1. Background
In 2000, the American Academy of Pediatrics (APP) introduced the International Pediatric Prehospital Program (PEPP), which was the result of more than 10 years of work by several experienced pediatric emergency physicians and the emergency medical care (EMS) in 2005 as a rapid assessment tool (pediatric assessment triangle [PAT]) introduced (1). A single, standard terminology and evaluation and treatment algorithm based on clinical experience in pediatric emergency and critical care were developed. They used this tool in pediatric emergency training courses, such as Advanced Pediatric Life Support (APLS), Emergency Nursing Pediatric Course (ENPC), and Ambulatory Pediatric Care (APC) (2-5). The emergency assessment of the patient in critical situations is often complex. Vital signs vary according to the patient’s age, and the clinical decision should be further investigated so that the examiner makes fewer mistakes in dealing with the child in critical situations and stressful emergencies and during quick decisions. A reliable and easy algorithm for immediate evaluation and intervention is needed in this situation. There are several scoring systems to examine the outcome of injury; however, limited studies have been conducted on its validity (6-9).
In recent years, PAT has been standardized as a tool in the initial assessment of infants and children for all levels of care (i.e., EMS, nurse, and emergency) (1). The instrument is used visually and audibly without needing touch or examination equipment and for about 30 seconds without causing anxiety, resulting in stable or unstable determination. This tool determines the severity of the disease, the urgency of the treatment intervention, the underlying physiopathology, and the general impression. The value of PAT in rapid assessment of a child without touch is visual and auditory and, therefore, does not cause anxiety for the child and determines how the operation is prioritized in other stages of assessment. In this assessment, the child is divided into four groups in terms of general condition, and finally, according to the mechanism of involvement, immediate action is taken (10, 11).
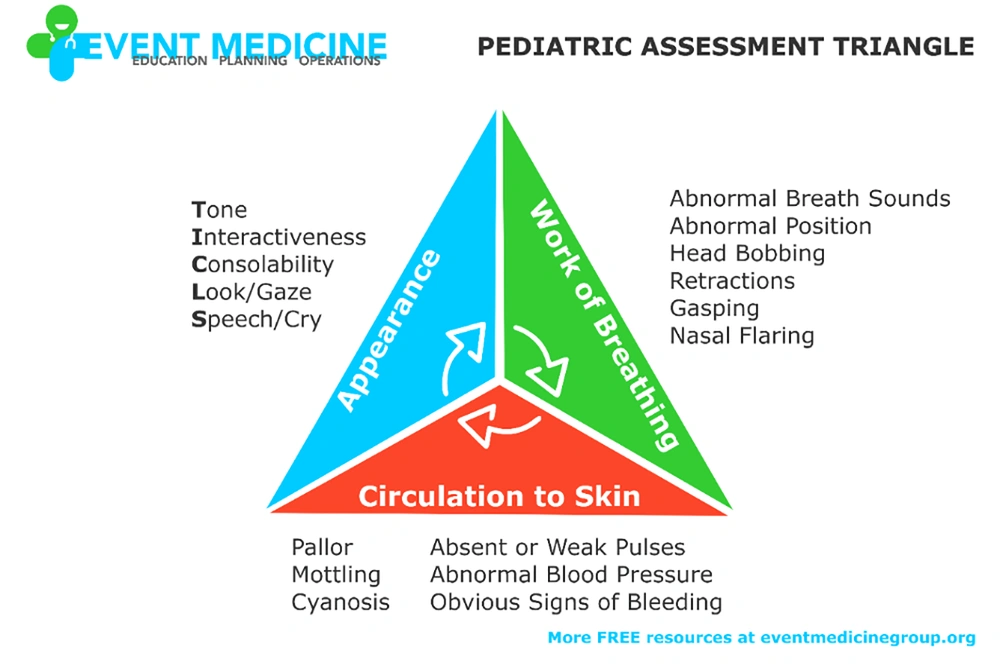
Figure 1 shows the PAT and its main components. The PAT falls into the physiological and general impression categories according to the assessments and answers to the following three main questions:
What is the most probable physiological disorder?
How severe are the child’s injury and illness?
