1. Background
Fever is an indication of a condition triggered by the immune system, responding to cytokines that stimulate brain prostaglandins to increase body temperature (1). Infections are the primary causes of fever, often resulting from invasive pathogens, while cancers and inflammatory responses are also contributing factors (2, 3). Proper management and response to fever can prevent future complications. Children are particularly susceptible to fever, commonly experiencing body temperatures of up to 40°C (4), which may lead to convulsions. Seizure damage, accompanied by disturbances in the metabolism of minerals such as iron (5), underscores the importance of timely intervention.
Parental awareness of fever and increased body temperature is crucial for taking timely action to prevent complications. Pediatricians recommend physical methods (such as bathing and sponging) to reduce fever in children, as these are preferable to conventional treatments. Educated mothers are often more successful at preventing seizures using these physical methods (6). Previous studies have shown that mothers' knowledge and education in managing fever in children are related to their ability to recognize critical temperature thresholds (4, 7). They should also be aware of the proper tools and methods for measuring body temperature in children (8).
The self-prescription of fever-reducing drugs without knowledge of the correct dosage may be linked to the parents' education level. Talebi indicated that mothers with a low education level have limited understanding and quality of knowledge regarding fever and antipyretics (9). Vanessa Castellano suggested that maternal education might reduce mothers' fear of fever and improve primary care for fever (4). The first reaction of Iranian mothers often involves searching for information about fever to reduce their fear, rather than employing physical methods (10). Knowledge and awareness of healthcare professionals are key to preventing many complications of fever in children.
This study complements previous research by closely examining various aspects of mothers' knowledge, such as their understanding of thermometers, antipyretics, and correct dosage prescription.
2. Objectives
We aimed to evaluate how mothers react to fever and use antipyretics. Mothers of febrile children who visited the pediatric emergency department described their knowledge and awareness of fever.
3. Methods
A descriptive, cross-sectional study was conducted in Bandar Abbas, the center of Hormozgan Province in southern Iran, at Bandar Abbas Children’s Hospital. This research adhered to the strengthening the reporting of observational studies in epidemiology (STROBE) guidelines for reporting observational studies.
We obtained ethics approval from the Ethics Committee of the Hormozgan University of Medical Sciences (ethics code: IR.HUMS.REC.1401.142). A checklist was prepared by infectious disease specialists at the hospital, and based on this checklist, information was gathered from the mothers of children with fever.
Participants were randomly recruited from mothers whose children had a temperature higher than 38°C at the time of hospital admission. The selection period was from June 22 to August 23, 2022. Considering the hot weather during these months in the research area, we ensured that the increased temperature was not due to heatstroke (based on patient history). The confirmation of fever with pathological causes was validated by infectious disease specialists.
The desired information was collected through a 15-parameter checklist prepared under the supervision of the Department of Pediatrics. The checklist included the following items: Mother's age, mother's education level, number of children, child's age, temperature usually considered as fever, how the mother became aware of the child's fever, type of thermometer used, type of antipyretic medication used, the time intervals for administering antipyretic medication, history of febrile seizures in children, the mother's approach to dealing with a febrile child at home, and awareness of possible complications such as seizures and brain damage.
The sampling method was systematic random sampling of patients referred to a pediatric hospital in Bandar Abbas. Among the 856 patients with fever who met our inclusion criteria, we selected 300 based on a study by Rashadat et al. (11). Participants were chosen at intervals of K = 2.85, rounded up to 3 (the result of dividing the total population by the sample population). An acceptable type 1 error of P = 0.05 and d = 0.06 was considered for determining the sample size.
The collected data were entered into SPSS version 25 and analyzed using descriptive statistics such as the mean and percentage. To compare the age and number of children between mothers who were aware and unaware of effective fever treatment and controls (based on the results of the Kolmogorov-Smirnov test), the Mann-Whitney test was used. Fisher’s exact test was used to compare the education levels between the two groups. Frequency indices were used to prepare tables, which were made with Microsoft Word.
