1. Background
As the etiologic agent of coronavirus disease 2019 (COVID-19), SARS-CoV-2 has produced morbidities and mortalities worldwide. Among 17,200 deaths reported in the under-20-year-old population, 47% occurred in children ages 0 - 9 (1). The COVID-19 epidemic, especially as a newly emerging disease in Iran, has caused a great challenge in managing patients (2). As the COVID-19 pandemic continues to affect people, children face challenges due to their critical age (3). Pediatric vaccination is one of those challenging issues. Centers for disease control and Prevention (CDC) recommends COVID-19 series vaccination for everyone aged six months or older and COVID-19 boosters for everyone aged five years or older (4). However, based on a CDC report published in July 2022, among US children aged 5 - 11 years, 37% received at least one dose of the COVID-19 vaccine, and 30% completed two-dose vaccination series (5). In the US, the leading predictors of willingness to vaccinate children were belief in the benefits of COVID-19 vaccination and acceptance of routine childhood vaccines (6).
A COVID-19 vaccine hesitancy survey across the eastern Caribbean subregion of UNICEF showed that “being too young” and “choosing not to vaccinate” were the main reasons for hesitancy (7), and parents’ trust/untrust in “fake news” information had an association with their decision to vaccinate their children (8). In Italy, parents who were less educated or had a lower perceived risk that SARS-CoV-2 could infect their children showed a lower willingness to vaccinate them. Only 38.8% of parents were keen to vaccinate their children against COVID-19 (9). In Quebec, parents who were themselves vaccinated but hesitated for their child’s vaccination believed that it is unnecessary due to lower COVID-19 complications in children. They were also concerned about the side effects of COVID-19 vaccination (10). Another study conducted in Saudi Arabia based on the health belief model showed “low benefits” and “lack of safety” as causes of the hesitancy of children’s vaccination against COVID-19 among parents (11).
2. Objectives
At the time of data collection, despite the availability of vaccines in Iran, about 60% of children aged 5 to 11 years had not received any dose of the COVID-19 vaccine. Due to the issue’s importance, we decided to design this study to investigate the causes of the unwillingness of parents to vaccinate children against COVID-19 among parents in Shiraz, Iran.
3. Methods
In this cross-sectional study, we used an online questionnaire to determine the attitude toward COVID-19 vaccination and associated factors among parents who did not vaccinate their 5 - 11-year-old offspring. The questionnaire was created based on a literature review and editing by two independent epidemiologists (to ensure face validity) and assessed by four specialists, including an epidemiologist, a pediatrician, an infectious disease specialist, and an immunologist (to ensure content validity). The questionnaire contained demographic questions, 16 beliefs about COVID-19 and vaccination against it, and their source of information about COVID-19. Statistics experts were consulted to estimate the required sample size for the study, resulting in a total number of 738 parents with a 95% confidence level. We sent our questionnaire’s online link to elementary schools’ health teachers in Shiraz, Iran, and asked them to share it with parents. After data gathering, we checked our database, cleared uncompleted ones, and imported the rest into IBM SPSS version 21 for analysis.
4. Results
This study analyzed 1,093 respondents, including 49.5% (n = 542) male and 50.5% female students’ parents. The mean age was 36.67 ± 4.81 for mothers and 41.22 ± 5.50 for fathers. The mean age of children was 8.87 ± 0.048. The mean number of children of these parents was 1.92 ± 0.02. According to parents’ educational status, most of them had a high school diploma or master’s degree (Table 1), and 74.8% of mothers and 53.4% of fathers were homemakers and self-employed, respectively (Table 2). Most of the parents were vaccinated with 2 - 3 doses against COVID-19 (82.8% of mothers and 84.3% of fathers).
