1. Background
Acute appendicitis (AA) is one of the leading causes of urgent operations in the pediatric population. It seems that AA’s incidence increases with age. During the first four years of life, AA occurs in one to six per 10,000 children, while this number reaches up to 28 per 10,000 in patients younger than fourteen. On the other hand, the lifetime risk for developing AA is between 7% to 9% (1, 2).
Historically, it is postulated that AA is usually caused by the incidental obstruction of the appendiceal lumen, leading to bacterial overgrowth, vein obliteration, ischemia, and gangrene or perforation. For this reason, its clinical manifestations may vary in each patient. The patient may experience a range of symptoms from mild discomfort in the abdomen to a catastrophic generalized board-like abdomen. However, in most cases, the pain remains in the right iliac fossa (3).
Although several guidelines and scoring systems have been developed to differentiate the disease, AA cannot be diagnosed based on only clinical or laboratory findings (4), and the definite diagnosis relies on the results of clinical, laboratory, and imaging studies together.
Despite recent claims about the conservative management of AA in uncomplicated cases, appendectomy remains the only safe treatment, which can be done either through open or laparoscopic surgery (5). As AA is a progressive disease, untreated cases may develop complications like gangrene, perforations, abscess, or phlegmon. Therefore, rapid diagnosis and surgical intervention are mandatory.
After the onset of the coronavirus disease 2019 (COVID-19) pandemic in early 2020 and subsequent worldwide lockdowns, restrictions, and global fear and panic, many medical procedures were affected remarkably. As the most common surgical indication in children, AA was not an exception (6). The pandemic caused a notable decrease in hospital visits, sometimes even for urgent problems. On the other hand, COVID-19 and AA may present some similar symptoms, possibly leading to misdiagnosis. Manifestations such as diarrhea, vomiting, and gastrointestinal discomfort are some prominent examples (7, 8). In addition, there have been reports indicating a rise in AA complications during the pandemic (6, 9).
2. Objectives
Considering that our hospital is one of the major tertiary referral centers for pediatric diseases, we intended to perform a retrospective analytical survey to validate these hypotheses in our population. This article was prepared in line with the guidelines of the STROBE checklist (10).
3. Methods
3.1. Study Design
In this cross-sectional analytical study, we enrolled all patients with a definite diagnosis of AA before and during the COVID-19 pandemic and compared their characteristics. The study aimed to discover any significant difference in the course of the disease, especially possible complications, between the two groups.
3.2. Setting and Population
This study was conducted at Mofid Children’s Hospital, which is a tertiary center for pediatric diseases and is affiliated with Shahid Beheshti University of Medical Sciences, Tehran, Iran. As an academic referral center, more than 4000 elective and urgent surgeries are performed in this hospital annually. All surgeries are done by trained pediatric surgery fellows under the strict supervision of board-certified pediatric surgeons. In this study, we retrospectively reviewed the patients who had undergone appendectomy over the last two years and divided them into two groups. The pre-pandemic group consisted of patients from February 2019 to February 2020 (i.e., before the official declaration of the pandemic in Iran). The pandemic group included cases referred between February 2020 and February 2021.
We enrolled all the patients who underwent appendectomy based on the International Statistical Classification of Diseases and Related Health Problems 10th Revision (ICD-10). Codes K35 - K38 were indicative of the diseases of the appendix. It should be noted that this study focused only on operated cases, and patients who were managed conservatively did not enter the study.
The clinical diagnosis of acute appendicitis was made based on physical examination, as well as laboratory and imaging studies. We usually use both Alvarado and Pediatric Appendicitis Score alongside ultrasonography to reach the correct diagnosis in our institute (11). The presence of tenderness in the right iliac fossa and leukocytosis, plus a dilated non-compressible appendix in ultrasonography, are highly suggestive of acute appendicitis.
Historically, surgeons use the complicated appendicitis term for situations associated with perforation, gangrene, abscess, or phlegmon (12). On the other hand, early acute appendicitis (or cathartic) refers to a condition where the appendix is congested, but no signs of inflammation are present. These conditions were discerned from and compared with each other according to imaging studies, intraoperative assessment, and pathology examinations.