4. Results
4.1. Demographic Findings
In this study, 300 mothers of children with fever who had visited the hospital were included. The average age of the mothers was 49.7 ± 0.30 years, and the average age of the febrile children was 2.2 ± 6.6 years. Most of the mothers had a diploma (36%), 12% were illiterate, and approximately 25% had less than a diploma. Only 4% had a post-diploma, and approximately one-sixth had a bachelor's degree. A postgraduate degree was reported by 3% of the mothers.
4.2. Main Outcome: Fever Prognosis
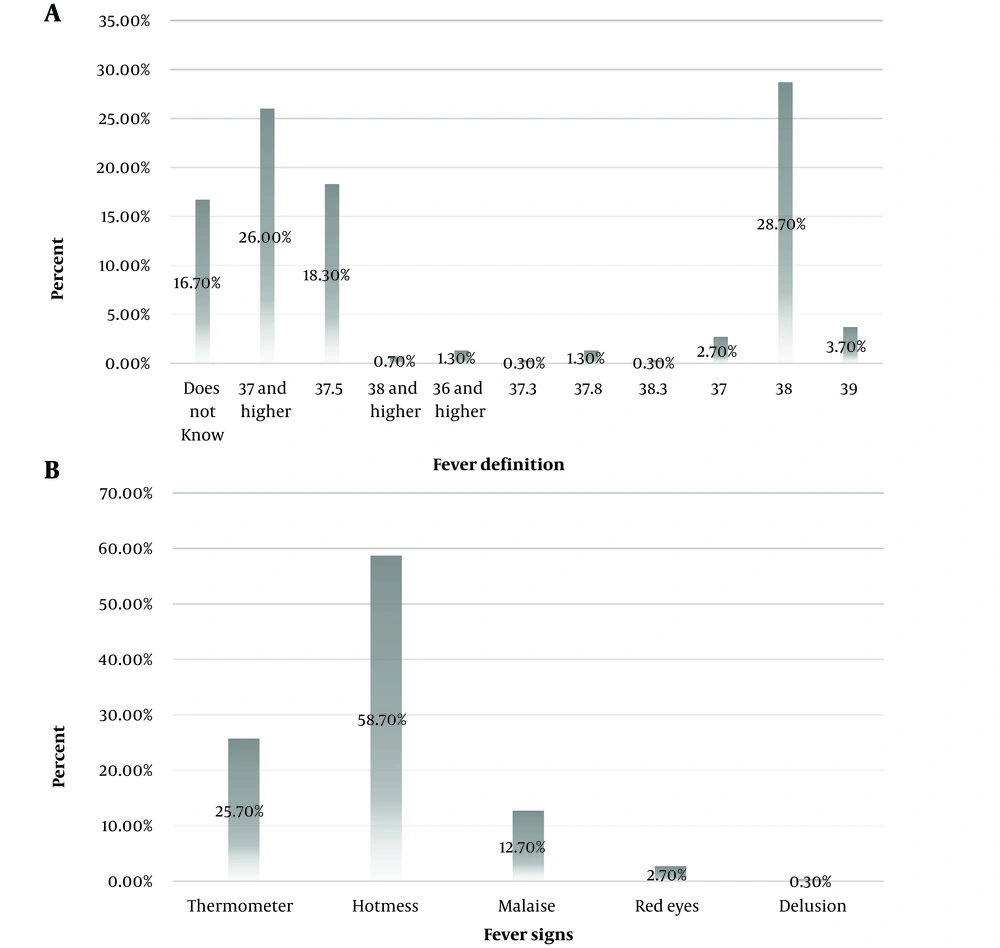
Sixteen percent of mothers did not know what temperature constitutes a fever, and approximately 28% considered a temperature of 38°C to indicate a fever. Twenty-six percent considered a temperature of 37°C or higher to indicate a fever, and approximately 18% considered a temperature of 37.5°C to indicate a fever. Only 1% of the participants considered a temperature of 36°C or higher to indicate a fever, while less than 1% thought that a temperature higher than 38°C was a fever. A temperature of 39°C was also considered to indicate a fever by some participants. However, slightly more knew that a fever was present at a temperature between 37°C and 38°C. More than half of the participants reported recognizing fever through body warmth, while 25% used a thermometer. Approximately 12% noticed fever by observing their child's fatigue, and less than 3% considered redness in their child's eyes. Only one mother thought her child had a fever because of hallucinations (Figure 1).
