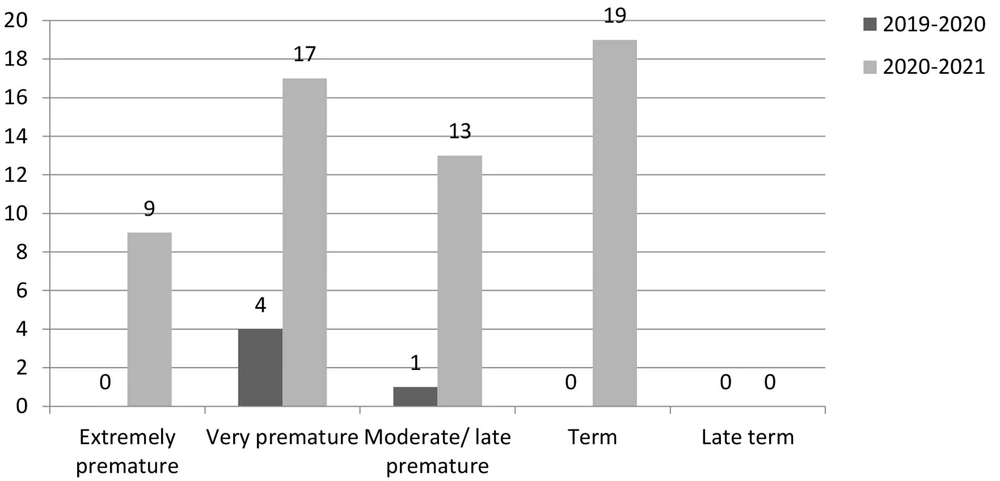
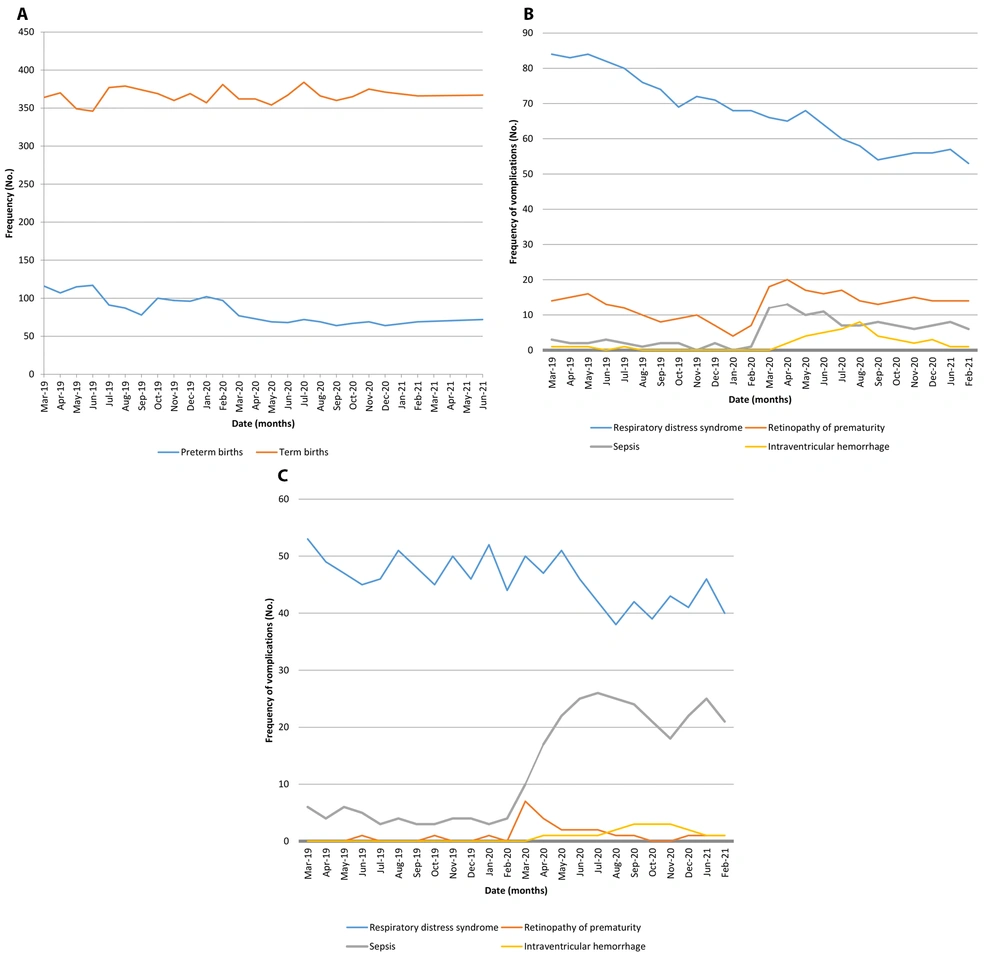
The prevalence of RDS decreased significantly during COVID-19 pandemic compared with the previous year (23.64% vs. 26.56%, P < 0.001). The prevalence of ROP significantly increased during COVID-19 pandemic compared with the previous year (3.97% vs. 2.28%, P < 0.001). Additionally, sepsis was significantly more prevalent during COVID-19 pandemic compared with the previous year (6.84% vs. 1.23%, P < 0.001). Moreover, IVH significantly increased during COVID-19 pandemic in comparison to the previous year (1.10% vs. 0.08%, P < 0.001). Figures 1 - 4 show the frequency of prematurity complications (RDS, ROP, sepsis, and IVH, respectively) based on gestational age. Also, Figure 5 shows time trend of preterm/term births and complications of prematurity.