During the pandemic period, only emergency operations could be done without prior screening for COVID-19 in our institute. As appendicitis is an urgent surgical condition (not emergent), the screening tests were obligatory. For screening the cases during the pandemic, different methods could be implemented by pediatricians, and due to contradictory screening guidelines for urgent surgeries, we also used a combination of various tools for screening, including lung computed tomography, plain chest x-ray, complete blood count, and polymerase chain reaction (PCR).
3.3. Inclusion and Exclusion Criteria
Despite the definition of childhood (i.e., age between 0 and 18 years) stated by the World Health Organization (WHO) (13), we enrolled all patients who were younger than 14 years of age. Also, only the cases that underwent surgery (either in an open or laparoscopic manner) were included. Patients who underwent appendectomy along with another surgery and those with congenital anomalies were excluded. As the COVID-19 infection may mimic the characteristics of the multisystem inflammatory syndrome in children (MIS-C), those who met the criteria for this condition were also excluded from the study (14).
3.4. Data Collection
We collected patients’ information recorded in an internal electronic health system and extracted the data into a digital dataset. All medical files were reviewed by experienced surgeons. Demographics, clinical signs and symptoms, laboratory data, imaging findings, and perioperative information were successfully imported into the main dataset. On the other hand, files with missing or lost data were excluded.
3.5. Statistical Analysis
We analyzed the dataset using Statistical Package for the Social Sciences (SPSS) version 26 (IBM, Armonk, NY) software. In order to describe scale variables such as age and laboratory data, central tendency and dispersion measures were used. On the other hand, for categorical items, we utilized frequencies to present the data. Chi-Square was the primary analytic test for investigating the correlation between two categorical variables. Besides, after ensuring that data distribution was normal according to the Kolmogorov–Smirnov test, the t-test (independent and paired samples) was used to compare the means of numerical variables.
4. Results
4.1. Demographics and Clinical Information
A total of 369 patients were included in the study. The pre-pandemic group consisted of 173 children, while 196 patients were diagnosed with AA during the pandemic, showing no significant difference in the size of the groups (P = 0.232).
Table 1 compares demographic data like age and gender between the two groups. There was no significant correlation between these variables before and after the pandemic. Regarding clinical signs and symptoms, however, fever was detected more frequently in the patients referred during the pandemic (P = 0.001). Moreover, constitutional symptoms like diarrhea and constipation were more common in the pandemic group (see Table 1).
| Variables | Total | Before COVID-19 Pandemic | During COVID-19 Pandemic | P |
|---|---|---|---|---|
| Mean age (mo) | 108.9 | 110.9 (9 - 204) | 107.1 (8 - 204) | 0.344 b |
| Gender | ||||
| Male | 235 (64.3) | 111 (64.5) | 124 (64.2) | 0.955 |
| Female | 130 (35.7) | 61 (35.5) | 69 (35.8) | 0.955 |
| Clinical signs and symptomsc | ||||
| Fever | 56 (16.5) | 6 (3.5) | 50 (29.9) | 0.001 |
| Anorexia | 229 (67.6) | 121 (69.9) | 108 (65.1) | 0.337 |
| Nausea/Vomiting | 261 (76.8) | 130 (75.1) | 131 (78.4) | 0.472 |
| Periumbilical pain | 212 (62.4) | 102 (59.0) | 110 (65.9) | 0.189 |
| Diarrhea | 14 (4.1) | 2 (1.2) | 12 (7.2) | 0.006 |
| Constipation | 9 (2.7) | 1 (0.6) | 8 (4.8) | 0.016 |
| RLQ pain | 233 (68.5) | 87 (50.3) | 146 (87.4) | 0.000 |
| Pain migration | 129 (37.9) | 35 (20.2) | 94 (56.3) | 0.000 |
| Symptom duration (days average) | 1.92 ± 2.1 | 2.14 ± 2.9 | 1.77 ± 1.45 | 0.137 |
| Physical signs | ||||
| RLQ tenderness | 313 (93.4) | 145 (97.3) | 168 (90.3) | 0.96 |
| Peritonitis | 10 (3.0) | 3 (2) | 7 (3.8) | 0.96 |
| Other e | 12 (3.6) | 1 (0.7) | 11 (5.9) | 0.96 |
| Imaging procedures | ||||
| Plain abdominal X-ray only | 51 (15.6) | 44 (27.8) | 7 (4.1) | 0.000 |
| Ultrasonography | 274 (83.8) | 113 (71.5) | 161 (95.3) | 0.000 |
| Computed tomography | 2 (0.6) | 1 (0.6) | 1 (0.6) |
Abbreviations: COVID-19, coronavirus disease 2019; RLQ pain, right lower quadrant pain.