Approximately half of the mothers had a thermometer at home, and 95% of them used it to measure their child's temperature. Twenty-two percent of all mothers used only a mercury thermometer, and 29% used a digital thermometer. A total of 48% of all mothers did not use a thermometer. Most mothers (approximately 71%) knew how to use axillary measurements, which was more common than using oral measurements (26%). Skin, rectal, or tympanic measurements were used to measure fever in less than 1% of the total population.
The temperature considered as a fever by mothers’ definition (A), The temperature considered by the mothers was categorized, and approximately 16% of the mothers stated that they did not know. First sign of fever in children according to mothers; (B), Manifestations of fever were categorized based on mothers' statements; options other than thermometers meant that the first diagnosis of fever was based on these manifestations.
4.3. Main Outcome: Fever Primary Intervention
The first reaction of 69% of mothers was to use a footbath, while 30.7% of mothers immediately visited a doctor. The first action of only one mother (0.3%) was to use suppositories at home. Approximately one-fourth of the mothers did not have any knowledge about the appropriate antipyretic to use. Eighty-eight mothers used antipyretics according to the latest doctor's instructions. Additionally, 84 mothers administered antipyretics based on half their child's weight, while 23 mothers based it on doubling their child's weight. Thirty-one mothers administered a child-specific antipyretic regardless of their child's weight or fever.
