1. Background
Systemic candidiasis is the most common invasive fungal infection in immunocompromised patients. Candida (C) species are endogenous human flora that may act as opportunistic pathogens. The prevalence of infections caused by Candida species in people with immune defects such as patients with malignant tumors, neutropenia, hematologic disorders, and extended hospital stays is increasing (1-3). Candida albicans is a more frequent isolate, but in recent years, the incidence of non-albicans Candida species like Candida krusei, Candida glabrata, Candida kefyr, Candida parapsilosis, and Candida tropicalis has increased significantly (4). The incidence rate of the fungal infection in pediatric patients with hematologic disorders was reported 16.3% and C. albicans was the most prevalent etiologic agent (5). In neonates, Candida colonization was reported in ear, umbilicus, rectum, catheter, and tracheal tube and it is related to the risk of developing a systemic candidiasis (6). A long-term use of antifungal agents can lead to an increase in resistance by specific mechanisms among Candida species (7, 8). The sensitivity patterns of Candida species depend on patient’s previous antifungal therapy and local healthcare management. The objective of the present study was to investigate the distribution of Candida species isolated from urine and blood samples of malignant patients and determine in vitro antifungal susceptibility patterns of the isolates to promote their effective management.
2. Methods
2.1. Sample Collection
This study was a cross-sectional type carried out in the department of infection and tropical diseases research center at Jundishapur University of Medical Sciences, Ahvaz, and professor Alborzi clinical microbiology research center, Shiraz University of Medical Sciences, Shiraz, Iran. It was approved by the ethics committee of Jundishapur University of Medical Sciences. The inclusion criteria were patients with various malignancies hospitalized at Shafa Hospital, a large tertiary care referral hospital, during 2013 - 2014 in Ahvaz with unknown fever. Blood and urine cultures were done at admission. All the patients had a history of previous use of antibacterial agents and admission in the hospital. Three hundred eighty-five (385) patients with malignancies were admitted to Shafa hospital and the clinical samples (240 blood and 285 urines; totally 525 samples) were collected during the hospitalization period (the patients did not have any blood or urinary catheter).
2.2. Mycological Study
The urine samples were cultured on Sabouraud’s Dextrose Agar (Merk, Germany) and blood samples on routine blood culture bottle (monophasic, broth blood culture method) and then transferred to the professor Alborzi clinical microbiology center for the evaluation of the isolated fungi. Demographic data including the type of malignancy, the reason for current hospitalization, age, gender, and the history of antibiotics use were collected using a questionnaire.
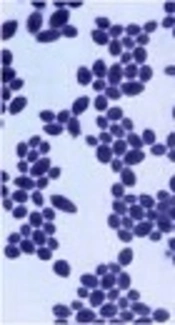
The isolated fungi were cultured twice on potato dextrose agar (Merk, Germany) for 3 - 5 days at 35°C to make sure the purity of the isolates. For species identification, chlamydospore and germ tube production and carbohydrate assimilation patterns (API 20 C AUX system) of all the isolates were investigated according to the manufacturer’s instructions (Biomerieux, France). Candida parapsilosis ATCC 22019 was used as a standard quality control CLSI-recommended strain.
2.3. Antifungal Drugs
Standard antifungal powders of amphotericin B (Sigma-Aldrich, Germany), ketoconazole (Sigma-Aldrich, China), posaconazole (Sigma-Aldrich, Germany), voriconazole (Sigma-Aldrich, USA), fluconazole (Sigma-Aldrich, USA), and itraconazole (Sigma-Aldrich, India) were obtained from their respective manufacturers. The serial concentration of the amphotericin B, itraconazole, posaconazole, and voriconazole was 16 to 0.032 µg/mL, and for fluconazole, it was 64 to 0.125 µg/mL.