Pediatric assessment triangle (PAT), so far and according to the documents in the world, three research samples have been conducted: One study by Fernandez in Spanish pediatric emergency, one study by Panigua in Africa as a criterion for asthma hospitalization, and one study for transmission and therapeutic interventions at the prehospital level in the United States with the PAT criterion. In all cases, it has a significant relationship with the aforementioned goals. Therefore, it was decided to conduct a sample of this study in Iran with PAT criteria for hospitalization in specialized pediatric emergencies. Due to the similarity to Fernandez’s study, the method was analyzed, and the results were extracted from that study; accordingly, the current similar study was performed. The results have been reasonable.
How fast and urgent should we act? What general and specific treatment should we do? (12).
A study in 2014 by Gausche-Hill et al. (13, 14) was conducted on children up to 14 years of age in California, the United States, in the form of a web observational study on 1168 patients, which finally had a high agreement between the prehospital paramedic measures and the algorithm of the impression of PAT diagnosis. Fernandez et al.’s study in 2017 (15) titled “Examining the Similarity of PAT as the First Step in the Triage Process of Pediatric Emergency Department” was conducted on 302,103 individuals. Finally, abnormal PAT had a high risk of hospitalization and was a useful tool to determine the severity of the disease. More than one abnormal criterion and appearance were most significantly associated with hospitalization. Paniagua et al.’s study in 2017 (16) evaluated PAT as a primary tool in determining the severity of asthma as a predictor for hospitalization, and this relationship was observed to be non-dependent.
The PAT is an easy, simple, and practical tool without intervention and cost-effective to be used at the bedside, which is used to establish an efficient system as a primary tool in the evaluation of children referred to the pediatric emergency room and to prevent confusion between patients and referrals. Furthermore, it reduces the cost to the family and improves the outcome of illness, complications, and mortality. It defines the severity of the injury and the urgency of the treatment, and according to previous studies, its use has well-expressed unstable cases requiring hospitalization.
2. Objectives
The objective of this study was to evaluate the effectiveness of the PAT as the initial step in the triage process in a pediatric emergency room.
3. Methods
In 2021, all children aged 0-14 years who were referred to the Emergency Department of Mofidhospital in Tehran, Iran, underwent an initial evaluation by a physician and a pediatric resident. The evaluation was based on three criteria known as the PAT, which included assessing skin circulation, respiration, and appearance. Any impairments in these criteria were recorded on an information form.
Upon arrival at the emergency department, the patients were evaluated using the PAT criteria by a doctor or resident, and any impaired criteria were marked on the questionnaire. Based on the evaluation results, the patients were either admitted to the emergency room, transferred directly to specific departments, or required resuscitation in the emergency department before being transferred to the pediatric intensive care unit (PICU) under the care of the emergency department or ward. The questionnaire documented the transition of each patient to the respective parts mentioned above. The patients who did not show impairments in any of the PAT criteria were categorized as “Normal” on the questionnaire but could still be hospitalized.
The objective of the study was to compare cases that were hospitalized with impaired PAT criteria in each component (i.e., blood circulation, respiration, and appearance) to cases that were hospitalized despite not having impaired PAT criteria. The cases with impaired PAT criteria were considered significant for the research. These variables were deemed important for patient outcomes, and the PAT criteria encompassed all three of these variables.
Two outcomes were examined in the study: (1) The extent of hospitalization and (2) the extent of hospitalization in the PICU under emergency supervision, along with conducting blood tests. The demographic data of patients, including age and gender, PAT assessment, hospitalization or discharge status, and the assigned ward, were recorded in the information forms.
Logistic regression analysis was used to examine the relationship between variables, both in univariate and multivariate forms. A significance level of 0.05 (95% confidence interval [CI]) was considered, and the analysis was conducted using STATA 16 software. The sampling method employed was non-random, continuous, and based on availability.
The data collection tool used was the researcher information form, which was completed through observation. After filling out the information form, the final outcome (hospitalization) and the type of ward were extracted from the clinical files.
