1. Background
The arrival of a newborn child is an expected moment, and in the great majority of cases, it is presented as a source of happiness and hope for the future, both for individual families and for the community as a whole (1). However, the time of delivery and the first month are critical for child survival, as the risk of morbidity and mortality can increase considerably if complications emerge (2, 3). The first 28 days of life—the neonatal period—represent the most vulnerable time for a child's survival. Children face the highest risk of dying during their first month of life, with a global rate of 17 deaths per 1,000 live births. Globally, approximately 2.4 million newborns died during the first month of life in 2020, which is about 6,500 per day (4). In 2020, the United States experienced a neonatal mortality (NNM) rate of 3.4 per 1,000 live births. Europe and Central Asia recorded a mortality rate of 4.1 per 1,000 live births, Tunisia registered a rate of 11.8 per 1,000 live births, and Libya had a rate of six per 1,000 live births. However, in Morocco, NNM has decreased from 19.3 deaths per 1,000 live births for newborns in 2010 to 11.5 deaths per 1,000 live births in 2020 (5). Children who die within the first 28 days of life exhibit conditions and illnesses linked to the lack of quality care at birth or the absence of care or treatment provided by skilled personnel immediately after birth and in the early days of life (6). Furthermore, approximately one-third of all neonatal deaths occur on the first day after birth, and nearly three-quarters occur during the first week of life (4). In 2018, Northern Africa had the highest NNM rate at 28 deaths per 1,000 live births (7). Moreover, the NNM rate in Morocco was 13.6% in 2018 (8) and 11.1% in 2021 (9). For in-hospital NNM, a rate of 19% was reported (10), and early NNM was estimated at 21.4% (11). Prematurity, low birth weight, neonatal infections, and neonatal distress are the main factors of morbidity and the leading causes of death among newborns, with neonatal asphyxia being the primary cause (12). Regarding in-hospital NNM, neonatal infections are the leading cause of death, followed by neonatal respiratory distress and perinatal asphyxia. Prematurity emerges as the primary predisposing factor (13). The burden of NNM and morbidity remains high, and the opportunities to enhance women's well-being and provide attentive care to newborns have not been fully exploited (14). In summary, each newborn is a roadmap that outlines the path to ending preventable NNM and reducing disabilities (15).
2. Objectives
The aim of this study was to identify factors associated with NNM in the Neonatology Unit at the Regional Center of Agadir and to estimate its prevalence.
3. Methods
This was an analytical cross-sectional study focused on deceased newborns recorded at the Neonatology and Intensive Care Unit of Hassan II Regional Hospital in Agadir. The study was conducted over the period from January 1, 2018, to July 31, 2021. It is a level II reference neonatal intensive care center in the Souss-Massa region. It receives and provides care for newborns who have health problems after birth and who are referred from the regional maternity ward, provincial hospitals, birthing centers, and clinics in the city of Agadir and neighboring regions. The facility has a capacity of 18 beds, along with 10 warming tables and five self-priming syringes.
The study population consists of newborns who were hospitalized and deceased at the neonatology unit of the Agadir Regional Hospital. The sample size was estimated using the sample size estimation formula for prevalence studies (16, 17). The required sample size calculation was based on the actual prevalence of in-hospital NNM (19%) (10) and the national prevalence of NNM of 11.1 per 1,000 live births (9), using a significance level of 5% (i.e., α = 0.05) with a study power of 80%. Subsequently, a minimum of 108 deceased newborns were required to obtain statistically representative data. The selection of records to be included was done randomly from the death registers, applying the simple random sampling method. All newborns who died in the Neonatology Unit at the Agadir Regional Hospital during the study period were included. The study excluded any newborns who were discharged alive from the Neonatology Unit and children who were hospitalized and died after 28 days of age. To avoid bias, the measuring instrument was tested on a small sample of files excluded following random sampling.
The criteria for judgment were NNM, which is defined as death occurring within the first 28 complete days of life (9, 15, 18). It was categorized as early deaths during the first week and late deaths during the subsequent three weeks (19). The modes of use of hospital services and benefits were: (1) ordinary admission—any scheduled hospitalization outside of emergencies; (2) emergency admissions (emergency consultations, transfers, and intra-hospital referrals) (20).
The tool used for data collection was an exploitation form of medical records and hospitalization registers, which was designed and selected based on a literature review. This exploitation form was developed using Sphinx software and included open-ended and multiple-choice questions aimed at exploring several aspects: (a) neonatal (age, gender, weight, hospitalization diagnosis, etc.); (b) maternal (mother's age, place of origin, etc.); and (c) obstetric (place and method of delivery, etc.).