2.4. Broth Microdilution Susceptibility Test Method
To determine the susceptibility pattern of the isolates, CLSI document M27-A3 and S4 were used (9, 10). The inoculums suspensions were prepared by the spectrophotometric method at 530 nm. The suspensions were diluted 1:1000 in RPMI 1640 medium (Sigma-Aldrich, United Kingdom) with pH 7.0 by using 0.165 M morpholinepropanesulfonic acid (Sigma-Aldrich, Germany) and adjusted to the final concentration of 1 x 103 to 5 × 103 CFU/mL. An aliquot of 100 µL of concentration was added to each well. The positive and negative controls (Drug-free and yeast-free) wells were included for each species. The trays (microdilution plate) were incubated at 35°C and the minimum inhibition concentration (MIC) after 24 and 48 hours was read visually. The definition of MIC value was the lowest concentration that produced a prominent decrease in turbidity compared to the positive growth control for fluconazole, itraconazole, posaconazole, voriconazole (approximately 50% or 80% reduction in growth). For amphotericin B, the complete inhibition of growth was considered the MIC value. The MIC50 and MIC90 values of the isolated species were calculated (the MIC at which 50% and 90% of the isolates were inhibited). According to the new CLSI (2012), the breakpoints of antifungal agents for some Candida spp. were changed. The susceptibility pattern of each isolate was analyzed according to the new CLSI breakpoints. For amphotericin B, many reports considered MIC ≥ 1 µg/mL as resistant. Clinical breakpoint for fluconazole in C. glabrata is ≤ 32 as susceptible dose-dependent and ≥ 64 as resistant. As for other species, susceptible, susceptible dose-dependent, and resistant are ≤ 2.0, 4.0, and ≥ 8.0, respectively. Interpretive breakpoint criteria have not been defined for ketoconazole and posaconazole and we reported them according to the MIC 90 value of isolates (9, 10).
2.5. Statistical Analysis
Data analysis was performed using SPSS 16.0 and subsequently analyzed using chi-square, t-test, and one-way ANOVA. The level of significance of the above tests was set at < 0.05. Sensitivity related data were analyzed by WHONET 5.6.
3. Results
Three hundred-eighty-five patients were included in this study. The ratio of female to male was 158/227 (41%:59%) with the mean age of 64.3 months (2 - 192 months). Of the patients, 241 (62.6%) had haematological malignancies and 144 (37.4%) had non-haematological malignancies. Fifty-four (11.4%) of the 385 patients had histories of taking antibiotics, while 341 had not taken these drugs (Table 1).
| Total Patients (n = 385) | Without any Isolation (%) | Isolation of Candida | P Value |
|---|---|---|---|
| Sex | 0.089 | ||
| Female (n = 158) | 137 (86.7) | 21 (9.5) | |
| Male (n = 227) | 158 (69.6) | 69 (15.4) | |
| Age, mo | |||
| mean (64.3 mo) | 60.9 | 64.8 | 0.55 |
| Type of malignancy | 0.301 | ||
| Hematologic (n = 241) | 190 (78.8) | 51 (21.2) | |
| Non hematologic (n = 144) | 105 (73) | 39 (27) | |
| History of receiving antibacterial | 0.001 | ||
| Received (n = 44) | 13 (29.6) | 31 (70.4) | |
| Not received (n = 341) | 277 (81.2) | 64 (18.7) |
From 385 patients, 525 clinical samples were collected. From 90 patients (23.4%), 102 Candida species were isolated (60 from urines and 30 from blood). Isolated species were 55 C. albicans, followed by 16 C. tropicalis, 10 C. kefyr, 10 C. parapsilosis, 4 C. famata, 3 C. glabrata, and two isolates of each C. guilliermondii and C. dubliniensis (Table 2). The average age was 60.9 months in the patients with Candida isolates and it was 64.8 months for those with no isolates; there was no significant correlation between age and Candida isolation (P = 0.55, df = 383, t = 0.585). In addition, 15.4% of the boys and 9.5% of the girls, 21.2% of the patients with haematological, and 27% of the patients with non-haematological malignancies were infected with Candida species (Table 1); there was no significant correlation between gender (P = 0.089) and various types of malignancies (P = 0.301) and Candida isolation. Candida species were isolated from 18.7% of the patients with no history of antibacterial use and 70.4% of the patients receiving antibacterial agents, with a statistically significant relationship between isolation and antibacterial use (P = 0.001).
| Candida Species | No. (%) |
|---|---|
| Candida albicans | 55 (54.0) |
| Candida tropicalis | 16 (15.7) |
| Candida parapsilosis | 10 (9.8) |
| Candida kefyr | 10 (9.8) |
| Candida famata | 4 (3.9) |
| Candida guilliermondii | 2 (2.0) |
| Candida dubliniensis | 2 (2.0) |
| Candida glabrata | 3 (2.8) |
| Total | 102 (100.0) |
The most prevalent species was Candida albicans with sensitivity rates of 91%, 96%, 100%, 96%, and 60% to fluconazole, amphotericin B, caspofungin, voriconazole, and itraconazole, respectively. Epidemiological cut-off values for amphotericin B, voriconazole and itraconazole were 0.064 µg/mL, 0.032 µg/mL, and 0.250 µg/mL, respectively. Most of the isolated species were wild-type (without mutational or acquired resistance gene). From all the isolated species, 4% of C. albicans was non-wild type (acquired resistance mutational gene) to amphotericin B and voriconazole and 6% to itraconazole. Itraconazole intermediate and resistance rates were 34% and 6%, respectively. There were no breakpoints in CLSI for posaconazole and ketoconazole. The MIC90 values for posaconazole and ketoconazole were 0.032 and 0.064, respectively. Comparing the MIC90 for all the strains, the lowest was observed for caspofungin (0.032 µg/ml). The susceptibility pattern and MIC for each isolate and MIC50 and MIC90 of all isolated Candida species are shown in Table 3.