a Values are expressed as No. (%) or mean ± SD.
b P-value estimated by the independent t-test.
c These values were calculated by the chi-square test.
e Includes abdominal distention and the presence of tender or non-tender masses in the right iliac fossa
4.2. Comparison of Perioperative Data
A detailed summary of preoperative, intraoperative, and postoperative variables is presented in Table 2. There was a significant decrease in leukocyte count in the pandemic group (P = 0.007). However, neutrophils, lymphocytes, and their ratio were not notably different between the two groups. Ultrasonography (US) was the most used imaging tool to diagnose AA, performed in 83.8% of the patients. A dilated non-compressible appendix was the most frequent finding in US (67.9%). Beside no remarkable US features in a considerable ratio of patients, common findings in others included mesenteric lymphadenitis, the presence of intraabdominal free fluid, phlegmon, and appendicular abscess, respectively. Phlegmon in US was found to be more common during the pandemic (P = 0.034), but the frequency of appendicular abscesses was comparable between the study groups (P = 0.378).
Open appendectomy was the most common surgical method used in both groups (93.2%). Also, laparotomy and successful removal of the appendix were more commonplace during the pandemic (P = 0.002). Moreover, two laparoscopic conversions were performed on patients in the pandemic group (1%). The rate of using the intraabdominal drainage system in the two groups is shown in Table 2. Intraoperative and pathology reports were also compared, showing a remarkable increase in gangrenous and suppurative appendicitis during the pandemic (P = 0.001).
| Variables | Total | Before COVID-19 Pandemic | During COVID-19 Pandemic | P |
|---|---|---|---|---|
| Preoperative | ||||
| Laboratory findings | ||||
| Leukocytes (WBC) | 13636 ± 9501 | 15059 | 12308 | 0.007 |
| Neutrophils | 74.35 ± 13.11 | 74.21 ± 13.6 | 74.46 ± 12.6 | 0.863 |
| Lymphocytes | 20.29 ± 12.3 | 21.47 ± 12.9 | 19.23 ± 11.7 | 0.096 |
| NLR | 5.8 ± 4.7 | 5.5 ± 4.6 | 6.05 ± 4.8 | 0.292 |
| Ultrasound findings | 0.006 | |||
| Dilated non-compressible appendix | 178 (67.9) | 76 (74.5) | 102 (63.7) | |
| Intraabdominal fluid | 15 (5.7) | 9 (8.8) | 6 (3.8) | |
| Mesenteric lymphadenitis | 17 (6.5) | 9 (8.8) | 8 (5.0) | |
| Appendicular bbscess | 4 (1.5) | 1 (1.0) | 3 (1.9) | 0.378 |
| Phlegmon | 5 (1.9) | 0 | 5 (3.1) | 0.034 |
| Normal | 42 (16) | 7 (6.9) | 35 (21.9) | |
| Intraoperative | 0.002 | |||
| Operative procedures | ||||
| Open appendectomy | 340 (93.2) | 170 (98.3) | 170 (88.5) | |
| Laparotomy | 15 (4.1) | 3 (1.7) | 12 (6.3) | |
| Successful LA | 8 (2.2) | 1 (1.0) | 7 (2.0) | |
| LA required conversion | 2 (0.5) | 0 | 2 (1.0) | |
| Drain used? | 33 (9.0) | 11 (6.4) | 22 (11.5) | 0.090 |
| Intraoperative diagnosis | ||||
| Acute Apx | 175 (47.9) | 112 (64.7) | 63 (32.8) | 0.000 |
| Suppurative Apx | 112 (30.7) | 23 (13.3) | 89 (46.4) | 0.000 |
| Gangrenous Apx | 53 (24.5) | 27 (15.6) | 26 (13.5) | 0.522 |
| Abscess | 22 (6.0) | 8 (4.6) | 14 (7.3) | 0.308 |
| Postoperative | ||||
| Pathology report | 0.000 | |||
| Early acute Apx | 39 (14.1) | 6 (7.1) | 33 (17.3) | 0.000 |
| Acute Apx | 83 (30.1) | 51 (60) | 32 (16.8) | 0.003 |
| Suppurative Apx | 85 (30.8) | 17 (20) | 68 (35.6) | 0.000 |
| Gangrenous Apx | 51 (18.5) | 10 (11.8) | 41 (21.5) | 0.000 |
| Perforated Apx | 7 (2.5) | 1 (1.2) | 6 (3.1) | 0.081 |
| Vermiform | 11 (4) | 0 | 11 (5.8) | 0.000 |
| Hospitalization (h) | ||||
| < 24 | 18 (5.3) | 11 (7.6) | 7 (3.6) | 0.101 |
| > 24 | 322 (94.7) | 134 (92.4) | 189 (96.4) | 0.163 |
Abbreviations: COVID-19, coronavirus disease 2019; WBC, elevated white blood cell count; NLR, neutrophil-to-lymphocyte ratio; LA, laparoscopic appendectomy; Apx, appendicitis.
