1. Introduction
The severe acute respiratory syndrome Coronavirus 2 (SARS-CoV-2) can present as either asymptomatic or mildly symptomatic in children, with symptoms of fever, dry cough, and fatigue (1).
Multisystem inflammatory syndrome in children (MIS-C) is a hyperinflammatory condition that occurs 2 - 6 weeks after a COVID-19 infection as a fatal complication. This condition is similar to Kawasaki disease (KD) and toxic shock syndrome (TSS) in children, (2) though recently, it was named COVID-MIS-C (3). This similarity, especially with KD, has prompted scientists to give it names, such as Kawasaki-like disease, atypical KD, SARS-CoV-2-induced Kawasaki-like hyper-inflammatory syndrome (SCiKH Syndrome), and Kawa-COVID-19 (2). MIS-C presents in older children with gastrointestinal (GI) complaints, shock, and coagulopathy, while KD presents in children under the age of five, with these presentations rarely associated with it (4). The main symptoms of MIS-C are fever (lasting more than 24 hours), severe illness requiring hospitalization, rash, conjunctivitis, hypotension or shock, multiorgan involvement (affecting more than two organs), acute GI symptoms, abdominal pain, and coagulopathy, with a special emphasis on recent positive COVID-19 test results. Neurologic and respiratory symptoms have not been reported as much (5), but they are not rare enough to be excluded entirely.
Thrombotic events following COVID-19 infection are mostly described in ill adults (6), and rarely occur in children (7). Thrombotic events present as pulmonary embolism (PE), deep vein thrombosis (DVT), thrombotic microangiopathy, and arterial thrombotic events, such as strokes (8). If such an event is associated with COVID-19, it is called COVID-19-associated coagulopathy (CAC) (6). The evaluation of a thrombotic event is best done with lab measurement of serum D-Dimer, which suggests endothelial cell dysfunction, confirming the thrombotic event. The mainstay of treatment is anticoagulant therapy. In adults, the use of thromboprophylaxis reduces hospital mortality, but in the pediatric population, there is a lack of evidence to provide an exact directive to do so (7).
Thromboembolic events, such as DVTs and PEs in children, can occur for various reasons, which can be divided into hereditary and acquired causes. Hereditary causes include defects within the coagulation factors and inhibitors of hemostasis, both of which have unknown causes, the malfunction of which can lead to hypercoagulable states. Some metabolic conditions have been theorized to contribute to this matter, yet they require further studies to be fully confirmed. Of the acquired causes, the use of central venous catheters, childhood cancers, thrombosis, and antiphospholipid syndrome, as well as Heparin-induced thrombocytopenia type 2, are some of the well-known culprits (9). In recent years, COVID-19 has been added as one of the causes of thrombotic events in children, with new information being added every day.
The diagnostic process involves a clinical evaluation of the symptoms and an accurate history of positive COVID-19 tests. Laboratory studies assess inflammatory biomarkers, such as C-reactive protein, erythrocyte sedimentation rate, ferritin, pro-calcitonin, interleukin-6 (IL-6), and fibrinogen. Elevated D-dimer levels and neutrophils, as well as reduced lymphocytes and albumin, help in narrowing down the diagnosis (5).
Treatment includes corticosteroids, IL-6 inhibitors, and intravenous immunoglobulins (IVIG), as well as management of other conditions (i.e., vasopressors and inotropes for cardiac issues, mechanical ventilation in respiratory distress, etc.) (10).
In this article, we presented the vignette of a nine-year-old boy with lower limb edema due to bilateral DVTs following COVID-19 infection.