A small percentage of mothers (approximately 5%) did not know the proper time interval for administering antipyretics. About half of the mothers stated that they used antipyretics every 6 hours, 35% every 4 hours, and just 5% every 8 hours. Less than 3% of the mothers stated that they used the drug every 12 hours, and one mother said that she used the antipyretic "as needed." Five percent of the participants had a history of seizures. A large majority (93%) of the mothers believed that if the fever is not treated, the child will have seizures, while 7% believed that the child would suffer from brain damage.
4.4. Main Outcome: Antipyretic Effect
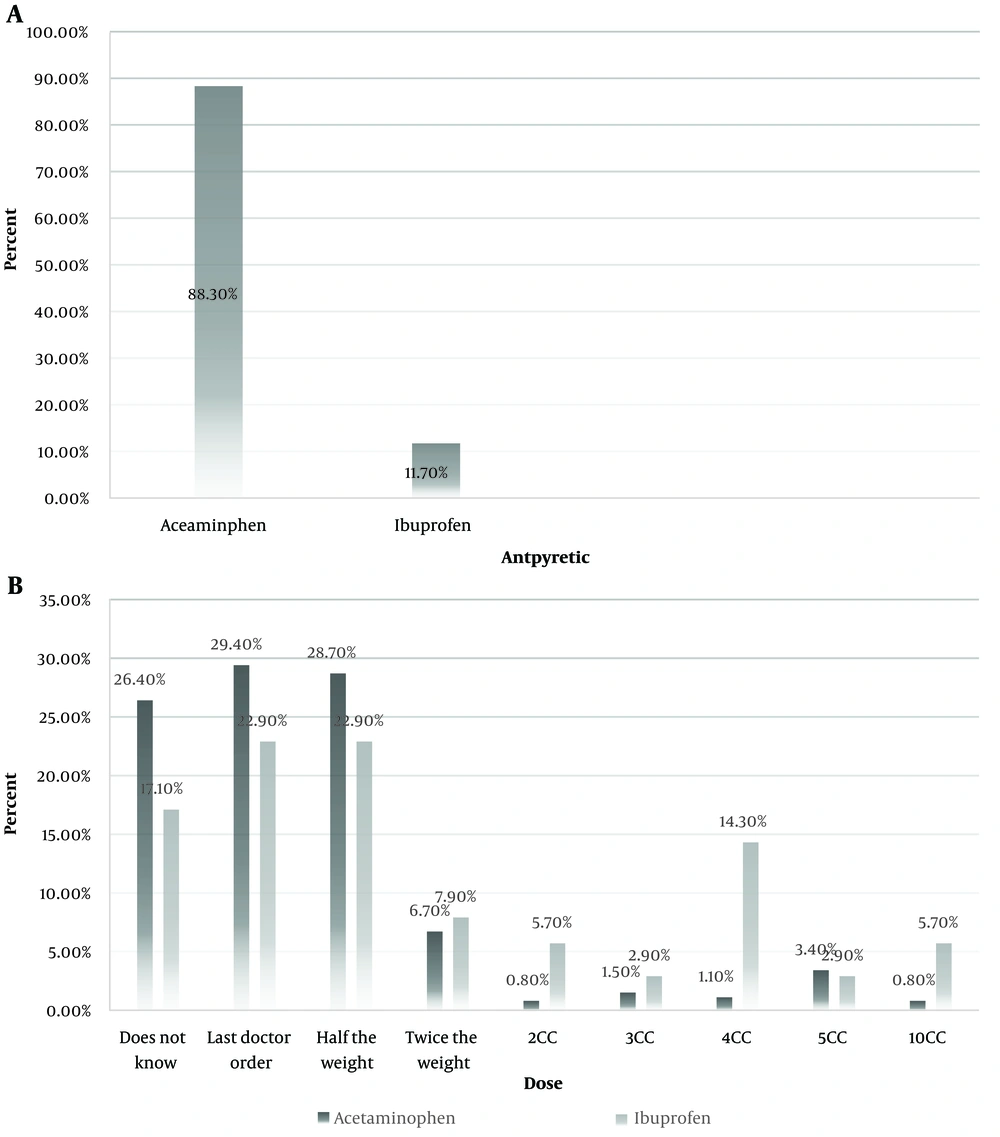
Acetaminophen was preferred by 88% of mothers, while 11% preferred ibuprofen as an antipyretic. A total of 4.26% of the mothers who reported using acetaminophen did not know the correct dosage. Some mothers followed the doctor's instructions for acetaminophen usage, while others gave only half the recommended dose based on their child's weight (Figure 2).
Preferable antipyretic medicine according to mothers (A), Mothers were using different brands, and after checking with a pediatric infectious specialist, we finally got acetaminophen and ibuprofen. Amount of antipyretic consumption by mothers according to the type of antipyretic; (B), The dosage of drugs used by mothers separately between these two drugs.
