1. Background
Cystic fibrosis (CF) is an autosomal recessive disorder that affects multiple organs in the body (1). Cystic fibrosis is caused by a defect in the CFTR gene (2). Mutations in the CFTR gene, resulting in insufficient production of CFTR proteins, induce chronic and severe inflammatory responses, especially in the lungs, sweat glands, gastrointestinal tract, and reproductive system (3).
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) induces several respiratory and non-respiratory symptoms. Fever, cough, dyspnea, sore throat, fatigue, and gastrointestinal discomfort are commonly observed among affected patients (4, 5). Additionally, the coronavirus disease 2019 (COVID-19) pandemic has placed a significant burden on both national and international healthcare systems (6). Fear of infection by coronavirus in Iran caused Iran several huge COVID-19 waves; therefore, Iranians experienced significant mortality and morbidity (7, 8). Among those who have recovered, many continue to experience post-COVID-19 symptoms that impact their respiratory functions (9-11).
Furthermore, COVID-19 can lead to more severe respiratory complications in patients with comorbidities such as CF, cardiovascular diseases, respiratory illnesses, and obesity. Cystic fibrosis patients are particularly susceptible to super-infections due to the limited effectiveness of their innate immunity (2, 9, 11, 12). Additionally, Mathew et al., in their meta-analysis, depicted more CF individuals during COVID-19 presented with high-grade fever and fatigue and needed supplemental oxygen therapy due to a decrease in oxygen saturation (2). Therefore, COVID-19 poses a significant risk to CF patients and places a substantial burden on healthcare systems (13).
The SARS-CoV-2 pandemic has disrupted patients’ access to medications, routine care, and visits to physicians (13-15). The lack of proper treatment can exacerbate the disease, necessitating hospitalization and increasing the risk of various respiratory infections, especially SARS-CoV-2 and Pseudomonas aeruginosa (9, 12).
2. Objectives
In the current study, the aim was to report on the complications caused by the COVID-19 pandemic in the routine medical care of CF patients during the SARS-CoV-2 pandemic compared to before. Additionally, this study compared COVID-19-infected CF patients with non-infected CF patients. Notably, this is the first study to evaluate these parameters in Iran.
3. Methods
A descriptive retrospective study was conducted at Mofid Children's hospital in Tehran, Iran, to assess the impact of COVID-19 on patients with CF. This study enrolled all confirmed CF patients who presented at Mofid Hospital between March 2020 and May 2022 for the present study. The inclusion criteria encompassed all CF patients visiting Mofid Hospital; however, the exclusion criteria included patients (or their parents) who chose not to participate in the current questionnaire. Furthermore, the World Health Organization (WHO) COVID-19 criteria (guidelines) were used for patient confirmation.
A valid and reliable questionnaire was completed by a single nurse practitioner and a pediatric pulmonary fellowship physician by CF patients and their parents, following verbal informed consent obtained via telephone. Additionally, hospital medical records were utilized to corroborate data and complete the remaining sections of the questionnaire. Consequently, the present study initially included 200 patients; however, due to the unwillingness of 72 participants, the study proceeded with 128 participants. The information collected via the questionnaire encompassed demographic data, patients’ height, patients’ weight, body mass index (BMI), historical and current occurrences of COVID-19-like symptoms, social determinants, and the influence of COVID-19 on routine therapeutic measures for CF patients.
This study has been registered with the Office of the Institute of Board Review at Shahid Beheshti University of Medical Sciences in Tehran, Iran, and has received approval from the Ethics Committee of Research of Shahid Beheshti University of Medical Sciences with the ethical code of IR.SBMU.MSP.REC.1401.362.
3.1. Statistical Analysis
All data were entered into Microsoft Excel software and then analyzed using IBM SPSS Statistics for Windows (Released 2012, Version 21.0, Armonk, NY: IBM Corp). Qualitative variables are presented as frequency and percentage, and quantitative variables are expressed as the mean. Inferential statistics involved calculating differences between study variables using the Chi-square test for categorical variables and the independent two-sample t-test for quantitative variables. Additionally, the normality of quantitative data was assessed using the Shapiro-Wilk test. It is important to note that any P-values less than 0.05 were considered statistically significant.