2. Case Presentation
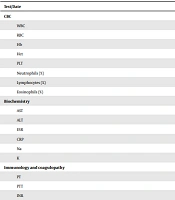
The patient was a nine-year-old boy who was admitted to the specialized hospital after being transferred from the city general hospital. His symptoms started two weeks earlier and were as follows: fever, malaise, and myalgias. He was initially visited as an out-patient in a clinic, during which he was prescribed acetaminophen and cefixime, after which he not only did not get better but developed lower limb edema and headaches too. Both these conditions were the chief complaints on admission to the general hospital a week earlier. During this time, he underwent a series of procedures as follows: a Doppler sonography, which revealed acute DVTs in the Iliac and femoral veins bilaterally, a brain MRI showing transverse sinus thrombosis, and an RT-PCR test for COVID-19, which came out positive. The patient was given remdesivir and methylprednisolone (1 mg/kg/dose) every 12 hours and enoxaparin (1 mg/kg) every 12 hours for five days prior to his transmission to the specialized hospital. Upon admission, the patient had a thorough physical examination, in which we ruled out the presence of meningeal irritation. The abdominal exam was unremarkable, and we confirmed the presence of lower limb edema. His vital signs were as follows: blood pressure (BP) = 110/60 mmHg, heart rate (HR) = 98 bpm, temperature = 37.2°C, and respiration rate (RR) = 18 bpm. Upon his entry, we asked for any significant family histories or past medical histories related to his current presentation. His family history was negative for any genetic diseases and stroke events in family members under 40 years of age. Laboratory studies were ordered routinely throughout his stay at the hospital. For convenience, we included the MIS-C and COVID-19-related test results from admission to discharge in the specialized hospital in Table 1.
| Test/Date | Admission | Discharge |
|---|---|---|
| CBC | ||
| WBC | 5.3 | 2.6 |
| RBC | 2.96 | 2.92 |
| Hb | 8.6 | 8.8 |
| Hct | 27.1 | 28 |
| PLT | 91.9 | 201 |
| Neutrophils (%) | 36 | 40 |
| Lymphocytes (%) | 60 | 51.4 |
| Eosinophils (%) | 2 | 1 |
| Biochemistry | ||
| AST | 230 | 35 |
| ALT | 276 | 84 |
| ESR | 97 | 40 |
| CRP | 53 | 12 |
| Na | 136 | 137 |
| K | 4.0 | 4.1 |
| Immunology and coagulopathy | ||
| PT | 13.9 | 12.0 |
| PTT | 40 | 33 |
| INR | 1.26 | 1.0 |
| D-Dimer | 450 | 14.8 |
| ASMA (I.F) | Negative | Negative |
| APCR | 191 | - |
| SARS-CoV-2 anti-spike (IgG) | > 100 | - |
aFor convenience, we have only reported the test results related to MIS-C and COVID-19, despite the fact that there were many more tests done at regular intervals to follow the progression of the condition.
During his stay in the specialized hospital, several tests were performed, and their results were as follows: the MRV revealed transverse sinus thrombosis, the chest CT scan and echocardiography were normal, and a repeat of his Doppler sonography confirmed the previous bilateral DVT finding in the same location. At this point, we established a diagnosis of MIS-C and continued his enoxaparin at 1 mg/kg/dose every 12 hours and methylprednisolone (1 mg/kg) every 12 hours. He was given enoxaparin for his DVTs, the toxic levels of which were tracked via anti-Xa assays (0.75). Then, hematology and neurology consultations with lab studies were made to ensure the exclusion of other possibilities. The following lab studies were done for the patient: presence of prothrombin G20210A, anticardiolipin antibodies (IgM and IgG), perinuclear antineutrophil cytoplasmic antibodies (P-ANCA), antineutrophil cytoplasmic antibodies (C-ANCA), pro-B-type natriuretic peptide (BNP), protein C, protein S, and activated protein C resistance (APCR for factor V Leiden), fibrinogen, anti-thrombin activity, anti-thrombin III, human leukocytic antigen (HLA) B51, HLA-B52, Ceruloplasmin, and homocysteine levels, and all were negative.
