1. Background
Antibiotics are the most commonly used medications in the emergency department. Unnecessary antibiotic prescription increases drug resistance and sometimes treatment failure (1). Therefore, antibiotics should be selected with more knowledge and more correctly. If antibiotic stewardship exists, using this model before the empirical administration of antibiotics is useful. However, in practice, broad-spectrum antibiotics are used unnecessarily (2). Various factors can be involved in increasing antibiotic use, such as the economic status of the region (3).
The administration of antibiotics in children is very important in the early diagnosis of the disease and treatment and inhibits progression to sepsis. The treatment strategy focuses on intervention within 60 minutes of visiting the emergency room for children at risk of infection (4).
The difficulty in early diagnostic measures and distinguishing a life-threatening severe bacterial infection from a viral infection causes long observation of the patient, unnecessary radiological procedures, and inappropriate antibiotics in some patients. Bacterial and viral infections have multiple manifestations, making diagnosis and clinical judgment based on history and disease manifestations complex tasks. For example, most febrile diseases in children are caused by viral infections, but antibiotics may be prescribed for these patients (5-7).
Unfortunately, some diagnostic interventions, such as lumbar puncture, are invasive and painful. Using blood culture to diagnose bacterial infections takes time (12 - 48 h), and its false positive result in contamination with dermal and mucosal bacteria limits its use. These cases increase the importance of the clinical judgment of practitioners. In addition, many upper respiratory tract infections among children referred to the emergency department are often caused by viruses, and it is wrong to use antibiotics against them. Therefore, diagnosing bacterial and viral infections alone through clinical judgment is impossible and increases antibiotic prescriptions (8-10).
Inappropriate antibiotics are prescribed at higher rates in the emergency department than in other parts of hospitals (11). Antimicrobial stewardship (AMS) recommendations are rarely observed in emergency departments. Although inappropriate antibiotics are highly prescribed in emergency departments, there are few studies on this issue (12, 13). Therefore, we evaluated the appropriateness of prescribed antibiotics in the children’s emergency department of a hospital with a tertiary level.
2. Objectives
We evaluated the appropriateness of prescribed antibiotics in the children’s emergency department of a hospital with a tertiary level.
3. Methods
This retrospective descriptive cross-sectional study was performed on children referred to Mofid Children’s Hospital, Tehran, Iran. All children referred to the hospital's emergency department were evaluated during January-December 2019.
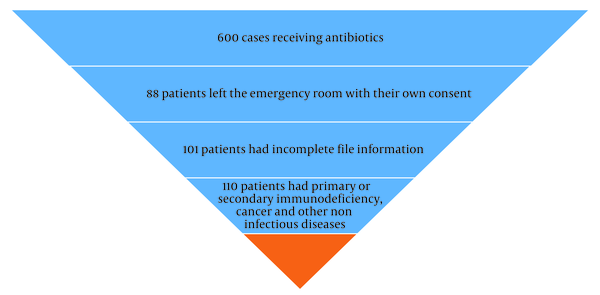
The inclusion criteria were diagnosing a bacterial infection at the emergency department and receiving antibiotic(s). The exclusion criteria were the lack of data on the patient’s file, discharge from the department without any antibiotic prescription, and having a history of immunodeficiency disorders, rheumatic disease, malignancies, or critical condition. Expired patients were also excluded.
All patients were evaluated, and after considering the inclusion and exclusion criteria, a checklist was filled for each patient. The checklist included age, gender, antibiotic appropriateness, laboratory data, body temperature, type of diagnosis, and causes of the inappropriateness of antibiotics. Patients were divided into two groups of effective and ineffective antibiotics. Differentiation between viral and bacterial infection was completed based on radiology and biomarker tests (Figure 1). The radiologic method was lung X-ray, and biomarker tests included C-reactive protein, procalcitonin, and lactate (14). Antibiotic appropriateness was considered as the correct disease diagnosis and prescribing medication with the correct indication and dosage for the disease based on the antibiotic stewardship protocol of Access, Watch, Reserve (AWaRe) classification (2019) (15, 16).
Nine common diseases of children, namely febrile convulsions (FC), pneumonia, gastroenteritis (GE), cellulitis, inflammatory arthritis, urinary tract infection (UTI), COVID-19, meningitis, and sepsis, were evaluated as the diagnosis of patients.
3.1. Statistical Analysis
As the normality test, the Shapiro-Wilk test was performed for all variables, and all had non-normal distribution. Consequently, non-parametric tests were applied for analysis. Mean, standard deviation, frequency, and percentage were used to describe the data. t-test was utilized to compare quantitative variables between two groups, and ANOVA was used for comparing more than two groups. The Fisher's exact test and chi-square test were used for qualitative variables. All analyses were performed by SPSS 25.0 statistical software. P-value < 0.05 was considered statistically significant.