4. Results
4.1. Participants Overview
In this study, 128 cases participated. Among the study subjects, 59.4% were male. The mean age of the cases was 10.2 years, ranging from 1 to 23 years, and the mean age at the time of CF diagnosis was 20 months, ranging from 1 month to 18 years. Common medications used by the studied patients included Creon, hypertonic saline nebulizer, salbutamol, and vitamins (A, D, E, and K).
Furthermore, among all participants, 13 patients (24.6%) infected with COVID-19 were less than 5 years old; nevertheless, the remaining 40 patients (75.4%) were older than 5 years. Additionally, 2 patients (3.8%) were infected during the initial peak of COVID-19 in Iran (with the Wuhan variant), 9 patients (17%) during the fifth peak (with the Delta variant), and 42 patients (79.2%) during the sixth and seventh peaks (with the Omicron variant).
Moreover, fever, cough, runny nose, sore throat, body pain, gastrointestinal symptoms, and headache were the most frequent COVID-19 symptoms among the studied CF patients (62.3%, 45.3%, 45.3%, 34%, 22.6%, 18.9%, and 9.4%, respectively). Additionally, this study compared the symptoms of fully vaccinated patients against COVID-19 with non-vaccinated patients. The results indicated that among fully vaccinated patients, headache was significantly higher than in non-vaccinated patients (P < 0.05); however, there was no statistically significant difference in other symptoms (P > 0.05).
4.2. Questionnaire Part
As shown in Table 1, the first part of the current questionnaire, used to assess changes in habits caused by the COVID-19 pandemic in the routine care of CF patients, revealed that the majority of the cases performed chest physiotherapy at home, continued routine follow-up with a pulmonologist, and used their previous medications as before (59.4%, 42.2%, and 82%, respectively). Additionally, 65.5% of the participants left home less frequently than before, and approximately 73% of patients’ parents exited their homes less often. Notably, none of these variables showed a significant relationship with SARS-CoV-2 infection (P > 0.05).
| Variables | No. (%) | |||
|---|---|---|---|---|
| Chest Physiotherapy (n = 128) | Patients Exit Home (n = 127) | Parents Exit Home a (n = 127) | Visiting Pediatric Pulmonologist (n = 127) | |
| Less than previous | 21 (16.4) | 84 (65.5) | 108 (85) | 17 (13.3) |
| Same as previous | 76 (59.4) | 21 (16.4) | 19 (15) | 63 (49.6) b |
| More than previous | 18 (14.1) | 12 (9.4) | 0 (0) | 32 (25) |
| Not do it | 13 (59.4) | 10 (7.8) | 0 (0) | 15 (11.7) |
a Approximately 11% of parents just avoided going to crowded places.
b Seven percent of patients visited their doctor only virtually.
Furthermore, the second part of the questionnaire provided information about COVID-19 protection measures among the cases. The majority (60%) of participants wore facemasks to protect against COVID-19 infection everywhere; nevertheless, 12.5% of cases did not wear facemasks anywhere. Moreover, 96 (75%) of the patients were eligible to receive the COVID-19 vaccine according to the guidelines; however, only 32% of patients and approximately 90% of their family members received the COVID-19 vaccine. All vaccinated patients received the Sinopharm vaccine.
Furthermore, among all the participants, 53 patients (41.4%) had a history of COVID-19 infection based on the results of polymerase chain reaction (PCR) tests, chest computed tomography (CT) scans, serological tests, or the presence of common cold-like symptoms in the patient and their family members. Of these patients, 9 cases (17%) required hospitalization due to COVID-19, although none of them needed admission to the intensive care unit (ICU). Additionally, 11.3% of cases received remdesivir and supplemental oxygen. Regarding COVID-19 treatment among the studied CF cases, 48 patients (90.6%) did not experience any changes in their CF medications, and only supportive treatment was administered. Additionally, 3 patients (5.7%) required an increase in the frequency of their previous medications, and amoxicillin-clavulanate was prescribed for 2 patients (3.8%).
4.3. Statistical Part of the Results
A significant relationship was observed between the gender of CF patients and COVID-19 infection (P = 0.01). Among the 78 male subjects with CF, 38 cases (50%) contracted COVID-19; however, among the 52 females with CF, only 15 cases (28.8%) were infected.