4. Results
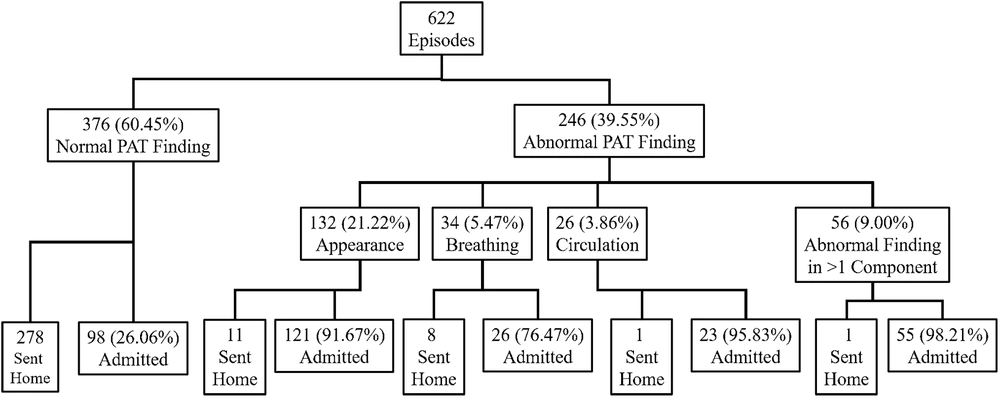
During the 4-month study period, 622 patients referred to the Pediatric Emergency Department of Mofidteaching Hospital were studied. According to statistical data, the mean age of patients was 54.8 months. The age range of the clients was from 0.1 to 204 months. (Table 1) At the initial assessment in the pediatric emergency department, the number of abnormal PAT cases was 246 (39.55%). The highest number of referrals was related to the appearance component, and more than one defective criterion was the case of impaired PAT. The cases of laboratory tests were 467 subjects (75.00%), and 323 cases (51.92%) were hospitalized. Only 26.06% of patients were admitted with normal PAT. Compared to the hospitalization of patients with impaired patency, which was 91.46% in total, there were more cases of hospitalization with impaired patency, which was statistically significant (P ≤0.05). Figure 2 shows the classification chart of patients according to PAT findings.
| PAT Finding | Blood Tests | Hospitalization | Admission to the PICU | Under Emergency Supervision |
|---|---|---|---|---|
| Normal | 231 (61.43) | 98 (26.06) | 1 (0.27) | 42 (11.17) |
| Appearance | 129 (97.73) | 121 (91.67) | 1 (0.76) | 43 (32.58) |
| Work of breathing | 29 (85.29) | 26 (76.47) | 3 (8.82) | 9 (26.57) |
| Circulation to the skin | 24 (100) | 23 (95.83) | 1 (4.17) | 6 (25.00) |
| Abnormal findin gsin >1 component | 54 (96.43) | 55 (98.21) | 28 (50.00) | 2 (3.57) |
Abbreviations: PAT, pediatric assessment triangle; PICU, pediatric intensive care unit.
a Values are expressed as No. (%).
4.1. Results of Univariate and Multivariate Analyses of Hospitalization
Regarding the initial outcome performed by univariate analysis, Table 2 shows the univariate analysis of PAT efficacy in a hospital setting. In the analysis of each component of the PAT triangle, more than one abnormal criterion was more likely to be associated with hospitalization (OR = 61.16, 95% CI: 8.41 - 444.97). This correlation was strong for circulation (OR = 22.85, 95% CI: 3.06 - 170.25) and the appearance of the patient (OR = 15.68, 95% CI: 8.24 - 29.82). Respiration was then ranked as the last (OR = 3.18, 95% CI: 1.41 - 7.14). Normal PAT (OR = 0.03, 95% CI: 0.02 - 0.05) was inversely related to hospitalization. Total PAT criteria were also strongly associated with hospitalization with OR = 33.03 and P ≤ 0.05.
| PAT Finding | Univariate | Multivariate | ||
|---|---|---|---|---|
| OR (95% CI) | P-Value | OR (95% CI) | P-Value | |
| Normal | 0.03 (0.02 - 0.05) | 0.000 | - | - |
| Appearance | 15.68 (8.24 - 29.82) | 0.000 | 31.20 (16.15 - 60.30) | 0.000 |
| Work of breathing | 3.18 (1.41 - 7.14) | 0.005 | 9.22 (4.04 - 21.04) | 0.000 |
| Circulation to the skin | 22.84 (3.06 - 170.25) | 0.002 | 65.24 (8.70 - 489.54) | 0.000 |
| Abnormal findings in >1 component | 61.16 (8.41 - 444.97) | 0.000 | 151.02 (21.30 - 1142.57) | 0.000 |
Abbreviations: PAT, pediatric assessment triangle; OR, odds ratio; CI, confidence interval.