The patient responded well to the MIS-C treatment. He was in the hospital for 14 days. On discharge, the patient was fine; his edema and headaches had subsided entirely. At his scheduled follow-up, the patient returned for an ultrasound, which showed normal blood flow in his superficial and deep popliteal veins on the right side and signs of recanalization with slight echogenic content and normal vein diameter on the left. Upon discharge, he was given corticosteroids to continue at home with plans to be gradually tapered off. A week later, the patient’s enoxaparin was changed to the 10 mg oral form, one pill in the morning and half of a pill at night, to which the patient responded really well in subsequent follow-ups. Two weeks after his discharge, his follow-up tests were done, and the results are provided in Table 2. Three weeks after discharge, methylprednisolone was discontinued. A month after discharge, he had another Doppler ultrasound of his popliteal and iliac vessels as part of his follow-up routine, which was completely normal. On his last follow-up visit, the patient was told to gradually taper off the enoxaparin pills, and the dosage was reduced to one pill every morning with instructions to taper off within three weeks, reducing by 1/3 of a pill every week. Future follow-up visits are scheduled to evaluate his improvement.
| Tests | Result |
|---|---|
| Biochemistry | |
| BUN | 31 |
| Creatinine | 0.65 |
| Total Bilirubin | 0.6 |
| Direct Bilirubin | 0.2 |
| AST | 21 |
| ALT | 40 |
| Alk.P | 294 |
| LDH | 825 |
| Hematology | |
| WBC | 5.6 |
| RBC | 3.5 |
| Hemoglobin | 11.3 |
| Hematocrit | 33.2 |
| MCV | 95 |
| MCH | 32.3 |
| MCHC | 34.0 |
| RDW | 18.9 |
| Platelet Count | 235 |
| Anisocytosis | (+) |
| Coagulation Test | |
| D-dimer (E.C.L) | 0.8 |
| FDP | 4.0 |
3. Discussion
In this section, we discussed the variety of presentations of MIS-C following COVID-19, with an emphasis on the thromboembolic events associated with it.
The diagnostic criteria for MIS-C following COVID-19 are quite different between resources. Still, the Centers for Disease Control and Prevention (CDC) has provided well-detailed criteria, which make the process much easier. However, neither of the existing criteria accounts for different presentations of MIS-C, especially those presenting with thrombotic events, such as our case. While the American College of Rheumatology provides a dedicated algorithm for the diagnosis of MIS-C, which includes anticoagulation therapies, (6) the Iranian national guideline of COVID-19 management in pediatrics suggests that any patients with presentations similar to ours should have all their laboratory markers evaluated. These include complete blood count (CBC), inflammatory markers (C-reactive protein (CRP) and erythrocyte sedimentation rate [ESR]), hepatic and coagulation markers, renal function, chest X-ray (CXR), electrocardiogram (ECG), echocardiography, and COVID-19 PCR. The guideline suggests that comorbidities like shock, severe heart failure, central nervous system (CNS) dysfunction, and respiratory distress should all be ruled out (11).
The risk of thrombotic events in hospitalized children following COVID-19 or MIS-C was studied by Whitworth et al. in 2021. Organizing their patients into three groups of asymptomatic with SARS-CoV-2, COVID-19 infection, and MIS-C following COVID-19, they showed that the risk of thrombotic events is much higher in children with MIS-C, followed by COVID-19 and SARS-CoV-2. They also showed that the risk factors for such events in children include older age, cancer, central venous catheter, and MIS-C, as well as expressing a high mortality rate of 28% in children and adolescents who experience a thrombotic event following MIS-C or COVID-19 (12). Thrombotic events have been reported with a variety of presentations following COVID-19, including kidney infarctions leading to acute kidney injury (13), cerebral venous thrombosis in a 41-year-old (14), pulmonary embolism (15), hepatic artery thrombosis (16), etc.
3.1. Conclusions
In conclusion, thrombosis following MIS-C is an unlikely but deadly event; thus, physicians should always be on alert to promptly find and treat such occasions. Treatment includes corticosteroids, anticoagulation therapies (with heparin), and symptomatic management of the condition. Monitoring patients during treatment for any changes, including the development of new symptoms as well as the toxic levels of the medications, is strongly recommended.