a Values are expressed as mean ± SD or No. (%).
4.3. Complicated Appendicitis
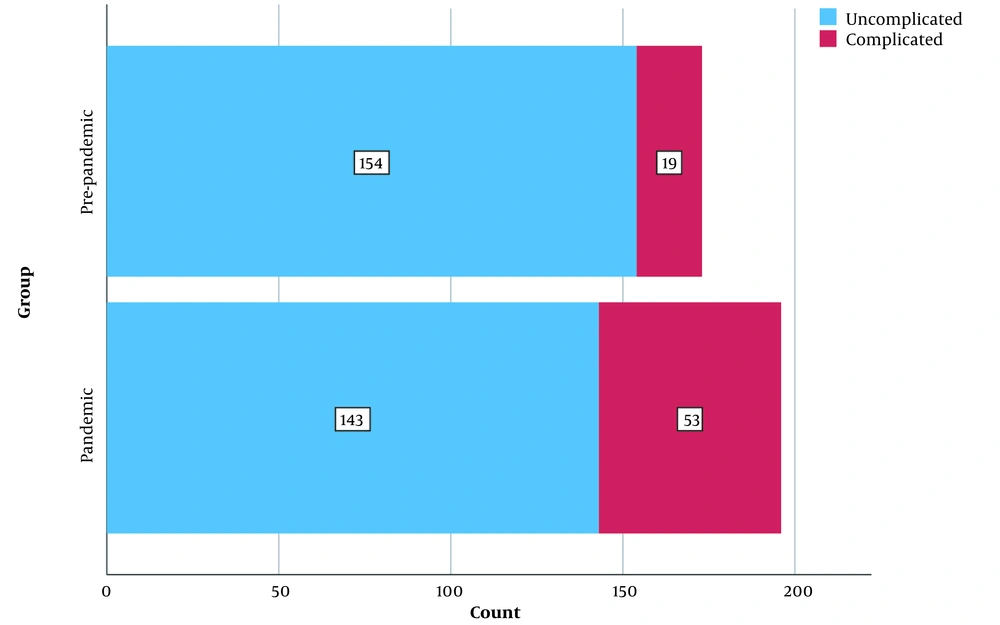
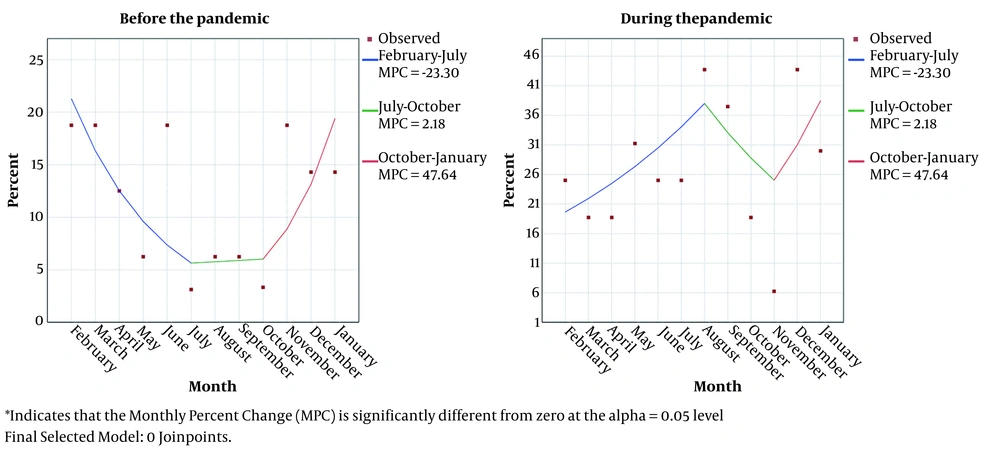
As previously stated, complicated appendicitis is characterized by perforation, gangrene, phlegmon, and appendicular abscesses. In the pre-pandemic period, 19 (11%) patients developed complicated appendicitis, while in the pandemic era, this number raised to 53 (27%, P = 0.000, Figure 1). Also, Figure 2 shows the monthly trends of the aggregate rate of complicated appendicitis.
