1. Background
It has been more than a year since the first case of severe pneumonia in Wuhan Seafood Market was reported. Shortly after, it spread worldwide and was renamed coronavirus disease 2019 (COVID-19) (1). SARS-CoV-2 is the primary culprit virus behind COVID-19 and the associated 21st-century pandemic. Its pathogenesis has been partially understood, and its etiology remains unclear (2). Its clinical manifestations could vary from common cold symptoms to acute respiratory distress syndrome (ARDS) and respiratory failure, resulting in death (3). Although preliminary data have focused on respiratory manifestations, other organ-specific symptoms have been reported, such as infiltration to the central nervous system (4), cardiac muscle (5, 6), and GI tract involvement (7-9). In the beginning, most research was done on adults, and data were insufficient to decide on COVID-19 manifestation in children.
From several aspects, children are more vulnerable to COVID-19. First, younger children are less able to express their symptoms and chief complaint. Second, children cannot control their contact with others and the environment. Third, therapeutic aspects in children are associated with limitations due to their more sensitive conditions in terms of growth, development, and prevention in different aspects such as vaccination, social distancing, and face mask use (5). The issues highlight the importance of research and data collection on the effects of COVID-19 on children (10). It was initially thought that children were less likely to be affected by SARS-CoV-2 infection. However, with the advent of new data, it was clear that children are also affected by SARS-CoV-2 infection, and their situation may even become critical and require hospitalization or intensive care. Due to past reports, SARS-CoV-2 infection and COVID-19 presentation in children is milder, and recovery is faster (although moderate to severe complications could also present). On the other hand, children of all ages are susceptible to COVID-19 (5, 11-14). In general, the most common symptoms reported in children are respiratory involvement in the form of fever and cough, muscle aches, runny nose, headache, nausea and vomiting, abdominal pain, diarrhea, and loss of taste or smell. In the meantime, GI symptoms may even occur without respiratory symptoms. Diarrhea, vomiting, and abdominal pain are children’s most common GI symptoms (5, 11, 13-16).
It also has been shown that SARS-CoV-2 is excreted in the feces of COVID-19 patients, and even the duration of excretion through feces can be longer than its presence in respiratory droplets. However, it has not yet been confirmed that the virus can be transmitted through the fecal-oral route (17, 18). This is supported by evidence that different parts of the GI tract express the angiotensin-converting enzyme 2 receptor, which is the main receptor for SARS-CoV-2 to enter the cell and initiate the infection (17, 19). Furthermore, GI manifestations of COVID-19 are also part of a life-threatening condition named multisystem inflammatory syndrome in children (MIS-C), which can progress to shock and multiple organ failure (20-22). Also, SARS-CoV-2, like other coronaviruses, can cause liver injury with mild to moderate elevation in aminotransferases, mild sinusoidal lymphocytic infiltration, and sinusoidal dilatation in COVID-19 patients; but significant damage is rare in the liver (23). Moreover, mild liver injury is frequently associated with moderate to severe illness in COVID-19 patients (24). Based on this, as well as the functional and anatomical correlation of the liver and GI tract, it is important to study COVID-19 hepatic manifestations along with GI manifestations.
Despite valuable information from previous studies, the question “Which GI symptoms and laboratory data are more common in COVID-19 patients and suggest COVID-19 as a differential diagnosis?” remains unanswered. In practice, a set of GI symptoms and routine laboratory data at the patient’s bedside suggests many differential diagnoses, including COVID-19. Herein, we investigated 184 children with non-specific symptoms (focusing on GI and hepatic symptoms) concerning SARS-CoV-2 real-time PCR (RT-PCR) results and disease outcomes. We attempted to link clinical presentations and lab data of cases having positive PCR tests.
2. Methods
This cross-sectional study was performed from 20 March 2020 to 20 November 2020. Data from 184 patients with GI and hepatic symptoms referred to the Pediatric Emergency Department of Shiraz Namazi Hospital were collected considering the study criteria. A convenience sampling method was administrated. The study design is summarized in Figure 1.
