1. Introduction
Septic arthritis refers to an infection in the synovial fluid and joint tissue. Children with acute septic arthritis may experience serious consequences, such as joint destruction, soft tissue damage, and osteonecrosis, if not diagnosed and treated promptly (1). Symptoms typically include joint pain, fever, and difficulty bearing weight (2). Inflammatory markers are elevated, and ultrasound may reveal joint effusion. The Kocher criteria can aid in distinguishing between septic arthritis and transient synovitis in children with hip pain. One point is assigned for each of the following four criteria: Inability to bear weight on the affected side, erythrocyte sedimentation rate > 40, fever > 38.5°C, and white blood cell count > 12 000. The likelihood of septic arthritis increases with the presence of more criteria, with a probability exceeding 93% when all four criteria are met (3, 4).
Kawasaki disease (KD) is a febrile, multiorgan vasculitis affecting young children, the etiology of which remains unknown. First described by Tomisaku Kawasaki in Japan in 1967, (5) the main symptoms of KD include fever, bilateral nonexudative conjunctivitis, erythema of the lips and oral mucosa, changes in the extremities, skin rash, and cervical lymphadenopathy. Up to 25% of untreated children may develop coronary artery abnormalities and subsequent complications such as ischemic heart disease, myocardial infarction, or sudden death (6).
We report a case of a 6.5-year-old boy with highly suspected septic arthritis and incomplete KD, presenting with hip pain in both hips.
2. Case Presentation
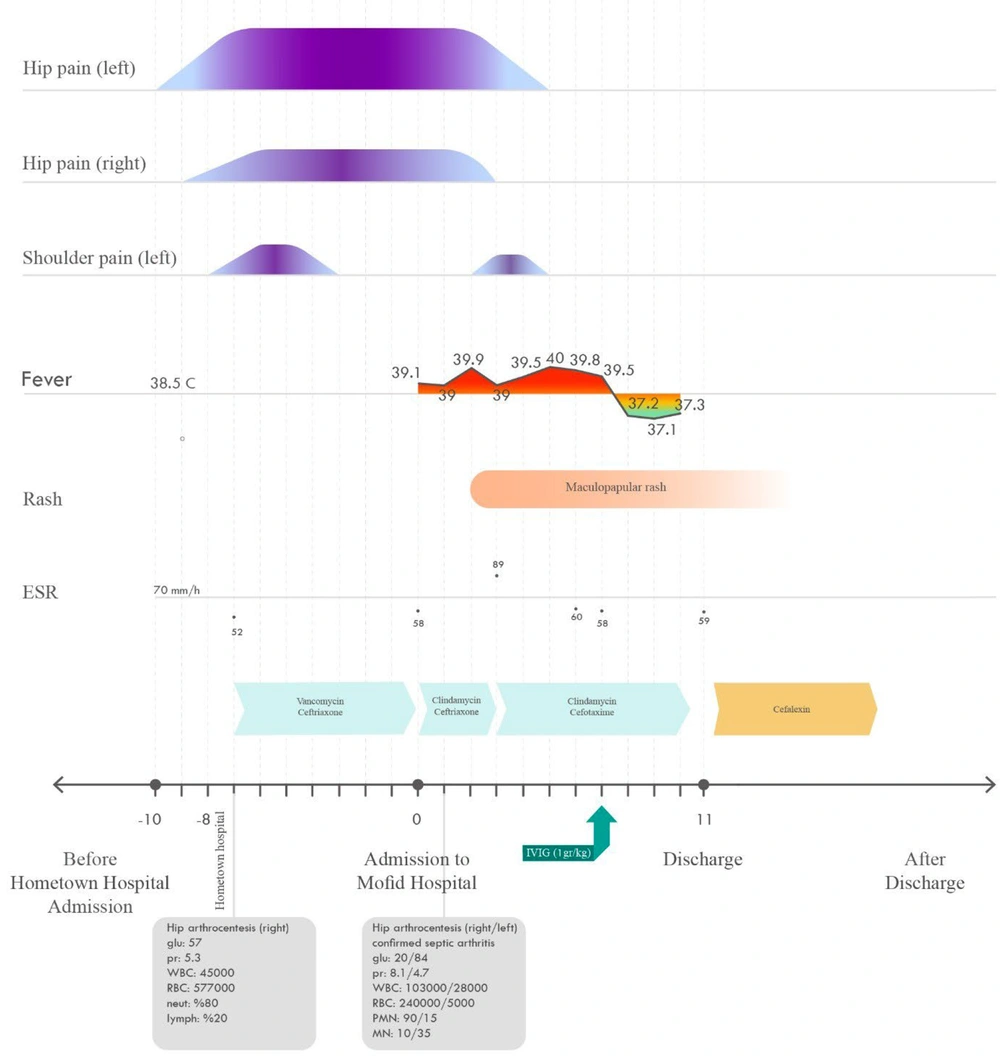
A 6.5-year-old boy, who had been experiencing pain in both hip joints for the past 10 days, was referred to Mofid Children's Hospital in Tehran from a hospital in his hometown. He reported a history of fever and mild pain in the left shoulder, which had resolved before referral. Azithromycin and dexamethasone were prescribed on the day his symptoms began, but because the pain only subsided for one day before worsening again, he was admitted to a hospital in his hometown approximately 3 days after symptom onset. The requested studies conducted at that center are listed in Table 1. His hip ultrasound at the center revealed synovial thickening and effusion in the right hip joint and synovial thickening without effusion in the left hip joint. Arthrocentesis of the left hip joint was also performed, the results of which are shown in Figure 1 (7). He received intravenous vancomycin and ceftriaxone. After 6 days, he was transferred to Mofid Center. At the time of admission to this center, he did not have a fever.