The monthly trend of complicated appendicitis. The left graph represents the pre-pandemic era, showing a descending rate of complicated acute appendicitis from February to July. On the other hand, the right graph (peri-pandemic era) shows increased rates of complicated acute appendicitis in these months.
4.4. Screening Methods
Lung computed tomography (CT) was the most common screening tool in our patients (54.6%), followed by the combination of CXR and CBC (35.2%). On the other hand, PCR was the sole screening test in only ten patients (5.1%), and in thirteen cases, PCR was performed preoperatively. Moreover, postoperative PCR was performed for seven patients, two of whom returned positive results (1.1%). In addition, fever was the most clinical symptom (28.6%) among the patients, urging clinicians to consider it as one pillar of the screening methods. For more detailed information, please refer to Table 3. In addition, we came across five positive cases for COVID-19; nevertheless, no significant correlation was found between COVID-19 and the development of complicated appendicitis (four uncomplicated vs. one complicated, P = 0.978).
| Methods | No. (%) |
|---|---|
| Screening methods | |
| Lung CT | 107 (54.6) |
| X-ray + CBC | 69 (35.2) |
| PCR | 10 (5.1) |
| Lung CT + PCR | 3 (1.5) |
| Nothing | 3 (0.5) |
| PCR before surgery | |
| Positive | 4 (2) |
| Negative | 9 (4.6) |
| Not done | 177 (90.3) |
| Lung CT | |
| Positive | 1 (0.8) |
| Negative | 119 (99.2) |
| PCR after surgery | |
| Positive | 2 (1.1) |
| Negative | 5 (2.6) |
| Not done | 183 (96.3) |
| Suspected COVID-19 symptoms | |
| Fever | 56 (28.6) |
| Exhaustion | 3 (1.5) |
| Myalgia | 1 (0.5) |
| None | 130 (66.3) |
| Mean admission time (days) | 3.34 ± 2.2 |
| Positive COVID-19 | 8.0 a |
| Negative COVID-19 | 3.29 a |
Abbreviations: CT, computed tomography; CBC, complete blood count; PCR, polymerase chain reaction; COVID-19, coronavirus disease 2019.
a P = 0.000
5. Discussion
Although we cannot re-estimate lifetime risk with the existing data during the pandemic, some nationwide studies have shown contradictory results regarding the annual risk of AA during the pandemic, some of which report a significant decrease in the overall number of patients diagnosed with AA during the pandemic (15, 16). Conversely, many studies reported an increased risk of complicated AA during the pandemic (15, 17). In our study, despite an increase in the number of AA cases after the pandemic, we could not find any significant difference in the number of cases between the pre-and peri-pandemic periods (P = 0.232). This may be due to more referrals of children to tertiary centers due to the lack of empty beds in general hospitals. Also, we witnessed a definite dominancy in the number of male patients. Boys were affected almost twice as girls, which is in agreement with the fact that AA is more prevalent in male children (18).
Clinically, AA may present with various symptoms. Mild periumbilical pain followed by a drastic localized pain in the right lower quadrant is the general picture and is highly indicative of AA. However, symptoms may vary from mild gastrointestinal discomfort to extreme generalized abdominal pain (19). Children may not express pain well, so a physical examination may be challenging in this population. The typical history of migratory pain or localized tenderness may be absent in many cases. This problem is considered one of the leading causes of the higher rate of complicated AA in children (20). In addition, the presence of tenderness, rebound tenderness, or coughing tenderness seems to be a reliable finding with a high predictive value for the diagnosis of AA (21).
