1. Introduction
Acute lymphoblastic leukemia (ALL) is the most common malignancy among children, with 25% prevalence and a cure rate of about 85% (1, 2).
Patients with ALL are susceptible to infection due to a compromised immune system. Infectious diseases are the main cause of morbidity and mortality in childhood cancer. Malignancy can incline children to severe or recurrent infections. Neutropenia has been documented as a major risk factor in the development of infections in patients with cancer, who receive chemotherapy. Effective strategies to find high risk patients, as well as for the management of infectious complications in a timely manner have given rise to improved outcomes (3-6).
Osteomyelitis may occur as the initial manifestation or a sign of disease relapse in ALL. It is usually localized and occurs when a patient experiences a severe and prolonged neutropenia. Here, the study presents a case with simultaneous occurrence of a multifocal osteomyelitis with ALL, during the maintenance phase of treatment.
2. Case Presentation
The patient was an 8-year-old male, who was a known case of precursor B cell type ALL for the past 6 months prior to the study. He was on maintenance phase of treatment with vincristine monthly injection, oral 6-mercaptopurin every night, oral methotrexate weekly, and prednisolone for 5 consecutive days every month. He had fever and malaise for 3 days prior to his admission to an oncology hospital affiliated to Shiraz University of Medical Sciences, Shiraz, Iran, during December, 2015. His physical examination was normal except high grade fever and mild tachycardia. No localizing source of infection was found. Laboratory tests showed pancytopenia and a positive blood culture for Citrobacter (Bactec system). Other investigations, which included, CSF analysis, chest X-ray, brain magnetic resonance imaging (MRI), and echocardiography were done in order to exclude bacterial dissemination, and the results were normal. Piperacillin-tazobactam was started after sampling and continued based on positive blood culture for Citrobacter (without species classification), according to antimicrobial susceptibility testing results. He was discharged from the hospital one week after negative blood culture and termination of fever.
Again, he returned to the hospital after 5 days due to recurrence of fever and neutropenia (absolute neutrophil count 700 cell/µL). His blood culture was positive for Pseudomonas species, and he had high inflammatory indices (erythrocyte sedimentation rate [ESR]: 113 and C-reactive protein [CRP]: 192). Meropenem was administered and continued based on antimicrobial susceptibility testing results; nonetheless, the patient was continuously febrile after 72 hours of treatment. As a result, vancomycin and amphotericin was added empirically to his regimen. In an advance work-up, including chest and paranasal sinus spiral CT scans and echocardiography was normal. Pan-fungal polymerase chain reaction (PCR) panel (aspergillosis, Mucormycosis, and candida) was negative.
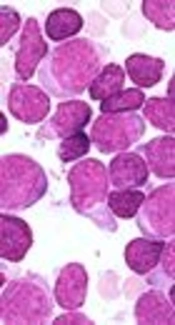
To ensure that the patient is in leukemic remission, bone marrow aspiration and biopsy was performed with normal results. The patient received a full course of antibiotic regimen in the hospital for 3 weeks and was then discharged with negative blood culture.
Once again after 3 days, he returned with left elbow swelling, fever, and bone pain. He had a negative blood culture, leukocytosis (white blood count [WBC]: 28,000/µL [87% neutrophil]), and high inflammatory indices (ESR 100, CRP 96). His bone survey showed multiple bone involvement with periosteal reaction and bone destruction (Figure 1A, 1B, and 1C). Vancomycin and meropenem were switched to linezolid and colistin in order to cover multidrug resistance (MDR) gram positive and gram negative organisms. Synovial aspiration of the left elbow was sent for microbial culture and was negative. Tc99m-MDP bone scan showed an increase radiotracer uptake in both humorous, both tibia, and both femur bones, which were suggestive of multifocal osteomyelitis or leukemic infiltration (Figure 1D and 1E). Bone biopsy was performed and confirmed osteomyelitis diagnosis (Figure 2). The patient was treated with linezolid and Colistin for 8 weeks. He was discharged from the hospital in good general condition without any complications. The patient is currently under regular follow-up, and is being treated for leukemia, as scheduled. After 6 months, no relapse was reported during follow-ups and X-rays showed resolution of periosteal reactions and major bone healing was observed (Figure 1F, 1G, and 1H). It is worth mentioning that written informed consent was obtained from his parents before this report.