Table 2 shows the multivariate analysis for abnormal findings in each component of the PAT with hospitalization. In multivariate analysis, more than one normal criterion with OR = 151.02 and 95% CI (21.30 - 1142.57) was more significantly associated with hospitalization. Then, blood circulation and appearance had a more significantrelationship with hospitalization.
4.2. Results of Univariate and Multivariate Analyses of Secondary Outcome
The results of univariate and multivariate analyses to evaluate the efficiency of the PAT in emergency hospitalization, hospitalization in the PICU, and blood tests are presented in Table 2, respectively.
Table 3 shows the results of univariate and multivariate analyses of PAT performance in the hospital under emergency supervision. Under emergency supervision, appearance analysis with OR = 3.53 and 95% CI (2.24 - 5.56) had a significant relationship with emergency hospitalization. More than one abnormal criterion with OR = 0.17 and 95% CI (0.04 - 0.72) and normal PAT with OR = 0.39 and 95% CI (0.25 - 0.60) were inversely related to emergency hospitalization. In multivariate analysis under emergency supervision, appearance with OR = 3.84 and 95% CI (2.37 - 6.24) and then breathing and then blood circulation had a significant relationship with hospitalization.
| PAT Finding | Univariate | Multivariate | ||
|---|---|---|---|---|
| OR (95% CI) | P-Value | OR (95% CI) | P-Value | |
| Normal | 0.39 (0.25 - 0.60) | 0.000 | - | - |
| Appearance | 3.53 (2.24 - 5.56) | 0.000 | 3.84 (2.34 - 6.24) | 0.000 |
| Work of breathing | 1.92 (0.87 - 4.24) | 0.108 | 2.86 (1.25 - 6.54) | 0.013 |
| Circulation to the skin | 1.74 (0.67 - 4.50) | 0.251 | 2.65 (1.00 - 7.05) | 0.051 |
| Abnormal findings in >1 component | 0.17 (0.04 - 0.72) | 0.016 | 0.29 (0.07 - 1.25) | 0.098 |
Abbreviations: PAT, pediatric assessment triangle; OR, odds ratio; CI, confidence interval.
Table 4 shows the results of univariate and multivariate analyses of the PAT in the PICU of the hospital. For hospitalization in the PICU, more than one criterion with OR = 93.33 and 95% CI (35.74 - 243.74) had a more significantrelationship with hospitalization in the PICU. Appearance with OR = 0.11 and 95% CI (0.01 - 0.78) and normal PAT with OR = 0.02 and 95% CI (0.00 - 0.13) were inversely related to PICU hospitalization. In the PICU, more than one disrupted criterion with OR = 375.00 and 95% CI (49.19 - 2858.94) was most significantly associated with hospitalization, followed by respiration, and then circulation was more significantly associated with hospitalization.
| PAT Finding | Univariate | Multivariate | ||
|---|---|---|---|---|
| OR (95% CI) | P-Value | OR (95% CI) | P-Value | |
| Normal | 0.02 (0.00 - 0.13) | 0.000 | - | - |
| Appearance | 0.10 (0.01 - 0.78) | 0.028 | 2.86 (0.18 - 46.09) | 0.458 |
| Work of breathing | 1.74 (0.50 - 6.00) | 0.382 | 36.29 (3.67 - 359.30) | 0.002 |
| Circulation to the skin | 0.74 (0.10 - 5.68) | 0.776 | 16.30 (0.99 - 269.09) | 0.051 |
| Abnormal findingsin >1 component | 93.33 (35.74 - 243.74) | 0.000 | 375.00 (49.19 - 2858.94) | 0.000 |
Abbreviations: PAT, pediatric assessment triangle; OR, odds ratio; CI, confidence interval.