Traditionally, leukocytosis (elevated white blood cell count (WBC)) and left shift in leukocyte maturation confirm the clinical suspicion of AA. Most of our patients showed leukocytosis in peripheral blood. Recently, the neutrophil-to-lymphocyte ratio (NLR) has been introduced and utilized for AA diagnosis. A systematic review conducted in 2020 declared that NLR > 4.7 could be used as an independent predictor of AA, while NLR > 8.8. is associated with complicated AA (22). The mean of NLR in our patients was 5.8, supporting the predictive role of the NLR mentioned above. On the other hand, the average NLR in our complicated cases was 7.0, which is far less than the cutoff of 8.8. Overall, NLR showed a statistically significant increase in complicated cases, suggesting an association between higher NLR values and complicated appendicitis. However, in many tertiary centers, more complex scoring systems are employed to diagnose AA. The Alvarado and pediatric appendicitis score are the most famous scoring systems used in children (23).
One of the diagnostic challenges of appendicitis during the COVID-19 pandemic was MIS-C, which may be misdiagnosed as severe acute appendicitis. In addition to fever, MIS-C is usually associated with laboratory evidence of inflammation, multisystem organ failure, and a past or present history of episodes of the SARS-CoV-2 infection (24). Severe cases of AA may be misdiagnosed as MIS-C or vice versa. Fortunately, in our study, none of the children with AA met the diagnostic criteria of MIS-C.
The mainstay of treatment in AA is surgical intervention, which can be done openly or via minimally invasive procedures like laparoscopy or robot-assisted surgery. Besides, in patients with peritonitis, a midline laparotomy may be necessary. Although we had fewer open appendectomies during the pandemic, laparotomy was conducted at a much higher rate during this period. Despite the fact that there were some concerns about the transmission of COVID-19 during laparoscopic surgery in positive patients (25), a remarkable proportion of AA cases in our center were managed with the aid of laparoscopy.
As we mentioned earlier, complicated appendicitis stands for situations associated with complications like gangrene, perforated appendicitis, abscess, and phlegmon. The diagnosis of these problems is mainly based on clinical and pathological examination. Our findings suggested a significant increase in the rate of complicated AA during the pandemic, which is consistent with numerous previous reports (26-28). A similar study performed in 2021 compared the possible complications of AA before and after the COVID-19 pandemic, reporting a significant increase in complicated AA after the outbreak (21%), while the rate of uncomplicated AA diminished notably in this period (27). Another study in France estimated an 11% increase in the incidence of complicated AA during the pandemic (29). A recent systematic review of more than 350 research articles, including 46 validated studies, declared a higher risk of complicated AA during the pandemic (28); however, this change in the trend of complicated AA was not statistically significant in children. We also observed a 16% (27% vs. 11%) increase in the rate of complicated AA after the COVID-19 pandemic. The increase in the incidence of complicated AA might indicate that children did not receive appropriate and timely surgical management during the recent outbreak.
Also, we can consider perforated AA as the most severe type of complicated appendicitis. We found a statistically non-significant increase (1.9%) in the frequency of perforated appendicitis during the COVID-19 pandemic in our study. Some studies evaluated the incidence of perforated appendicitis during the pandemic. In a retrospective cohort study on 80 patients, a 19% increase was reported in the incidence of perforated appendicitis after the pandemic (P = 0.04) (30). Another study on 285 children confirmed the growing numbers of perforated appendicitis (45.6% vs. 26.4%; P < 0.001) during the COVID-19 pandemic (31). Our findings and aforesaid reports show that the COVID-19 pandemic has escalated the rate of complicated appendicitis. This is probably due to the reluctance to seek appropriate care following the public fear of being infected by the coronavirus.
5.1. Conclusions
Our results suggest that the rate of complications of appendicitis in children was much higher amid the COVID-19 pandemic. Also, a significantly more ratio of patients underwent midline laparotomy after the outbreak, but this increase in the rate of complicated appendicitis did not affect the length of hospital stay or the incidence of postoperative complications. The increase in the rate of complicated appendicitis during the COVID-19 pandemic suggests that delays in seeking care due to fear of contracting COVID-19 may complicate the natural course of appendicitis in children.