The inclusion criteria for detailed medical review included hospitalization with GI and hepatic symptoms from 20 March 2020 to 20 November 2020 and age under 18 years. The exclusion criteria included asymptomatic patients with positive test results, parents’ dissatisfaction with participating in the study, patient death before complete data collection, an incomplete patient file, and age under one month.
Positive GI symptoms in patients are defined as having at least one of the following symptoms: Diarrhea (watery or bloody diarrhea), vomiting (bilious or non-bilious), nausea, acute abdominal pain, and hematemesis. Also, hepatic symptoms in patients are defined as jaundice, itching, anorexia, and abdominal distention as chief complaints on admission. As mentioned, patients’ symptoms were recorded on admission to prevent the effect of unwanted and uncontrolled factors such as medical therapy side effects and symptom development during hospitalization.
This study focused on signs and symptoms (with special consideration of GI and hepatic manifestations) on admission. Then, we collected demographic information, clinical data (besides the chief complaint), and laboratory records and classified children into four groups (based on symptoms of the complicated systems):
(1) Cirrhotic children with decompensated cirrhosis
(2) Children with inflammatory bowel disease (IBD) exacerbation
(3) Children with gastroenteritis
(4) Children with acute abdominal pain
It is noteworthy that our study was designed in late 2019, while MIS-C was first identified in April 2020. Hence, MIS-C criteria were hard to consider at that time. However, according to the patient’s recorded data, we could confirm if any MIS-C case should be included in the further survey.
2.1. Lab Data
The SARS-CoV-2 RT-PCR test was performed on the patient’s oropharyngeal and nasopharyngeal swab samples. All laboratory procedures were conducted at the Shiraz University of Medical Sciences Laboratories.
2.2. Ethical Considerations
This study was done under the careful consideration of local medical ethical codes. The parents signed informed consent forms for all patients participating in this study. It was also ensured that no intervention would be made outside the framework of common guidelines. In addition, the data obtained in this study will be available to other researchers for further study. Moreover, this study was approved by the Institutional Ethics Board of Shiraz University of Medical Sciences (Approval No. IR.sums.med.rec.1399.625).
2.3. Statistical Analysis
Statistical analysis was done using SPSS 22. Quantitative and qualitative data were described using mean (standard deviation) and relative frequency, respectively. Research questions were answered using the chi-square and Easy Fisher Exact tests for Tables 1 - 4, and an independent t test for Table 5. P value < 0.05 was considered significant.
| Symptoms on Admission | Positive PCR Test (n = 51) | Negative PCR Test (n = 133) | P Value |
|---|---|---|---|
| Watery diarrhea | 0.043 a | ||
| Yes | 2 | 21 | |
| No | 49 | 112 | |
| Intractable vomiting | 0.044 | ||
| Yes | 7 | 37 | |
| No | 44 | 96 | |
| Abdominal pain | 0.922 | ||
| Yes | 7 | 19 | |
| No | 44 | 114 | |
| Dysentery | < 0.001 a | ||
| Yes | 11 | 2 | |
| No | 40 | 131 | |
| Gastrointestinal bleeding | 1 a | ||
| Yes | 1 | 4 | |
| No | 50 | 129 | |
| Jaundice | 0.349 a | ||
| Yes | 3 | 3 | |
| No | 48 | 130 | |
| Diarrhea + abdominal pain | 0.021 a | ||
| Yes | 4 | 1 | |
| No | 47 | 132 | |
| Vomiting + abdominal pain | 0.418 | ||
| Yes | 8 | 15 | |
| No | 43 | 118 | |
| Diarrhea + vomiting + fever | 0.038 a | ||
| Yes | 5 | 3 | |
| No | 46 | 130 | |
| Diarrhea + vomiting | 0.447 a | ||
| Yes | 1 | 7 | |
| No | 50 | 126 | |
| Anorexia | 0.194 a | ||
| Yes | 0 | 7 | |
| No | 53 | 126 | |
| Abdominal distension | 1 a | ||
| Yes | 1 | 2 | |
| No | 52 | 132 | |
| Abdominal distension + vomiting | 0.107 a | ||
| Yes | 0 | 8 | |
| No | 53 | 125 | |
| Jaundice + vomiting | 1 a | ||
| Yes | 1 | 4 | |
| No | 52 | 129 | |
| Total | 51 | 133 | - |
a Easy Fisher Exact Test for evaluating the P value.