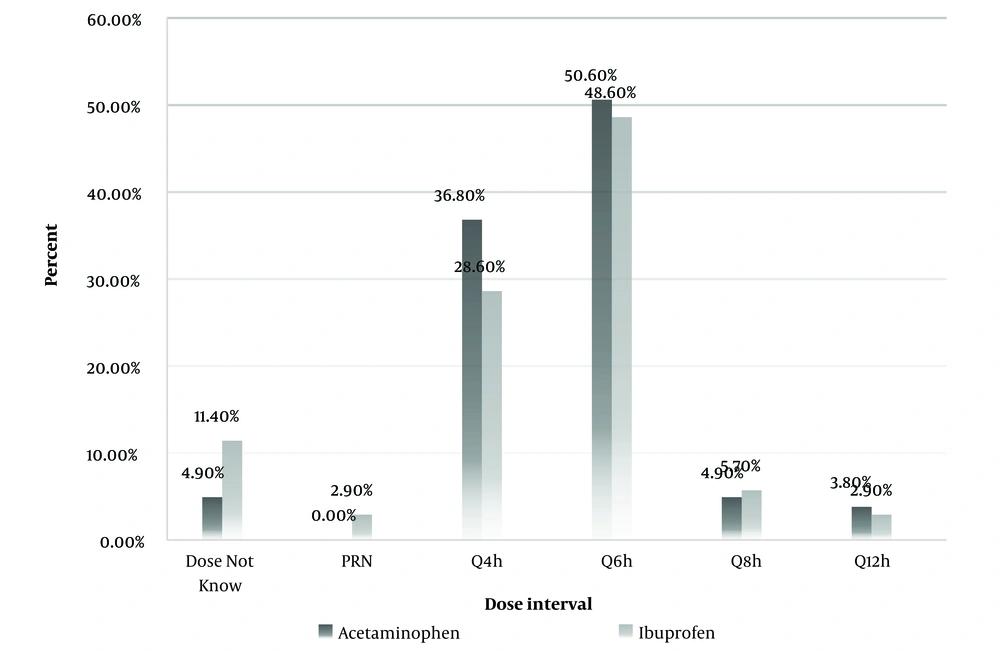
The majority of mothers administered acetaminophen every 6 hours, with only 8.35% giving it every 4 hours. A small percentage of mothers who reported ibuprofen as their preferred fever treatment knew the correct dosage. Less than one-fourth of the mothers used ibuprofen according to the latest doctor's orders, and only half the weight of their child. Most mothers who preferred ibuprofen used it every 6 hours, with 28.6% giving it to their child every 4 hours (Figure 3).
5. Discussion
Our study showed that most mothers considered a temperature of 38°C to indicate a fever, and 50 mothers did not know the exact temperature at which a fever occurs. This lack of knowledge appears to be directly related to their level of education. All mothers who were aware of effective fever treatment and control had a high school diploma or higher, and these mothers tended to be older on average. Many mothers who reported acetaminophen as their preferred antipyretic did not know the correct dosage. Furthermore, all the mothers believed that if a fever is not treated, the child would suffer seizures or brain damage.
The mothers included in this study generally lacked correct information on how to treat and care for a feverish child, with this issue being more prevalent among those with a lower level of education. The increasing concern among mothers was associated with their lack of knowledge, as our results showed that many mothers do not even have a correct definition of their child's fever.
Parental concerns about fever management practices have remained almost unchanged (12). Wan-Tsien Bong found that 72% of mothers experienced fever anxiety, and 12% were afraid that their children would die from a fever (13). Mothers need various forms of educational, emotional, and spiritual support to better manage their children's fevers. The reactions they show to fever and their level of awareness are influenced by their level of education. Bakry highlighted the importance of providing appropriate information to younger mothers, those with fewer children, higher education, sufficient income, and good knowledge of fever (14). While a lower average age and fewer children did not significantly influence our results, all mothers in our study met the minimum education requirement of a high school diploma.
Mothers' perceptions were related to their level of education, indicating that educated mothers are more likely to understand the relationship between fever and the presence of a pathogen in the body. A high percentage of mothers who were more aware of their condition believed that untreated fever leads to convulsions. Reducing fever and normalizing body temperature are the main approaches taken by parents, and body temperature is considered the primary indicator of disease severity (15). An increase in children's body temperature is a disease-related symptom, but most mothers do not measure their child's body temperature correctly.
More than half of the mothers in the Korkut study had a thermometer, but almost half of the population examined their child's fever by touch, and a few examined the appearance of their child (16). This pattern was consistent with our study, as most of our mothers used touch and body warmth, and 75% did not use a thermometer accordingly. Although understanding the importance of fever is directly related to education, the results showed that using a thermometer was not necessarily dependent on education. Even though using a thermometer was the most common method of diagnosis, detecting fever was still a challenge for mothers. In other words, only 18% of the participants considered a fever to be a temperature above 38°C, and just 4% considered a fever to be a temperature between 37°C and 38°C. This indicates that the method of diagnosing fever by mothers has been accompanied by incorrect information about the normal range of a child's body temperature (17).