The collected data were analyzed using Jamovi V21 software. Firstly, a descriptive analysis was performed, and the qualitative variables were expressed as frequency and percentages; the quantitative variables were expressed as medians and interquartile ranges. The distribution of quantitative variables was assessed based on graphical representations, including histograms, Q-Q plots, and the Shapiro-Wilk test. The assessment of associations was conducted using the chi2 test or Fisher's exact test, according to the conditions of application for each test. To determine factors associated with early NNM, binary logistic regression was employed in both univariate and multivariate analyses; all variables with P ≤ 0.05 in the univariate analysis were included in the multivariate model. The odds ratios (OR) were calculated with a 95% confidence interval (95% CI). The significance level was set at P ≤ 0.05.
The Ethics Committee of the Faculty of Medicine and Pharmacy of Rabat approved this study with reference number (C64-20). The study strictly adhered to ethical considerations, including (a) obtaining authorization for access to records from the responsible administration; (b) preserving anonymity; (c) confidentiality; and (d) professional secrecy.
4. Results
4.1. Neonatal Mortality Rate
The NNM rate at the Hassan II Regional Hospital in Agadir was 17.44%, 95% CI (13.2-21.7), for the period from 2018 to 2021. Among the newborns who died in the Neonatology Unit at CHR Hassan II in Agadir during the study duration, there were 1,535 cases, while the hospitalized newborns totaled 8,802.
4.2. Demographic and Clinical Characteristics
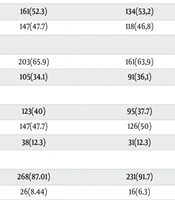
A total of 308 deceased neonates were included in the study; early NNM accounted for 81.81%. The median length of hospitalization was 1 [1-1] day, with 95.45% being hospitalized during their first week of life, of which 97% died during the early neonatal period. 52.3% of the deceased were from rural areas. There was a predominance of females, with a percentage of 52.3% compared to 47.7% for males. As for the median weight, it was 2200 (1450 – 3200) grams (g), with 47.7% of cases having low birth weight, and 50% of them lost their lives during the early neonatal period. 43.7% of the deaths during the early neonatal period were from intra-hospital referrals, 31.7% were transfers, and 17.2% were admitted through the emergency department.
The median Apgar score was 7 [6-8]. 65.9% of cases had an Apgar score less than 7 at the 5th minute after birth, of which nearly 64% were classified as early NNM. The main diagnoses for hospitalization of newborns who died in the neonatal unit were prematurity (59.7%), neonatal distress (14.3%), convulsions (5.8%), malformation (4.3%), jaundice (2.9%), and neonatal infection (1%). (Table 1). The types of malformations were distributed as follows: 8 (32%) neural tube defects, 4 (16%) multiple malformations, 2 (8%) cardiac malformations, and abdominal, ocular, and genital malformations, each recorded at a frequency of 1 (4%). However, 8 (32%) of malformation types were not specified. 85.7% were born to women aged between 20 and 35 years. 72.4% of cases were born in a hospital maternity ward, followed by 25.6% born in a private clinic. Only 1.3% and 0.6% were born at home and in a birthing center, respectively. 65.3% of cases were from singleton pregnancies, 30.8% from twin pregnancies, and only 3.9% from multiple pregnancies (Table 1).