Table 5 shows the results of the analysis conducted on the PAT in blood testing, comparing the outcomes of univariate and multivariate approaches. Regarding the blood test in the appearance component with OR = 19.34 and 95% CI (6.06 - 61.72) and more than one defective criterion with OR = 10.00 and 95% CI (2.41 - 41.52) had a significant relationship with hospitalization. In the case of multivariate analysis, the correlation with the appearance component with OR = 26.99 and 95% CI (8.43 - 86.39) and more than one abnormal finding and then breathing had a significant relationship with a blood test. Circulation was not significantly associated with blood tests.
| PAT Finding | Univariate | Multivariate | ||
|---|---|---|---|---|
| OR (95% CI) | P-Value | OR (95% CI) | P-Value | |
| Normal | 0.07 (0.03 - 0.13) | 0.000 | - | - |
| Appearance | 19.34 (6.06 - 61.72) | 0.000 | 26.99 (8.43 - 86.39) | 0.000 |
| Work of breathing | 1.99 (0.76 - 5.22) | 0.184 | 3.64 (1.38 - 9.62) | 0.009 |
| Circulation to the skin | 1.00 (-) | - | 1.00 (-) | - |
| Abnormal findingsin >1 component | 10.00 (2.41 - 41.52) | 0.002 | 16.95 (4.07 - 70.58) | 0.000 |
Abbreviations: PAT, pediatric assessment triangle; OR, odds ratio; CI, confidence interval.
In the PICU, having more than one disrupted criterion showed the strongest association with hospitalization. When patients were under emergency supervision, their general appearance was observed to be highly associated with hospitalization. In terms of blood tests, abnormalities in appearance and having more than one disrupted criterion were most closely linked to hospitalization. Having a normal PAT did not have any significant effect on hospitalization, whether it was in the PICU, during emergency monitoring, or in blood testing. However, there was a statistically significant difference in hospitalization rates between cases where the PAT was disrupted and cases where it was normal.
5. Discussion
The findings of this study indicate that PAT has the potential to serve as a valuable tool for pediatricians in assessing the need for hospitalization in patients. The study revealed that patients with impaired PAT were at a higher risk of requiring hospitalization. Notably, the study was conducted in a teaching hospital by well-trained residents during their introductory courses, and it demonstrated a significant association between the utilization of the PAT by pediatric residents and the likelihood of hospitalization.
The PAT was initially used in prehospital use and is useful for determining patient transfer. Later, its use began in hospitals. In a 2013 study by Horeczko et al. (17), PAT employment by a nurse showed that high specificity identified unstable cases. This ability of the PAT to determine serious problems helped predict the patient’s subsequent condition, such as hospitalization. In Fernandez et al.’s study (15), the PAT was an independent criterion for hospitalization, and the criterion of abnormal appearance and more than one abnormal criterion of the PAT introduced strong criteria for hospitalization even after adjusting for age. The PAT was a useful tool for determining the severity of the disease. The significance of the PAT indicated the need to use it in the first step of patient evaluation.
In this study, more than one disrupted criterion was most significantly associated with hospitalization in the hospital and PICU. Under emergency supervision, all disrupted PAT criteria were significantly associated with hospitalization. As a result, the PAT is a good criterion for showing urgent cases and hospitalization in the first step of patient evaluation and raises the need for education in this field.
Furthermore, it is worth noting that the PAT exhibited a statistically significant relationship with hospitalization (OR = 33.30, P = 0.000). Investing in education and training in this domain can effectively mitigate complications and alleviate financial burdens on both families and the healthcare system of the country. Naturally, an experienced and well-trained doctor working in a busy emergency room possesses the expertise to accurately differentiate between patients who are in good health and those who require immediate attention.
The PAT can identify unstable and hospitalized cases more quickly and reduce the likelihood of ignored serious cases. Normal PAT was inversely related to hospitalization (OR = 0.03, P = 0.000) and blood tests (OR = 0.06, P = 0.000), and this indicates the value of using the PAT to determine the severity of the disease and hospitalization. In addition, the high number of blood tests and the accuracy of the PAT in the patient’s hospitalization indicate that the physician’s training in the use of the PAT should be more to use this tool with more confidence in the first step in determining hospitalization cases and urgency in treatment.