5. Discussion
Our study aimed to determine the prevalence of preterm births and complications of prematurity during the first year of COVID-19 pandemic compared with the previous year. Like the previous study (10), our results revealed that the prevalence of both preterm and term births altered during COVID-19 pandemic. Based on our results, late preterm pregnancies decreased obviously, in exchange for the increase in term births. We also assessed common complications of hospitalized neonates in both years. Our results noticed a considerable change in the above complications during the pandemic period. Although ROP and IVH increased during COVID-19 pandemic, they are unexplainable by the COVID-19 pathogenesis. These conditions are multifactorial and may be caused by hospitalization events. On the other hand, sepsis and RDS could be affected by prenatal care, which changed strongly during COVID-19 lockdowns.
This was the first study determining the prevalence of preterm births during COVID-19 pandemic in Iran. Since Mahdiyeh hospital is the major obstetrics and neonatal care center in the capital of Iran, Tehran, a large number of samples were available. Furthermore, no previous studies evaluated neonatal complications during national lockdowns. The duration of lockdown was short, and commitment to hygiene protocols was not satisfying for many months of the pandemic based on national surveys. These different situations in Iran led us to carry out this research.
Preliminary studies in European countries showed almost consistent outcomes with our findings. In the study by Been et al., the prevalence of preterm births was determined after lockdown implementation in the Netherlands. In this study, a significant reduction was observed in preterm births after mitigation measures. Besides, the prevalence of preterm births was not associated with socioeconomic status (6). A similar study in Denmark by Hedermann et al. revealed a substantially lower rate of extremely premature infants in contrast with the previous five years in which 3,1180 singleton births were assessed, and no considerable changes were observed among other GA groups (3). In another study by Philip et al. in Ireland, the rate of very low birth weight (VLBW) and preterm infants in the previous two decades were calculated. A significant reduction was revealed in preterm and VLBW neonates from January to April 2020. This study was conducted in a single health area, and preterm births were not categorized with GA (11). However, the impact of COVID-19 and lockdown on preterm births is controversial. Based on a meta-analysis by Vaccaro et al., conflicting results have been reported from 13 previous studies focusing on preterm births during COVID-19 lockdown. They stated an increase and a decrease in the incidence of preterm births, with odds ratios (95% confidence interval) between 0.09 (0.01 - 0.40) and 1.93 (0.76 - 4.79) (12).
Preterm labor is a multifactorial phenomenon (13). Both genetic and environmental factors can lead to this condition. To reduce this overwhelming problem, it is reasonable to decrease modifiable risk factors (14). It seems that focusing on self-hygiene, social distancing, less transportation, and less work stress may reduce the number of preterm births. However, the socioeconomic status may be altered drastically during lockdowns, leading to adverse health issues (15-17). COVID-19 pandemic affected healthcare systems dramatically worldwide. Caregivers and health facilities focused more on COVID-19 patients. As a result, access to health providers may be more difficult for conditions other than COVID-19, which may have consequences. Thus, further studies are needed to delineate the exact effect of COVID-19 management policies on preterm births.
Our study had some limitations. First, this was a single-center study, but a national survey with a further population may lead to different results. Second, due to the restriction of previous studies, the findings could not be completely interpreted and discussed. Third, we performed a cross-sectional study. Due to the study design, the impact of COVID-19 lockdown on the prevalence of preterm birth and prematurity complications could not be assessed. Thus, we suggest performing analytical studies in the future.
5.1. Conclusions
The prevalence of preterm birth decreased during COVID-19 lockdown. Also, major complications of prematurity such as RDS, ROP, sepsis, and IVH may be affected by COVID-19 lockdown.