| Variables | Total a; N = 308 | Early NNM; n = 252 | Late NNM; n = 56 | P-Value |
|---|---|---|---|---|
| Sex | 0.501 b | |||
| Female | 161 (52.3) | 134 (53.2) | 27 (48.2) | |
| Male | 147 (47.7) | 118 (46.8) | 29 (51.8) | |
| Apgar 7 [6-8] c | 0.113 b | |||
| < 7 | 203 (65.9) | 161 (63.9) | 42 (75) | |
| ≥ 7 | 105 (34.1) | 91 (36.1) | 14 (25) | |
| Birth weight 2200 [1450 - 3200] c | 0.198 b | |||
| Normal | 123 (40) | 95 (37.7) | 28 (50) | |
| Low birth weight | 147 (47.7) | 126 (50) | 21 (37.5) | |
| Overweight | 38 (12.3) | 31 (12.3) | 7 (12.5) | |
| Neonatal age at admission 1[1-1] c | < 0.001 d | |||
| ≤ 1 jr | 268 (87.01) | 231 (91.7) | 33 (58.9) | |
| 2 - 7 | 26 (8.44) | 16 (6.3) | 9 (16.1) | |
| > 7 | 14 (4.55) | 5 (2) | 14 (25) | |
| Mode of admission | < 0.001 b | |||
| Ordinary | 28 (9.1) | 17 (6.7) | 11 (19.6) | |
| Emergency consultations | 53 (17.2) | 45 (17.9) | 8 (14.3) | |
| Intra-hospital referral | 122 (39.6) | 110 (43.7) | 12 (21.4) | |
| Transfer | 105 (34.1) | 80 (31.7) | 25 (44.6) | |
| Origin | 0.206 b | |||
| Rural | 161 (52.3) | 136 (54) | 25 (44.6) | |
| Urban | 147 (47.7) | 116 (46) | 31 (55.4) | |
| Type of pregnancy | 0.536 b | |||
| Singleton | 201 (65.3) | 161 (63.9) | 40 (71.4) | |
| Twin | 95 (30.8) | 81 (32.1) | 14 (25) | |
| Multiple | 12 (3.9) | 10 (4) | 2 (3.6) | |
| Place of delivery | 0.717 d | |||
| Private clinic | 79 (25.6) | 62 (24.6) | 17 (30.4) | |
| Hospital maternity ward | 223 (72.4) | 184 (73) | 39 (69.6) | |
| Birth center | 2 (0.6) | 2 (0.8) | 0 | |
| At home | 4 (1.3) | 4 (1.6) | 0 | |
| Maternal age | 0.555 d | |||
| ≤ 20 | 17 (5.5) | 13 (5.2) | 4 (7.1) | |
| > 20 - 35 | 264 (85.7) | 215 (85.3) | 49 (87.5) | |
| > 35 | 27 (8.8) | 24 (9.5) | 3 (5.4) | |
| Prematurity | 0.05 b | |||
| Yes | 184 (59.7) | 157 (62.3) | 27 (48.2) | |
| No | 124 (40.3) | 95 (37.7) | 29 (51.8) | |
| Neonatal infection | 0.086 d | |||
| Yes | 3 (1) | 1 (0.4) | 2 (3.6) | |
| No | 305 (99) | 251 (99.6) | 54 (96.4) | |
| Neonatal distress | 0.398 b | |||
| Yes | 44 (14.3) | 38 (15.1) | 6 (10.7) | |
| No | 264 (85.7) | 214 (84.9) | 50 (89.3) | |
| Seizure | 0.752 d | |||
| Yes | 18 (5.8) | 14 (5.6) | 4 (7.1) | |
| No | 290 (94.2) | 238 (94.4) | 52 (92.9) | |
| Malformation | 0.759 d | |||
| Yes | 19 (6.2) | 15 (6) | 4 (7.1) | |
| No | 289 (93.8) | 237 (94) | 52 (92.9) |
Abbreviations: NNM, neonatal mortality; ds, days.
a Expressed in numbers (percentage).
b Chi2 test.
c Expressed in median and interquartile ranges.
d Fisher's exact test.
The results from Table 1 indicated a statistically significant difference in the frequency of neonatal admission age (P < 0.001), mode of admission (P < 0.001), and prematurity (P = 0.052) between early NNM and late NNM.
4.3. Factors Associated with Early Neonatal Mortality
In univariate analysis, the factors associated with early NNM were APGAR (cOR: 0; 95% CI: 6.62 - 57.96); admission age ≤ 1 day (cOR: 19.6; 95% CI: 6.62 - 57.96); neonatal admission age 2 - 7 days (cOR: 4.94; 95% CI: 1.34-18.40); emergency consultations (cOR: 3.64; 95% CI: 1.25 - 10.59); intra-hospital referral (cOR: 5.93; 95% CI: 2.26 - 15.56). However, the other factors studied in the univariate analysis (Table 2) were not significantly associated with early NNM (P > 0.05).