| Isolate | Antifungal | Sensitive% (Wild Type) | Intermediate% | Resist% (Non-Wild Type) | MIC50 | MIC90 | Range |
|---|---|---|---|---|---|---|---|
| Candida albicans (55) | Amphotericin B | 96 | 0 | 4 | 0.032 | 0.064 | 0.032 - 16 |
| Caspofungin | 100 | 0 | 0 | 0.032 | 0.032 | 0.032 - 0.032 | |
| Voriconazole | 96 | 4 | 0 | 0.032 | 1 | 0.032 - 2 | |
| Fluconazole | 91 | 5 | 4 | 0.125 | 2 | 0.064 - 2 | |
| Posaconazoleb | - | - | - | 0.032 | 0.032 | 0.032 - 0.064 | |
| Itraconazole | 60 | 34 | 6 | 0.064 | 0.5 | 0.032 - 1 | |
| Ketoconazoleb | - | - | - | 0.032 | 0.064 | 0.032 - 0.125 | |
| Candida tropicalis (16) | Amphotericin B | 100 | 0 | 0 | 0.032 | 0.064 | 0.032 - 0.064 |
| Caspofungin | 100 | 0 | 0 | 0.032 | 0.064 | 0.032 - 0.064 | |
| Voriconazole | 97.5 | 0 | 2.5 | 0.032 | 1 | 0.032 - 1 | |
| Fluconazole | 90 | 0 | 0 | 0.125 | 2 | 0.064 - 2 | |
| Posaconazoleb | 0 | 0 | 0 | 0.032 | 0.032 | 0.032 - 0.032 | |
| Itraconazole | 60 | 30 | 10 | 0.032 | 0.5 | 0.032 - 0.5 | |
| Ketoconazoleb | 0 | 0 | 0 | 0.032 | 0.032 | 0.032 - 0.032 | |
| Candida parapsilosis (10) | Amphotericin B | 100 | 0 | 0 | 0.032 | 0.032 | 0.032 - 0.032 |
| Caspofungin | 100 | 0 | 0 | 0.5 | 1 | 0.032 - 1 | |
| Voriconazole | 100 | 0 | 0 | 0.032 | 0.032 | 0.032 - 0.032 | |
| Fluconazole | 100 | 0 | 0 | 0.25 | 0.5 | 0.125 - 0.5 | |
| Posaconazoleb | - | - | - | 0.032 | 0.032 | 0.032 - 0.032 | |
| Itraconazole | 100 | 0 | 0 | 0.032 | 0.0125 | 0.032 - 0.125 | |
| Ketoconazoleb | - | - | - | 0.032 | 0.032 | 0.032 - 0.032 | |
| Candida kefyr (10) | Amphotericin B | 100 | 0.0 | 0 | 0.032 | 0.064 | 0.032 - 0.064 |
| Caspofungin | 100 | 0 | 0 | 0.032 | 0.032 | 0.032 - 0.032 | |
| Voriconazole | 100 | 0 | 0 | 0.032 | 0.064 | 0.032 - 0.064 | |
| Fluconazole | 100 | 0 | 0 | 0.032 | 0.125 | 0.064 - 0.125 | |
| Posaconazoleb | - | - | - | 0.064 | 0.032 | 0.032 - 0.032 | |
| Itraconazole | 50 | 50 | 0 | 0.032 | 0.5 | 0.064 - 0.5 | |
| Ketoconazoleb | - | - | - | 0.032 | 0.032 | 0.032 - 0.032 |
aBreakpoints are according to the new CLSI (S4, Reference 8).
bThere was no breakpoint for this antifungal agent according to the new CLSI.
4. Discussion
Isolation of Candida from blood samples may be due to the transient passing of yeasts or true systemic infections, and isolation of yeast from urine can be explained by systemic candidiasis or colonization of Candida in the urinary tract. Colonization in urine samples was defined as the isolation of a Candida species from the urinary tract without any symptom of urinary tract infection. The symptomatic urinary Candida infections are indistinguishable from bacterial infections and they are presented with oliguria, cystitis, strangiuria dysuria, urgency, flank pain, and rarely fever (11).