| Education | Mothers (%) | Fathers (%) |
|---|---|---|
| Under diploma | 13.9 | 20.2 |
| High school Diploma | 33.2 | 34.1 |
| Bachelor | 12.5 | 12.3 |
| MS | 30.3 | 20.5 |
| MSc | 7.7 | 9.7 |
| Doctor | 2.3 | 3 |
| Profession | Percentage |
|---|---|
| Mothers | |
| Housewife | 74.8 |
| Teacher or professor | 6.6 |
| Government staff | 4.5 |
| Private staff | 3.2 |
| Health worker | 2.7 |
| Self-employed | 4.8 |
| Others | 3.4 |
| Fathers | |
| Unemployment | 2.7 |
| Teacher or professor | 3.7 |
| Government staff | 19.7 |
| Private staff | 9.0 |
| Health worker | 1.1 |
| Self-employed | 53.4 |
Parents were asked about their beliefs or reasons for not vaccinating their children. According to the literature review and expert opinions, we chose 16 motives and reasons, and parents answered yes or no (Table 3).
| Wrong Beliefs or Explanations | Yes (%) | No (%) |
|---|---|---|
| I did not know that my child should be vaccinated. | 30 | 70 |
| I haven’t had the chance to vaccinate my child yet. | 28.8 | 71.2 |
| Crowded vaccination center | 12 | 88 |
| I am worried my child will have a developmental disorder after vaccination. | 81.2 | 18.8 |
| I am worried that my child will be infertile after injecting the vaccine. | 76.7 | 23.3 |
| I am worried that my child will have a genetic change by injecting the vaccine. | 74.3 | 25.8 |
| Because the coronavirus does not cause severe disease in my child, vaccination is unnecessary. | 50.9 | 49.1 |
| The available vaccines are not effective in preventing the coronavirus. | 50.9 | 49.1 |
| I am worried that my child will get the coronavirus due to vaccination. | 43.4 | 56.6 |
| The coronavirus vaccine was prepared very early, and it is still too early to start vaccination. | 63.3 | 36.7 |
| The COVID-19 vaccine has long-term side effects that will show in adulthood. | 82.7 | 17.3 |
| The pressure from family and friends made me not vaccinate my child for coronavirus. | 18.6 | 41.4 |
| I am waiting for other children and students to get vaccinated; after that, we will also start vaccination. | 36.9 | 63.1 |
| My child has already had the coronavirus and has good immunity, so the vaccine is unnecessary. | 34.1 | 65.9 |
| Because the adults in my family had complications after the vaccination, we decided not to vaccinate our child. | 54.4 | 45.6 |
| We did not vaccinate our child because of the physician’s opinion or because of a special disease of our child. | 11.5 | 88.5 |
The most common wrong beliefs were probable vaccines’ side effects in the future, the undesirable effect of vaccination on children’s growth, and the awful effect of the vaccine on fertility, with the prevalence of 82.7%, 81.2%, and 76.7%, respectively. Among 1093 participants, 78.6% had at least five wrong beliefs or excuses for not vaccinating their children.
The mean number of wrong beliefs was 7.21 ± 2.80 in parents who had boys and 7.78 ± 2.95 in girls’ parents, which was significantly higher in parents who had girls (P-value = 0.001). The false beliefs significantly correlated with mothers’ age (P-value = 0.001) and mothers’ educational level (P-value = 0.000). Older mothers had fewer wrong beliefs (P-value = 0.001). Moreover, mothers who were teachers/professors had a fewer total number of false beliefs than housewives (P = 0.005). We found that unemployed fathers had a higher total number of false beliefs than fathers who were teachers/professors (P-value = 0.027), government staff (P-value = 0.038), and health workers (P-value = 0.033). No significant correlation was found between the age of fathers and the number of false beliefs.
There was an inverse correlation between the education level of parents and the number of wrong beliefs (P-value = 0.000). Another significant inverse correlation was found between parents vaccinated with 2 - 3 doses and the total number of false beliefs compared with parents who did not vaccinate against COVID-19 (P-value = 0.02 for mothers and P-value = 0.009 for fathers). There was no correlation between the number of children in the family and the total number of false beliefs in parents (P = 0.449).