The normal body temperature of children is considered to be between 37.2°C and 37.8°C (18). Fever was defined as an oral temperature above 37.8°C, a tympanic or rectal temperature of 38°C, and an axillary temperature above 37.2°C (4). Despite the high percentage of educated mothers in our study, approximately 16% did not know the normal range of temperature, and about half did not correctly know the desired temperature for fever. According to a study by Anokye, 71% of mothers used an axillary thermometer to measure their child's temperature, but only 22% considered a temperature above 37°C to indicate a fever (19). Mothers may have taken inappropriate action for fever treatment, as they considered temperatures less than 37°C to indicate fever (20). This means that a large percentage of mothers may have misdiagnosed fever (at 37°C) and used antipyretics incorrectly. In our study, 26.4% of mothers who reported acetaminophen as a preferred antipyretic did not know the exact dosage. Most of them used acetaminophen according to the doctor's last order, and it was half of the child's weight.
Self-medication and visiting the nearest hospital were the most common actions taken by mothers when their child experienced fever symptoms (19). Approximately 69% of mothers in the study used a wet cloth to lower their child's temperature, while only 1% were aware of and used suppositories for fever treatment at home. It is encouraging to see that, despite inadequate education, mothers prioritize physical methods over medication based on pediatricians' recommendations (6). However, knowledge of these physical methods may be limited regarding treating fevers.
Approximately one-fourth of mothers were unaware of the appropriate use of antipyretics, and even among those who were aware of the medication, 35% adjusted the dosage based on their child's weight, regardless of the type of medication. Only 30% of mothers followed the latest doctor's instructions for timely use of antipyretics, which indicates the need for better education on proper use. Approximately 5% of the mothers were not familiar with the exact duration of use, and 8% of the mothers used antipyretics every eight or twelve hours, whereas the most effective method is every 4 to 6 hours (21). Caring for a feverish child is a significant concern for parents because their knowledge, especially mothers', about the effectiveness and appropriateness of antipyretics is often questionable.
Ayatollahi introduced acetaminophen and ibuprofen as common drugs used by mothers (20). In our study, approximately 88% of mothers used acetaminophen, though about a quarter of them did not know how to use it correctly. This issue persisted for ibuprofen, with around three-quarters of mothers lacking complete knowledge of its proper use. Twenty-six percent of mothers using acetaminophen did not know the correct dosage, and only 28% used it based on the child's weight. Similarly, for 17% of mothers, the correct dosage of ibuprofen was unknown, and less than a quarter administered it based on half the child's weight (according to the latest doctor's instructions). Inaccurate information about antipyretics leads to their incorrect use, potentially threatening the child's health. Concerns can cause the use of inappropriate treatment and sometimes result in poisoning due to nonstandard drugs, leading to numerous visits to emergency wards (22, 23).
In summary, our results were consistent with previous findings and showed a significant correlation between mothers’ education levels and their knowledge of effective fever treatment and control. A large percentage of mothers in this study did not have accurate knowledge of how to treat and care for a child with a fever, particularly those with lower education levels. Many mothers did not know the correct information about antipyretic drugs, the proper dosage, and how to use them. This lack of knowledge makes managing children's health during fever treatment uncertain. If mothers are not properly informed about fever and fever reducers, they will not provide adequate care. Since fever in children is an important sign of infection and can lead to seizures, the importance of mothers' knowledge and their response to fever increases.
5.1. Conclusions
Diagnosing and managing children's fever heavily depends on mothers' education levels, as educated mothers are generally more aware of proper child care standards. There is a significant gap between mothers' awareness of the duration and dosage of antipyretics and the standard use of these drugs, which is highly concerning for child care. Increasing mothers' awareness is a critical issue in health and child care and should receive special attention. We recommend that a comprehensive program be organized to enhance mothers’ understanding of managing children's