| Underlying Disease | Positive PCR Test (n = 51) | Negative PCR Test (n = 133) | Total |
|---|---|---|---|
| No underlying disease | |||
| Yes | 40 | 84 | 0.071 |
| No | 11 | 49 | |
| Cystic fibrosis | |||
| Yes | 0 | 10 | 0.064 a |
| No | 51 | 123 | |
| Cirrhosis | |||
| Yes | 8 | 25 | 0.622 |
| No | 43 | 108 | |
| Lupus | |||
| Yes | 0 | 1 | 1 a |
| No | 51 | 132 | |
| Liver transplant | |||
| Yes | 1 | 8 | 0.448 a |
| No | 50 | 125 | |
| Cerebral palsy | |||
| Yes | 1 | 0 | 1 a |
| No | 50 | 133 | |
| Inflammatory bowel disease | |||
| Yes | 1 | 4 | 1 a |
| No | 50 | 129 | |
| Major thalassemia | |||
| Yes | 0 | 1 | 1 a |
| No | 51 | 132 |
a Easy Fisher Exact Test
| Computed Tomography Scan Finding | Positive PCR Test (n = 51) | Negative PCR Test (n = 133) | P Value |
|---|---|---|---|
| Normal | |||
| Yes | 11 | 48 | 0.058 |
| No | 40 | 85 | |
| Collapse consolidation | |||
| Yes | 2 | 5 | 1 a |
| No | 49 | 128 | |
| Reticulonodular | |||
| Yes | 2 | 0 | 0.075 a |
| No | 49 | 133 | |
| Consolidation | |||
| Yes | 1 | 2 | 1 a |
| No | 50 | 131 | |
| Ground-glass opacity | |||
| Yes | 5 | 1 | 0.006 a |
| No | 46 | 132 | |
| Bronchiectasis | |||
| Yes | 0 | 1 | 1 a |
| No | 51 | 132 | |
| Abscess | |||
| Yes | 1 | 0 | 1 a |
| No | 50 | 133 | |
| Total | 22 | 57 |
a Easy Fisher Exact Test
| Cumulative Symptoms on Admission | Positive PCR Test | Negative PCR Test | P value |
|---|---|---|---|
| Diarrhea | 0.010 | ||
| Yes | 23 | 34 | |
| No | 28 | 99 | |
| Vomiting | 0.128 | ||
| Yes | 22 | 74 | |
| No | 29 | 59 | |
| Abdominal pain | 0.494 | ||
| Yes | 20 | 45 | |
| No | 31 | 88 | |
| Total | 51 | 133 |
| Laboratory Finding | Positive PCR Test (n = 51) | Negative PCR Test (n = 133) | P Value a |
|---|---|---|---|
| WBC count | 12447 | 12072 | 0.00001 |
| Lymphocyte count | 2642 | 3021 | 0.001 |
| ESR | 34 | 26 | 0.037 |
| CRP | 80 | 40 | 0.002 |
a Independent t test
3. Results
3.1. Statistical Population
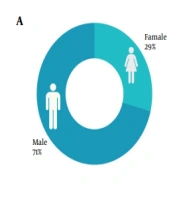
In this cross-sectional study, 184 patients were studied from 20 March to 20 November 2020 according to inclusion criteria. The mean age was 62 ± 64 months (2 to 215 months). The subjects included 108 (58%) males and 76 (42%) females (Figure 2A and Table 1).
Since the underlying disease is involved in GI and hepatic symptom development and COVID-19 treatment and outcome, it was examined in all patients. It was found that 33 (18%) patients had cirrhosis, 10 (5%) patients had cystic fibrosis, and 9 (5%) patients had liver transplantation (2 patients because of progressive familial intrahepatic cholestasis, 3 patients because of biliary atresia, and 4 patients because of cryptogenic cirrhosis). In addition, 5 (3%) patients had IBD (three with Crohn’s disease and 2 with ulcerative colitis) (Figure 2B and Table 2).