A, right humerus X-ray reveals: diffuse metadiaphyseal mottling, rarefaction, significant periosteal reaction with Codman's triangle appearance and soft tissue swelling. There is also a radiolucent area in distal humerus metaphysis suggesting abscess formation. Soft tissue swelling is also noted. There is no squestrum formation; B, left humerus plain X-ray reveals: plain X-ray of the left humerus demonstrates diffuse metadiaphyseal mottling, solid periosteal elevation occupying most of the bone shaft and bone demineralization. There is no evidence of involucrum or abscess formation. Surrounding fat lines are also obliterated suggesting soft tissue edema, periosteal reaction and diffuse bony destruction; C, femoral bones x-rays reveals: Plain X-ray clearly shows bacterial osteomyelitis of both femoral bones consistent with mottling, solid periosteal reaction and a diffuse mixed lytic and sclerotic appearance of the entire diaphysis and metaphysis. Findings are more prominent distally. On the right side, radiolucent defect is also noted in distal femoral metaphysis suggesting abscess formation. Note the slight surrounding sclerotic rim obvious periosteal elevation is also eminent; D and E, Tc99m-MDP bone scan showed increased uptake in both humorous, both tibia and both femur bones; F, G and H, plain X-Ray of the same patient six months post treatment with significant improvement was compared to previous images, F, right humerus; G, left humerus; H, femoral bones.
3. Discussion
Children with ALL may be confronted with bone pain episode during their treatment course. It is necessary to differentiate whether the pain is related to relapse of underlying illness or orthopedic conditions. The main cause of bone pain in children, includes growing pain, hematologic malignancies, rheumatic fever, juvenile rheumatoid arthritis, septic arthritis, osteomyelitis, transient synovitis, primary bone tumors (Ewing sarcoma, osteosarcoma, and osteoid osteoma), neuroblastoma or other solid tumors with bone or bone marrow metastasis, Legg-Calve-Perthes disease, sickle cell anemia, scurvy, and osteonecrosis (7-10).
The incidence of musculoskeletal problems in childhood with ALL is about 40%. The initial presentation in children with ALL can be bone pain, which is commonly localized in long bones and is partly due to leukemic infiltration. This pain is usually described as intermittent, localized, severe, and sudden in onset (8-10).
Normally, osteomyelitis is a localized disease with the femur being the most common site of involvement. However, it may manifest as a multifocal disease in certain clinical conditions (11, 12). The pathogenesis of multifocal osteomyelitis is due to hematogenous dissemination of infection in an immune-compromised host. Bacteremia was much longer than expected along with inappropriate clinical and bacteriologic response, and was the usual suspect in this case. Even though at the time of bone involvement blood culture was negative for citrobacter species, compatible clinical signs and symptoms were accompanied with high grade fever that convinced the medical team of probable hematogenous seeding of citrobacter bacteremia to long bones in this patient. It should be emphasized that the time table of osteomyelitis in immune compromised patients could be different when compared with a healthy individual.
Multifocal osteomyelitis may also occur in patients with sickle cell anemia and recurrent vaso-occlusive crises and ischemia, which could lead to seeding of infection in multiple bones. Patients with acute leukemia are highly susceptible to infection, yet severe osteomyelitis is a rare phenomenon (11, 12).
Multifocal osteomyelitis may occur in a case of leukemia for a variety of reasons, including compromised immune system due to underlying disease or chemotherapy effect, and prolonged antibiotic use. Moreover, high-dose corticosteroid can cause osteonecrosis, which can predispose patients to diffuse bacterial seeding in the setting of bacteremia (13).
De Bernardi et al. reported on 2 cases of leukemia that developed osteomyelitis in the induction phase of therapy, whose synovial fluid culture was positive for citrobacter Freundii (11). However, no microorganism could be isolated from the blood or bone biopsy specimen, which could be due to heavy pre-treatment with different antibiotics during the patient’s previous admissions. Nonetheless, the pathology report confirmed the diagnosis of osteomyelitis.
Therefore, clinicians should be aware of osteomyelitis in febrile neutropenic patients, even if there are no localized signs of infection.
4. Conclusions
Osteomyelitis should be considered in patients with leukemia, who present an unexplained prolonged fever with or without neutropenia. In neutropenic patients, localized signs of infection could be absent. Multifocal osteomyelitis can occur in leukemia patients and should be distinguished from bone marrow relapse. This report suggested the seriousness of MDR resurgence gram negative organisms in oncology wards that occurs due to rapid polymicrobial resistance during prolonged or short-term hospitalization. High index of suspicion is necessary to initiate prompt broad-spectrum anti-MDR gram positive and anti-gram negative antibiotics.