| Variables | Analyze Univariate | Analyze Multivariate | ||||
|---|---|---|---|---|---|---|
| cOR | IC 95% | P-Value | aOR | IC 95% | P-Value | |
| Sex | ||||||
| Female | 1.22 | 0.68 - 2.18 | 0.502 | - | - | - |
| Male | 1 | 1 | - | - | - | - |
| Apgar | ||||||
| < 7 | 0.590 | 0.30 - 1.14 | 0.115 | - | - | - |
| ≥ 7 | 1 | 1 | - | - | - | - |
| Birth weight | ||||||
| Low birth weight | 1.77 | 0.94 - 3.30 | 0.074 | - | - | - |
| Overweight | 1.31 | 0.51 - 3.28 | 0.571 | - | - | - |
| Normal | 1 | 1 | - | - | - | - |
| Neonatal age at admission | ||||||
| ≤ 1jrs | 19.6 | 6 .62 - 57.96 | < 0.001 | 17.87 | 5.78 - 55.29 | < 0.001 |
| 2 - 7 jrs | 4.978 | 1.34 - 18.40 | 0.016 | 6.64 | 1.68 - 26.30 | 0.007 |
| > 7jrs | 1 | 1 | - | - | - | - |
| Origin | ||||||
| Rural | 1.45 | 0.81 - 2.60 | 0.208 | - | - | - |
| Urban | 1 | 1 | - | - | - | - |
| Mode of admission | ||||||
| Emergency consultations | 3.64 | 1.25 - 10.59 | 0.018 | 4.25 | 1.28 - 14.01 | 0.017 |
| Intra hospital referral | 5.93 | 2.26 - 15.56 | < 0.001 | 4.49 | 1.59 - 12.65 | 0.004 |
| Transfer | 2.07 | 0.20 - 1.16 | 0.106 | - | - | - |
| Ordinary | 1 | 1 | - | - | - | - |
| Type of pregnancy | ||||||
| Twuin | 1.44 | 0.74 - 2.79 | 0.285 | - | - | - |
| Multiple | 1.24 | 0.26 - 5.89 | 0.785 | - | - | - |
| Singleton | 1 | 1 | - | - | - | - |
| Place of delivery | ||||||
| Private clinic | 0.773 | 0.40 - 1.46 | 0.429 | - | - | - |
| Birth center | 3.32e+6 | 0.00 - inf | 0.993 | - | - | - |
| At home | 3.32e+6 | 0.00 - inf | 0.990 | - | - | - |
| Hospital maternity ward | 1 | 1 | - | - | - | - |
| Maternal age | ||||||
| ≤ 20 | 0.741 | 0.23 - 2.37 | 0.613 | - | - | - |
| > 35 | 1.823 | 0 .52 - 6.30 | 0.342 | - | - | - |
| 20 - 35 | 1 | 1 | - | - | - | - |
| Prematurity | 1.78 | 0.99 - 3.18 | 0.054 | - | - | - |
| Neonatal infection | 0.108 | 0.009 - 1.21 | 0.071 | - | - | - |
| Neonatal distress | 1.48 | 0.59 - 3.69 | 0.401 | - | - | - |
| Seizure | 0.765 | 0.24 - 2.42 | 0.648 | - | - | - |
| Malformation | 0.823 | 0.26 - 2.58 | 0.738 | - | - | - |
Abbreviations: cOR, crude odds ratio; aOR, adjusted odds ratio; CI, confidence interval.
After adjusting for the following factors: Neonatal age, mode of admission, jaundice, and length of hospitalization, the factors that were statistically associated with the risk of early NNM were as follows: Newborns admitted during the ultra-early neonatal period (age ≤ 1 day) had a risk multiplied by 17 of death (aOR: 17.87; 95% CI: 5.78 - 55.29). In addition, those admitted during the early neonatal period (2 - 7 days) had a risk 6 times higher of death (aOR: 6.64; 95% CI: 1.68 - 26.30). Intra-hospital referral increases the risk of death by 4 times (aOR: 4.49; 95% CI: 1.59 - 12.65). Newborns admitted via the emergency department had a 4-fold increased risk of death (aOR: 4.25; 95% CI: 1.28 - 14.01) (Table 2).
5. Discussion
Through the reported results, the present study attempted to identify the factors associated with NNM and to estimate its prevalence. Newborns are the most vulnerable population group in the world due to their specific needs; consequently, they serve as a sensitive indicator of the quality of services provided, as they can die within a few days (21). The NNM rate at Hassan II Regional Hospital in Agadir is 17.44%, 17.44% (95% CI: 13.2 - 21.7) for the period from 2018 to 2021. This rate remains significant compared to that recorded at the reference hospital in Kindu, where the hospital NNM rate was 15% (22). However, it is lower than the NNM rates reported by studies conducted in Meknes and in the South Kivu province of Congo, 19% and 26.6%, respectively (10, 23). The main diagnoses for hospitalization of newborns who died in the neonatal unit were prematurity (59.7%), neonatal distress (14.3%), convulsions (5.8%), malformation (4.3%), jaundice (2.9%), and neonatal infection (1%). WHO declared that premature birth, birth asphyxia, infections, and birth defects are the main causes of neonatal death (6).