The most common GI symptoms among patients were vomiting (96 patients), watery diarrhea (44 patients), and dysentery (13 patients) (Figure 2C and Table 1).
Besides, 157 (85%) patients had no respiratory symptoms besides GI symptoms (cough, dyspnea, and tachypnea). Ten (5%) patients presented with cough, 7 (3%) with dyspnea, and 10 (5%) with both symptoms. In addition, 3 patients were intubated upon arrival at the hospital.
In the physical examination, 87 (47%) patients had no specific finding. The most common clinical findings were cirrhosis-related signs (mainly jaundice) observed in 30 (16%) patients. Other clinical findings included abdominal tenderness (19%), respiratory signs (tachypnea) (10%), and dehydration (3%). According to the result, 22 of 51 PCR-positive patients had both respiratory and GI symptoms.
3.2. Common Symptoms Among Patients with Positive PCR Test
All 184 patients were tested for SARS-CoV-2, showing 51 (28%) positive results in 36 boys and 15 girls. The mean age was 54 months in patients with positive SARS-CoV-2 and 69 months in negative patients.
The most common symptoms in SARS-CoV-2 PCR-positive patients were vomiting (22 patients), watery diarrhea (12 patients), and dysentery (11 patients) (Table 1 and Figure 3). Vomiting in PCR-positive patients was associated with fever and watery diarrhea. Also, intractable vomiting and nausea vomiting were common in PCR-negative patients. In PCR-negative patients, vomiting, abdominal pain, and watery diarrhea were the most common symptoms.
Forty-six patients with abdominal pain were referred to the pediatric emergency surgery department of Namazi Hospital, of whom 35 were monitored, and finally, 32 underwent surgery.
The pathology of these 32 patients showed that 21 had appendicitis, of whom 2 had positive PCR tests for SARS-CoV-2. Pathologic evaluation in surgical exploration revealed that 10 patients did not have appendicitis-related pathology (6 patients had normal pathology results and 4 patients had nodular lymph hyperplasia). Four of these 10 patients had positive PCR tests. The only patient left from the non-appendicitis-related pathology group was diagnosed with intussusception, and the patient’s COVID-19 test was also positive.
The study results showed that the distribution of GI findings was significantly different between patients with positive PCR tests for SARS-CoV-2 and patients with negative PCR tests (P < 0.05).
3.3. Investigating Underlying Disease and Positive PCR Test for SARS-CoV-2
In this study, 124 patients had no underlying disease, of whom 40 (32%) had positive PCR tests for SARS-CoV-2. Eight of 33 patients with cirrhosis had positive SARS-CoV-2 RT-PCR tests (24%). Of 9 patients planned for liver transplantation, only 1 (11%) patient had a positive PCR test for SARS-CoV-2 (Table 2).
Five patients had IBD, with 1 (20%) having a positive SARS-CoV-2 RT-PCR test (Table 2).
The prevalence of positive PCR tests for SARS-CoV-2 was not higher in patients with underlying diseases than in those without (P > 0.05).
Due to the financial constraints in this study, it was impossible to do SARS-CoV-2 RT-PCR tests on the stool or anal swab samples for all patients. Therefore, rectal swabs underwent SARS-CoV-2 RT-PCR only for patients with diarrhea. The results revealed that only one case was positive.
3.4. Laboratory Findings
A review of the laboratory findings of the patients showed a difference in the mean lymphocyte count between patients with positive and negative SARS-CoV-2 PCR tests; it was significantly lower in PCR-positive patients (P < 0.05). Besides, inflammatory markers (CRP and ESR) were significantly higher in patients with positive PCR tests (Table 5).