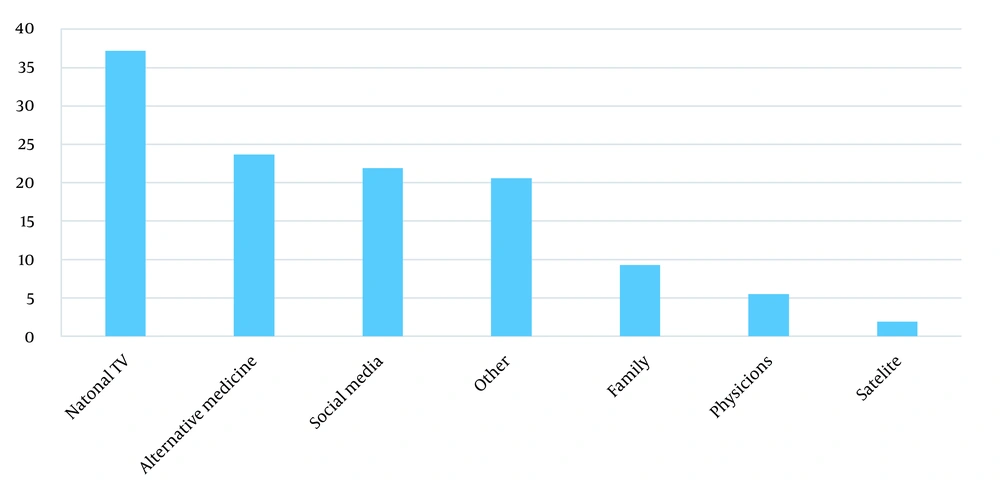
Parents received information about COVID-19 vaccination mostly from national TV (37.2%) and alternative or traditional medicine specialists (23.7%) (Figure 1).
5. Discussion
Vaccination against COVID-19 is necessary to end its pandemic. Studies show that the acceptance of vaccinating children among parents ranged from 48.2% to 72.6% (12). In this study, we aimed to determine the factors leading to low parental acceptance of vaccinating children against COVID-19. For this goal, we asked parents who did not vaccinate their children about their attitude toward injecting the COVID-19 vaccine and what leads them to be unsure about the COVID-19 vaccine.
The number of false beliefs significantly correlated with mothers’ age, so older mothers had fewer false beliefs. This finding is similar to a previous study (13), which showed that parental age is positively associated with a higher determination to vaccinate their children for COVID-19. Among those who answered the questionnaire, more than 80% had over diploma degrees, similar to (14) that found that higher education level correlated with increasing parents’ intention to vaccinate their children for COVID-19. In our study, the education level had an inverse correlation with the number of wrong beliefs. Also, 75% of mothers were homemakers, and about half of the fathers were self-employed. Although only less than 10% of the participants did not vaccinate themselves, they all did not vaccinate their children either. This controversy has been shown in various international studies; for instance, one study from Saudi Arabia mentioned that even though 86.7% of parents in their study were vaccinated against COVID-19, only 47.6% of the parents intend to vaccinate their children (13). Another study from England showed that parents of children were less willing to vaccinate their children than to vaccinate themselves (15).
Most participants believed COVID-19 vaccines have side effects for their children and harm children’s growth and infertility. Among the excuses, doctors’ decisions, crowded vaccination centers, and pressure from other relatives had a lower prevalence (Table 3).
About half of the participants (50.9%) believed the existing vaccines were not effective enough to protect their children against the COVID-19 virus (Table 3). This opinion may be due to the types of vaccines available in Iran.
In multiple comparison analyses, teacher or professor mothers had fewer wrong beliefs about vaccination than homemakers. Fathers who were teachers, professors, health workers, or government workers had fewer wrong beliefs toward vaccination than unemployed ones. There was no correlation between the number of children and parents’ attitudes, while in previous studies, families with more children had a lower willingness to vaccinate (16). While one meta-analysis showed that parents’ age was a significant predictor of vaccination willingness (17), in our study, the older mothers had fewer wrong attitudes about vaccination, and there was no meaningful correlation with the age of fathers. Also, parents vaccinated 2 - 3 times had fewer misconceptions about vaccination, which is approved by other studies (17, 18).
Our study demonstrated that the most preferred information source among parents was national TV, which shows the critical role of national TV in conveying reliable information (Figure 1).
5.1. Limitations and Recommendations
In this study, we mentioned wrong beliefs about COVID-19 vaccination according to specialists’ ideas. We recommend qualitative studies to determine the general population’s concerns about vaccination against COVID-19.
5.2. Conclusions
The average number of wrong beliefs among participating parents was seven, so mass and social media can play game-changer rules in correcting these wrong beliefs toward COVID-19 vaccination and other new-generation vaccines.