This study was a follow-up to a previous study in a center, and some patients with more critical conditions were cared for before the assessment, which increased the percentage of PICU cases and reduced the number of hospitalized cases. Furthermore, the aforementioned issue has diminished the value of the data recorded. However, the researcher recorded the information correctly and before medical procedures, and the large sample size reduced the likelihood of error.
During the study period, which was carried out at the peak of the coronavirus disease 2019 (COVID-19) pandemic, most of its manifestations in children were gastroenteritis (e.g., diarrhea and vomiting, skin rash, fever, skin discoloration, severe abdominal pain, and instability of consciousness) and later in the form of respiratory symptoms that were less, and this in itself conveys the importance of appearance and blood circulation. Additionally, the patients were admitted directly with dehydration and gastroenteritis. Moreover, impaired appearance (MISC and early stages of gastroenteritis) accounted for the largest admissions. They were then stabilized and transferred to the ward. Appearance is the most important component in the PAT triad.
The appearance and more than an abnormal PAT criterion were the most effective factors in hospitalization. Moreover, due to the peak of the COVID-19 period and its manifestation mostly in the form of diarrhea and vomiting and a decrease in body volume, paleness and rash and the effect on the appearance even its effect on hospitalization at the peak of a pandemic was also proven in addition to previous studies.
In the case of hospitalization, due to the filling in the information forms by various reporters and due to the high workload of the resident and the crowded emergency room, in some cases, the patient’s final result has been recorded. For example, a patient with more than one normal criterion has been stabilized under emergency supervision and then transferred to one of the hospital wards, and this in itself has reduced the number of patients under hospitalization with more than one normal criterion and increased its statistics in the hospital. This does not diminish the value of the study results. However, the appearance component with 91.7% after that was the highest rate of hospitalization under emergency supervision, and this is the manifestation and prevalence of COVID-19 in pediatric emergencies and the importance of using the PAT in hospitalization and urgent treatments of this global pandemic.
The advantages of this study include establishing an effective PAT system as a primary evaluation tool for children referred to the pediatric emergency room. This system helps prevent patient confusion, repeated visits, and unnecessary expenses for families and improves disease outcomes.
The current study indicates that impaired PAT findings, when utilized by pediatricians, are associated with increased hospitalization rates even during the peak of the COVID-19 pandemic. This finding emphasizes the importance of physician training in effectively utilizing the PAT as the initial step in evaluating pediatric patients in the emergency room. As a result, unnecessary additional testing can potentially be reduced, enabling physicians to make more confident decisions.
Overall, the present study aligns with previous research (13-16) in highlighting the significance of PAT in pediatric emergency care. It reinforces the notion that the PAT can be a valuable tool for assessing the severity of various conditions and determining the need for hospitalization. However, it is essential to acknowledge that the PAT should not be considered the sole determinant for hospitalization decisions, as other factors might also come into play.
Further research and collaboration among healthcare professionals are necessary to continue exploring the potential benefits and limitations of PAT pediatric emergency care. Building upon the existing knowledge base can enhance patient outcomes and optimize the use of resources in emergency settings.
5.1. Conclusions
The following points can be summarized:
• In both outcomes, multiple disrupted criteria were observed to be strongly associated with hospitalization in the entire hospital. Specifically, disrupted circulation, general appearance of the patient, and respiratory function were identified as the factors linked to hospitalization.
• The simplicity and reliability of the PAT, along with its low cost and time-saving nature, compared to other examination tools, make it a compelling option.
• The accuracy of this study demonstrates that the PAT is a straightforward and dependable tool that can quickly determine the need for hospitalization by pediatricians, even during the peak of the COVID-19 pandemic and in emergency room settings.
• The purpose of the study was to investigate the association between disrupted PAT scores and hospitalization at Mofid Hospital. The results indicate that all criteria assessed by the PAT directly and definitively correlate with the need for hospitalization.