3.5. Radiographic Findings
Radiologic studies like lung high-resolution computed tomography (HRCT) were considered for patients with respiratory symptoms or suspicion of lung involvement and pneumonia. Twenty-two of 57 PCR-positive patients and 57 of 137 PCR-negative patients had HRCT. The most common radiologic finding on chest X-rays was the presence of reticuloendothelial lesions; 10 patients with this finding had positive PCR tests. The most common radiologic finding on lung CT scans of suspected patients was collapse consolidation, which was reported in seven patients, 2 of whom had positive PCR tests for SARS-CoV-2 (Table 3).
3.6. Patients Outcome
The outcome of the studied patients was also examined, showing that 172 of 184 patients were discharged from the hospital. Twelve patients died, 4 of whom had positive PCR tests.
4. Discussion
This article reports the prevalence of positive PCR tests for SARS-CoV-2 in pediatric patients with GI symptoms. The most common GI symptoms in positive PCR test patients were vomiting and diarrhea, inconsistent with other reports (25-28). The GI symptoms of COVID-19 can be the only presentations of the disease or accompany respiratory symptoms. Diarrhea is a prevalent GI symptom and is very important for public health because of the potential for fecal-oral disease transmission (29). Patients can also have nausea and vomiting as their only presentation or concurrent with other GI symptoms (29, 30). Out of 51 patients with positive SARS-COV-19 PCR test, male dominancy was found, similar to other reports (31). Some other studies found no difference in sex ratio (7, 32). In this study, male dominancy was present. In abnormal CT images, collapse consolidation was the most common feature, similar to other studies reporting consolidations as a mark of COVID-19 in radiographic studies (33, 34). Acute abdominal pain or GI tract inflammation with various pathogens (including SARS-CoV-2) may provide a clinical picture that mimics appendicitis in children. Therefore, more specific criteria should be defined in future investigations for accurate differentiation from other potential diagnoses (35).
4.1. Limitations
This study had some limitations that further investigations should address. Our hospital predominantly serves an Iranian community and has a small sample size, so the findings may not be generalizable to other populations. Many patients were discharged from the hospital with personal consent due to fear of COVID-19 before performing necessary examinations or preferred outpatient departments for medication. In the course of the study, a decrease in the number of patients was observed, which may be due to the increase in general knowledge of the population about COVID-19, faster diagnosis, or a decrease in the number of patients referred to the hospital after the second peak of COVID-19 outbreak in Iran. Due to the lack of sufficient knowledge about the criteria for diagnosis of MIS-C in the course of the study, several patients may have been excluded from the study. Due to the shortage of diagnostic and laboratory facilities in the early outbreak of COVID-19 and financial constraints in the study, it was impossible to examine the stool PCR for all patients and other markers related to COVID-19. COVID-19 detection could also be coincidental with other diagnoses or be asymptomatic, which could cause incorrect classification. In addition, the SARS-CoV-2 PCR test could remain positive in some patients with chronic diseases. Therefore, the positivity of the test does not necessarily indicate an acute COVID-19 infection. It means that some of these positive PCR tests may be due to a remote SARS-CoV-2 infection (PCR positivity state).
As mentioned before, our study was designed in late 2019, and MIS-C was first identified in April 2020. Therefore, MIS-C criteria were hard to consider at first. However, after sampling and precisely recording the patient data, we could confirm if any case of MIS-C was included in this study. According to our data and MIS-C criteria, our study had no definite or suspicious case of MIS-C. The readers should consider this issue for further investigation.
4.2. Conclusions
This study aimed to find more about the prevalence of GI symptoms that might mask COVID-19 diagnosis, causing it to be delayed or misdiagnosed as a medical or surgical emergency. In this study, the PCR-positive patients had various GI manifestations. Children with the underlying disease were not at increased risk of COVID-19 infection. Elevated inflammatory markers were seen in those with positive PCR tests. This study showed that COVID-19 still has many unknown aspects, and newer findings should be presented. On the other hand, any unexplained findings may be COVID-19 in patients referred to the hospital. Therefore, according to the pandemic status and the variety of COVID-19 presentations, physicians should consider all symptoms, including GI and hepatic manifestations.