Given similar clinical and radiologic signs and symptoms of infections in this population, unfortunately, differentiation between colonization and transient candidemia and pathogenic condition was difficult; therefore, we report the rates of Candida isolation. In recent years, infections caused by Candida species, particularly in immunodeficient patients, have increased considerably. Malignancy is one of the most common underlying conditions for fungal infections. In this study, 90/385 patients (23.4%) had Candida species in urine and blood samples. The rate of Candida colonization from nose, oropharynx, stool, and urine of hematologic paediatric patients was reported 54% (12). No relationship was seen between Candida isolation and sex, age, and type of malignancy; but a significant relationship was between the use of antibacterial agents and Candida isolation. Borges et al. reported the history of receiving antibiotics increased 15 folds the chance of Candida colonization (1). Cornistein et al. revealed that the history of receiving antibiotics increased the probability of Candida colonization (13). In contrast, Issa et al. reported no relationship between antibiotics use and extent of infections with Candida species (14). The difference in findings may be due to the length of the treatment period and the types of antibiotics taken.
Candida albicans was the most prevalent species isolated from the samples in our study, which is consistent with other studies (1, 15-17). In this study, the rates of non-Candida albicans were C. tropicalis 16 (15.7%), C. parapsilosis 9.8%, C. kefyr 9.8%, C. famata 3.9%, and C. dubliniensis 2%. In another study, C. tropicalis 3.9%, C. parapsilosis 4.9%, C. dubliniensis 1.5%, and no C. kefyr were reported (18). Another study revealed the rates of non-albicans Candida were C. krusei (14%), C. tropicalis (16%), and C. glabrata (24%) (19). The existing differences in the distributions may be due to differences in the places where the studies were conducted.
In the present study, no resistant species like C. krusei and only 3 C. glabrata were isolated; and other isolated Candida species were sensitive to all antifungal agents except itraconazole. Azole resistance was more common in non-albicans Candida species, compared to C. albicans. The MIC90 values for posaconazole and ketoconazole were 0.032 and 0.064 µg/mL, respectively. Differences between the sensitivity patterns of antifungal agents may be explained by their availability in each region. In studies carried out by some researchers, most Candida species were resistant to itraconazole (20-22). Cross-resistance between azole antifungals was reported and resistance to itraconazole could increase the MIC of each of fungi to azole antifungals. Long-term itraconazole prophylaxis is associated with a decline in its susceptibility pattern. Itraconazole resistance has become a growing concern in our region. However, in Da Costa et al. study in Brazil in 2014, the sensitivity to itraconazole was reported 100% in 108 patients (16). In addition, in this study, the sensitivity patterns to the antifungal medicines were 91%, 98%, and 99%, to fluconazole, voriconazole, and amphotericin B, respectively (16). Issa et al. conducted a research in 2011 among 492 immunodeficient children and found all Candida spp. were sensitive to amphotericin B and caspofungin, and 97% of species were sensitive to fluconazole (14). These differences may be due to the type of the healthcare and management in patients in each region.
According to the recommendation for the management of candidiasis, neutropenic and non-neutropenic patients should be treated for candidemia. The retinal examination should be performed by an ophthalmologist in these patients. Blood cultures should be performed routinely and the duration of the therapy is 2 weeks after clearance of etiologic agent from the bloodstream (23). In neonates with the isolation of Candida species from blood or urine, a lumbar puncture and a dilated retinal examination are strongly recommended (23).
When Candida species are isolated from urine, imaging by ultrasound or CT scanning from urinary tract is helpful in the diagnosis of structural abnormalities, abscesses, obstruction in the kidney or bladder by fungus ball, emphysematous and pyelonephritis (24-27).
For the treatment of Candida urinary tract infections, the presence of enough concentration of the antifungal agent in the target organ and the knowledge of antifungal susceptibility patterns of the etiologic agents are very critical (24). Fluconazole, flucytosine, and amphotericin B deoxycholate demonstrate good activities in the treatment of urinary tract infections due to C.albicans because their concentrations in the urine are high. The use of such antifungal agents for the treatment of infections caused by C. glabrata and C. krusei, which are extremely difficult to treat, is not effective enough (24-27).
Based on our obtained results, the most prevalent species isolated from the clinical blood and urine samples of patients was C. albicans, with almost highest sensitivity to routine antifungal agents like fluconazole and amphotericin B. Furthermore, the isolates were sensitive to caspofungin, voriconazole, and ketoconazole and the most resistant was to itraconazole.
4.1. Conclusions
Mutations in drug sensitivity were found in some species (non-wild type). As there was a relationship between the use of antibacterial agents and isolation of Candida species from immunocompromised patients, accurate diagnosis of Candida species isolated, along with knowledge of antifungal susceptibility patterns in different geographical zones, are needed for the management of the affected population.