3.2. Ethical Consideration
This study was approved under the ethical approval code of IR.SBMU.MSP.REC.1400.227.
4. Results
Finally, 301 patients were included in the study. The demographic information is presented in Table 1.
| Variables | Total, No. (%) | Antibiotic Appropriateness, No. (%) | P-Value a | |
|---|---|---|---|---|
| No | Yes | |||
| Gender | 0.728 | |||
| Girl | 133 (44.2) | 18 (47.4) | 115 (43.7) | |
| Boy | 168 (55.8) | 20 (52.6) | 148 (56.3) | |
| Age | 0.674 | |||
| 0 - 3 (mo) | 46 (15.3) | 4 (10.8) | 42 (16.0) | |
| 3 - 12 (mo) | 56 (18.7) | 6 (16.2) | 50 (19.0) | |
| 1 - 5 (y) | 116 (38.7) | 18 (48.6) | 98 (37.3) | |
| 5 - 10 (y) | 66 (22.0) | 8 (21.6) | 58 (22.1) | |
| 10 - 15 (y) | 16 (5.3) | 1 (2.7) | 15 (5.7) | |
Demographic Data of Patients Based on Antibiotic Appropriateness
Antibiotic appropriateness was observed in 87.38% and antibiotic inappropriateness in 12.62% of patients. The causes of antibiotic inappropriateness were incorrect diagnosis in 13 (34.2%), incorrect medicine dose in 6 (15.8%), and the lack of indication for prescribed medication in 19 (50%) patients. These rates were 13/301 (4.31%), 6/301 (1.99%), and 19/301 (6.31%) of all research cases.
Table 2 shows the results of laboratory studies based on antibiotic appropriateness.
| Variables | Total, Mean ± SD | Antibiotic Appropriateness, Mean ± SD | P-Value a | |
|---|---|---|---|---|
| No | Yes | |||
| WBC | 9958.87 ± 6035.24 | 7860.53 ± 3796.27 | 10262.05 ± 6240.26 | 0.011 |
| ESR | 31.95 ± 22.87 | 28.76 ± 24.44 | 32.41 ± 22.65 | 0.214 |
| CRP | 37.58 ± 34.29 | 32.68 ± 40.3 | 38.29 ± 33.37 | 0.211 |
| Neutrophil | 53.29 ± 19.31 | 53.26 ± 20.62 | 53.29 ± 19.16 | 0.972 |
| Fecal or urine WBC | 6.22 ± 19.12 | 4.45 ± 17.39 | 6.47 ± 19.38 | 0.169 |
Laboratory Data in the 2 Groups (Appropriateness and Inappropriateness of Antibiotic)
Regarding the number of days of hospitalization in the emergency room and hospitalization in the ward by groups, it was observed that the mean number of days of hospitalization in the emergency room in the ineffective antibiotic group was 1 ± 1 day, and in the other group was 0 ± 1 day. The number of days of hospitalization in the ward was 5 ± 5 days in the ineffective antibiotic group and 5 ± 4 days in the influential antibiotic group (P = 0.837).
The diagnosed disorders based on antibiotic appropriateness are presented in Table 3.
| Variable | Total, No. (%) | Antibiotic Appropriateness, No. (%) | P-Value a | |
|---|---|---|---|---|
| No | Yes | |||
| Diagnosed disorders | 0.495 | |||
| GE | 52 (17.3) | 9 (23.7) | 43 (16.3) | |
| UTI | 28 (9.3) | 2 (5.3) | 26 (9.9) | |
| Sepsis | 23 (7.6) | 5 (13.2) | 18 (6.8) | |
| COVID-19 | 21 (7.0) | 3 (7.9) | 18 (6.8) | |
| Arthritis | 8 (2.7) | 0 (0.0) | 8 (3.0) | |
| Cellulitis | 24 (8.0) | 1 (2.6) | 23 (8.7) | |
| FC | 21 (7.0) | 4 (10.5) | 17 (6.5) | |
| Pneumonia | 117 (38.9) | 13 (34.2) | 104 (39.5) | |
| Meningitis | 7 (2.3) | 1 (2.6) | 6 (2.3) | |
Diagnosed Disease in the Two Groups
Table 4 shows body temperature and fever (axial temperature > 39ºC) in all patients and compares the two groups of antibiotic appropriateness and inappropriateness. Table 5 demonstrates body temperature and fever based on different causes of antibiotic inappropriateness. Based on the findings in Tables 4 and 5, body temperature and fever did not have associations with antibiotic appropriateness, incorrect diagnosis, incorrect dose, or not indicating the antibiotic used.