Birth weight is a good indicator to enhance the chances of a newborn's survival. Low birth weight and overweight are considered risk markers, with low birth weight predominating in our sample (47.7%), and 50% of them lost their lives during the early neonatal period. In this regard, Ilunga et al. state that there is a relationship between birth weight and mortality. The lower the birth weight, the higher the mortality rate (24). The findings of Nouria et al. revealed that 84.27% of deceased newborns had low birth weight (25). In light of these results, new studies on all parameters associated with low birth weight are necessary to monitor the ongoing evolution of this issue and its recurrent associated factors (26). The Apgar score is the first test that a newborn undergoes at birth. It provides an idea of the newborn's adaptation to extrauterine life, its circulatory functions, as well as its neurological condition. In France, a study on NNM reported that newborns with a very low Apgar score had an earlier age of death (27). This is consistent with the data from our series. The median Apgar score was 7 [6-8], with 65.9% of cases having an Apgar score less than 7 at the 5th minute of birth, of which nearly 64% were classified as early NNM.
The results of our study identified four factors significantly associated with the risk of early NNM: Admission age ≤ 1 day (aOR: 17.87; 95% CI: 5.78 - 55.29); neonatal admission age 2 - 7 days (aOR: 6.64; 95% CI: 1.68-26.30); emergency consultations (aOR: 4.25; 95% CI: 1.28 - 14.01); intra-hospital referral (aOR: 4.49; 95% CI: 1.59 - 12.65).
The age of hospitalization provides insight into the alarming age of newborns as well as the delicate stage after birth and reflects the early onset of a serious medical condition. In our series, 95.45% were hospitalized during the early neonatal phase, with 98% of them dying during the early neonatal period. Additionally, the multivariate analysis is statistically significant, showing an association between the age of hospitalization and early NNM for admission age ≤1 day (aOR: 17.87; 95% CI: 5.78 - 55.29), and neonatal admission age 2 - 7 days (aOR: 6.64; 95% CI: 1.68 - 26.30). This is consistent with the study by Feirouz et al., which reported that the NNM rate is very high during the early neonatal period, with 15% occurring on the first day of life and 60% dying beyond 48 hours of life (28). Similarly, Kedy Koum et al. and Garba et al. reported hospital NNM rates of 97.1% and 63.21%, respectively, during the early neonatal period (29, 30). More than half of the births, even more, conclude with death within the first 24 hours of life, and 75% within the first week of life (31). However, the study by Zoungrana-Yameogo et al. reported that the median age of death was 2 [1-5] days and the probability of survival at the seventh day of birth was 77% (32). This similarity with other studies could be explained by the fact that the early neonatal period is very critical, as almost two-thirds of these deaths occur in this period, and to reduce early NNM, it is imperative to reduce NNM.
The probability of death occurrence was multiplied by 2.1 among newborns born to referred mothers [aOR = 2.11; (1.12 - 3.99)] (33); this implies that each level of care facility should be able to immediately provide essential care for survival, with the required skills and equipment to stabilize a newborn and safely facilitate transfer if necessary (21). In this context, the present study found a statistically significant association between mode of admission and the risk of early NNM: Emergency consultations (aOR: 4.25; 95% CI: 1.28 - 14.01); intra-hospital referral (aOR: 4.49; 95% CI: 1.59 - 12.65). In comparison with a study at the Douala referral hospital, where NNM was higher among referrals from healthcare facilities other than the maternity unit, compared to those referred from the maternity unit (29). In contrast, in the study by Mouahid et al., one-fifth of the deceased were transferred from another facility (10). This suggests a qualitative approach to understanding why these preventable deaths occur and how they are related to social determinants on one hand, hospital care provided on the other, and the skill and motivation of health staff on the third (33).
This study reported ultra-early age, early age, intra-hospital referral, and transfer as factors associated with the risk of early NNM. Nevertheless, this study had certain limitations. The retrospective nature of our study, based on data from hospital records and registers, meant that a large amount of data was missing due to the under-notification of data, in particular socio-demographic, clinical, medical, and obstetrical data on the mothers of newborn babies. Given the high proportion of missing data for these variables, they were not investigated in our study. Otherwise, the dearth of information was also a limitation in this study, resulting in a difference between our results and those of other studies. To strengthen our findings, we recommend similar prospective research involving all the obstetric and neonatal teams over a longer period, with a comparison of the results with some regional and international studies.
5.1. Conclusions
Neonatal mortality is an indicator of population health. It represents a significant health challenge worldwide, particularly in developing countries where rates of NNM are predominant, such as the NNM rate at Agadir hospital, which remains high. The results of the present study highlight the need to strengthen efforts to eliminate preventable deaths and bring about significant changes in the field of maternal and child health. This can be achieved through better monitoring of pregnancy and ensuring early diagnosis, monitoring and surveillance of pregnancy, screening and management of high-risk pregnancies, better monitoring of delivery, good management of childbirth, promoting intrauterine transfer, and improving transfer conditions. Additionally, quality care for small and sick newborns is essential.