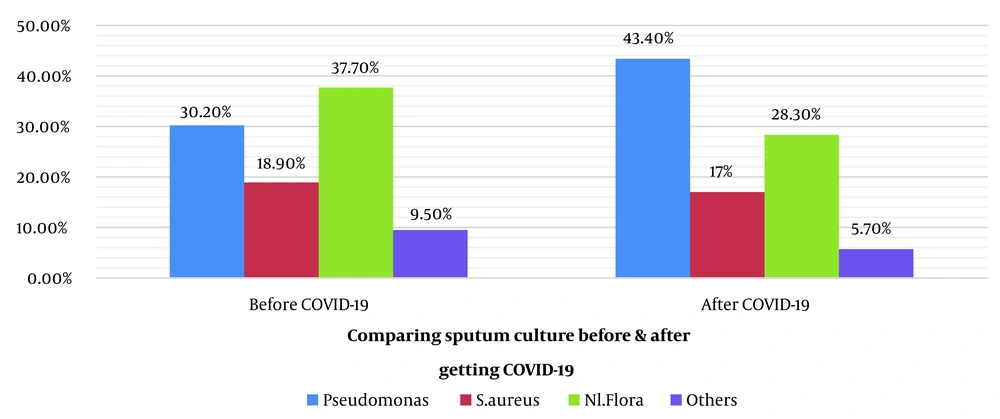
As depicted in Figure 1, the sputum cultures of patients before and after being infected by COVID-19 showed that Pseudomonas aeruginosa and Staphylococcus aureus were the most common pathogens, with no significant statistical difference before and after COVID-19 infections (P > 0.05).
Additionally, 36.6% of patients who did not receive the COVID-19 vaccine had a history of COVID-19. In contrast, 55.9% of fully vaccinated patients (those who received at least 2 doses of the vaccine) had a history of COVID-19 infection. This difference was statistically significant (P < 0.05). Furthermore, 33.3% of patients whose family members did not receive the COVID-19 vaccine were infected with COVID-19. Similarly, 42.6% of patients with family members who were vaccinated were infected with COVID-19 without any significant relationship (P > 0.05).
Half of the patients who were underweight in terms of BMI Z score were infected with COVID-19. Among patients with a normal BMI range, 38.1% had a history of COVID-19 infection. Of the overweight patients, 30.8% were infected with COVID-19. Additionally, 33.3% of obese patients had a history of COVID-19 infection. In this study, BMI did not show a statistically significant relationship with SARS-CoV-2 infection (P > 0.05). However, a significant relationship was observed between contracting COVID-19 and making changes to one’s usual diet (P < 0.05). Among the 33 patients who added various foods, such as tea with honey and lemon juice, garlic, ginger, and citrus fruits, to their diet to prevent COVID-19, the incidence of COVID-19 was surprisingly higher, with 19 of them (57.6%) becoming infected. Conversely, among the 94 patients who continued their usual diet without any changes, 34 patients (36.2%) had a history of COVID-19.
5. Discussion
This study examined the impact of the COVID-19 pandemic on CF patients at Mofid Hospital, a tertiary referral hospital in Tehran, Iran. The current study is the first study in Iran to investigate the presentation of COVID-19 in CF patients. This study collected data from a total of 128 participants who completed the questionnaire. The data were meticulously analyzed and reviewed by an expert single nurse practitioner and a pediatric pulmonary fellowship physician. The questionnaire inquired about changes in routine diagnostic and therapeutic care for CF patients since the onset of the pandemic.
Havermans et al. (14) reported that during the pandemic, 32.9% of parents of children with CF performed physiotherapy more effectively, 24.7% performed it less effectively, and 15.1% had forgotten to do physiotherapy. In Boni et al.’s study (16), 47.6% of parents found that physiotherapy was more effective than before. It seems that in the studies of other countries during the pandemic, physiotherapy was performed unchanged or more than before (17). This difference might be attributed to cultural variations in Iran and inadequate patient education on the importance of physiotherapy. However, there was no significant relationship between the frequency of chest physiotherapy and COVID-19 infection in the present study.
Regarding changes in patients and their family activity outside the home, the current study did not find a significant association with the likelihood of contracting COVID-19. Nevertheless, another study (14) demonstrated that all parents reported that the patient always stayed at home, 73.4% of parents reduced their family’s outdoor activity, 10.9% avoided being in crowded places, and 15% did not follow any instructions. In the aforementioned study, 74% of children with CF used facemasks as soon as they left home. These differences could be due to variations in COVID-19 restrictions and lockdown measures applied in other countries and differences in public awareness and adherence to health guidelines (11, 13, 14, 18).