Body Temperature and Presence of Fever Based on the Causes of Antibiotic Inappropriateness
5. Discussion
In this retrospective study, which aimed to investigate antibiotic appropriateness in patients admitted to the emergency department of Children's Hospital, 87.4% of patients received appropriate antibiotics, and 12.6% received inappropriate antibiotics. The appropriateness of treatment in this study was evaluated based on correct diagnosis, medication indication, and drug dosage. We observed that gender and age were not significantly associated with antibiotic effectiveness. The mean white blood cell count significantly correlated with antibiotic effectiveness, while other laboratory findings had no association with antibiotic effectiveness.
In the current study, the most common reason for the inappropriateness of antibiotics was the lack of indication for prescription. Oomen et al. reported that 24% of antibiotic prescriptions were evaluated as inappropriate (17). In our study, 12.62% of patients received inappropriate antibiotics. Inappropriate antibiotics were prescribed two times more in the study by Oomen et al. than in our research. This discrepancy between the two studies may be due to the fact that the study by Oomen et al. was conducted on all patients who went to the emergency room (adults and children). In contrast, the present study exclusively investigated children.
Onsare et al. concluded that the prevalence of antibiotic prescription errors in children hospitalized in Mbagathi District Hospital was high, and at least one mistake was made every time a medication was prescribed. Therefore, it was recommended that interventions be made to promote the safe administration of antibiotics (18). Their results are in line with the current study and confirm the importance of appropriate and correct antibiotic prescriptions in patients.
Shiva et al.'s study showed that antibiotics were used for 161 people, 20% of which were unnecessary. The prescribed medicine dose and treatment duration were incorrect in 15% and 27% of cases, respectively (19). In our study, 50% of inappropriate prescriptions were due to the lack of antibiotic indication, 15.79% were inappropriate drug dosage, and 34.21% were inappropriate diagnoses, similar to the findings of Shiva et al.
Denny et al. concluded that prescribing inappropriate antibiotics can cause antibiotic side effects, incomplete treatment, and antibiotic resistance. Therefore, it is necessary to increase the accuracy of clinical judgment to prevent antibiotic dependence and damage to society by choosing the correct medication (1). The adverse effects associated with antibiotic use go beyond the development of resistance in target organisms. In some studies, the prescription of antibiotics to patients who were referred to the emergency room for otitis media, sinus infections, and pneumonia were evaluated. It was concluded that when antibiotics are given frequently at the beginning of life and without clinical assessment, they will be effective in promoting intestinal dysbiosis and causing arthritis, inflammatory bowel disease, asthma, and diabetes (20-22). Although the correct administration of antibiotics has made significant progress in the last decade, there is still a need for further studies due to complications and antibiotic resistance. The need for long-term care, cultural influences on antibiotic prescribing, comparison of different drug regimens, duration of treatment, parenteral versus oral therapy, optimal dosing strategies, development and validation, and criteria that consider the potential harms of antibiotics are all critical in choosing an effective antibiotic. Even when the appropriate drug and dose are prescribed, duration of therapy is an important goal of care (23). We also found that the incorrect prescription of antibiotics in one of the largest children's referral hospitals in Iran had a high prevalence, which shows the urgent need to review the therapeutic and educational methods. El Feghaly et al. emphasized that very few specialized children's treatment centers have dedicated standard antibiotic prescription patterns for hospitalized patients to promote treatment efforts, and this issue requires the implementation of appropriate plans by managers (24).
Consideration of the prevalence rate of the most common childhood infections, such as non-specific upper respiratory infections, bronchiolitis, acute bronchitis, exacerbation of asthma, or conjunctivitis, is critical. Regarding the epidemiology of bacterial infections requiring antibiotics in the outpatient setting, it has been conservatively estimated that antibiotic prescribing could be safely reduced by 30%, and there is no need to prescribe an antibiotic. Implementing a systematic approach to follow-up negative culture results and discontinuing the antibiotics initiated based on early signs and symptoms can also reduce antibiotic exposure (25).
In a study conducted at our hospital, 140 children were assessed, and it was found that the most common treated infectious disease was UTI (33.5%). Dosing error was about 7%, and the prolonged duration of antibiotic treatment was observed in 25.6% of cases (26). One of the advantages of our study was the larger statistical population of our study compared to similar investigations. In the current study, we assessed 301 patients, which was more than 2 times higher than the study by Shiva et al. (26). The rate of dosing error was about 2% in the present study, which was lower than the research by Shiva et al. This difference may show an increase in the knowledge of pediatricians about antibiotic prescription, but it should also be investigated in future studies.
5.1. Conclusions
According to our results, the incorrect prescription of antibiotics due to incorrect diagnosis, incorrect drug dosage, and lack of indication for prescribed medication in Mofid Children's Hospital has a significant prevalence that requires further investigation and resolution methods for decreasing these mistakes.