Havermans et al. (14) also noted that 28.8% of children with CF followed their medication regimen more closely during the pandemic. In addition, in Boni et al.’s study (16), 43% of patients reported that they had more adherence to their drug treatments due to having more free time. In the current study, however, some patients made arbitrary changes in their drug treatments. Proper education about the importance of consistent CF medication use might be needed for parents of CF patients.
Approximately 75% of the patients were eligible to receive the COVID-19 vaccine according to the Ministry of Health guidelines; however, only 32% of participants had been vaccinated. This discrepancy might be attributed to concerns about the vaccination and the lack of WHO approval for their use in children. Nonetheless, the vaccination rate among patients’ families was relatively acceptable.
In the present study, around 41% of patients were infected with COVID-19. A systematic review by Mathew et al. (2) reported a lower infection rate of 1.8% among CF patients than in the general population. Furthermore, 17% of patients required hospitalization due to COVID-19, consistent with the results of Colombo et al.’s study (19) and Carr et al.’s study (20). However, another study showed that (21) only 1.3% of patients needed hospitalization. In Simonson et al.’s study (15), 8% of patients needed hospitalization, and 85% did not need any treatment. Probably, the difference in the time of conducting the study, due to the different common variants of coronavirus, explains why the present study reached a higher prevalence.
In this study, it was observed that 24.6% of COVID-19-infected patients were less than 5 years old; however, Rahimi et al. (22) mentioned that the most common age group affected in children was between 1 and 4 years.
By comparing sputum culture results before and after COVID-19 infection, there was an increase in the probability of positive sputum culture with Pseudomonas after COVID-19 infection. This finding aligns with the findings of Rakhshan et al. (12), who identified Pseudomonas aeruginosa as a common superinfection among CF patients.
In the current study, 79.2% of COVID-19 infections were associated with the Omicron variant. This contrasts with Thouvenin et al.’s (18) findings that before the Omicron variant, 9% of CF patients had a history of COVID-19 infection; nonetheless, during the Omicron peak, 32% were infected. The widespread distribution of the Omicron variant in the community might explain this increase in infections among CF patients.
Furthermore, the present study showed that 36.6% of unvaccinated patients had a history of COVID-19; however, 55.9% of fully vaccinated patients had a history of infection. This difference was statistically significant. It is related to the subtype of coronavirus infections in the current studied patients, Omicron. The COVID-19 vaccines had typically induced immunization for previous subtypes of coronavirus. Moreover, in patients who have not been injected with booster doses, the effect of the vaccine was neutralized (23). Moreover, some of the studied patients had coronavirus before the time of injection.
In addition, among fully vaccinated patients, the headache was significantly higher in COVID-19-infected patients. In the study of Thouvenin et al. (18), the symptoms were similar in vaccinated and non-vaccinated patients. Furthermore, similar to many previous studies (5, 9-11, 14, 15), the coronavirus clinical findings of the current study, for instance, fever, cough, sore throat, body pain, and gastrointestinal symptoms, were the same. However, in various COVID-19 waves, several symptoms were highlighted.
Furthermore, Simonson et al. (15) showed that the average BMI among CF patients who were infected with COVID-19 was 22.4 kg/m2. In Carr et al.’s study (20), underweight patients had a more severe infection caused by COVID-19, and being overweight acted as a protective factor. The possible cause of this difference between the present study and similar studies was that those studies were conducted on adults, and there is a need to conduct further studies on children.
Although the present study provided valuable information, it is suggested that future studies report detailed information on CF patients’ care habits during the SARS-CoV-2 pandemic with more participants.
5.1. Conclusions
A descriptive retrospective study at Mofid Children's Hospital, Tehran, Iran, to determine the impact of COVID-19 on CF patients provided valuable information about the demographics and routine care habits of CF patients during the COVID-19 pandemic. To summarize, CF patients' habits were not significantly changed during the COVID-19 pandemic. Interestingly, COVID-19 was significantly common among CF male patients. Moreover, headache, as the most common symptom, played a role among vaccinated patients.