| Parameter | Hometown Hospital | Admission Day | 3 Days Later | 1 Week Later |
|---|---|---|---|---|
| WBC | 15 900 | 15 300 | 15 500 | 8 500 |
| Neutrophil, (%) | 75 | 80 | 64 | 69 |
| Lymphocyte, (%) | 22 | 17 | 28 | 23 |
| Hemoglobin | 14.6 | 15.3 | ||
| Platelet | 403 000 | 455 000 | 423 000 | |
| Erythrocyte sedimentation rate (ESR) | 52 | 58 | 89 | 60 |
| C-reactive protein (CRP) | 47 | 2+ | ||
| Alanine aminotransferase (ALT) | 83 | 171 | 72 | |
| Aspartate aminotransferase (AST) | 45 | 31 | ||
| Lactate dehydrogenase (LDH) | 441 | |||
| Antistreptolysin-O (ASO) | < 100 | < 200 | ||
| Wright and 2ME | Negative |
The parents did not report any recent infections or trauma to the affected area, and the patient had not consumed any local dairy products (Iran is endemic for Brucellosis). Additionally, there was no remarkable family history. The patient weighed 25 kg and experienced malaise but had no complaints of nausea, vomiting, diarrhea, or dysuria. Physical examination revealed pain and tenderness in both hips, although there were no signs of erythema or swelling in the hip areas. Range of motion could not be assessed in the left hip due to severe pain, and weight bearing was disrupted on both sides. His ear, nose, and throat exams, lung exam, and echocardiography were normal, and there were no signs of lymphadenopathy. He developed a mild fever (38.1°C) on the day of admission.
A series of studies were requested, with results indicating an erythrocyte sedimentation rate (ESR) of 52, C-reactive protein (CRP) of 47, blood urea nitrogen (BUN) of 14, Cr of 0.6, white blood cell (WBC) of 15.9, neutrophil of 75, lymphocyte of 22, Hb of 14.6, CPK of 37, and U/A revealing WBC of 2 - 3, and red blood cell (RBC) of 2 - 3. His echocardiography showed normal results.
Considering that he met three out of four Kocher criteria—leukocytosis of 15 300, elevated ESR (58), and disrupted weight bearing in the hip joints—and arthrocentesis was performed one day after admission. Although his synovial culture came back negative, the synovial fluid analysis showed a highly suspected septic arthritis pattern in the right hip and a sympathetic inflammatory pattern in the left hip, indicative of possible septic arthritis on the other side.
Upon admission, his fever persisted. The course of his fever is illustrated in Figure 1. On the second day of admission, erythema of the lips and oral mucosa, as well as maculopapular rashes over his whole body, appeared.
He received apotel for his fever, along with ceftazidime, cefotaxime, ceftriaxone, clindamycin, linezolid, and azithromycin, but the fever did not respond to these medications. Based on clinical signs, symptoms, and laboratory results, a diagnosis of incomplete KD was made, and he received intravenous immunoglobulin (IVIG) (2 g/kg) on the seventh day of fever. Rapid resolution of fever and all symptoms occurred with IVIG treatment. He was discharged on oral antibiotics and aspirin.
3. Discussion
The cause of KD remains unknown, but its clinical and epidemiological features suggest an infectious agent (8). Patients with KD exhibit a clinical presentation similar to those with viral or superantigenic diseases. However, research indicates that the immune response in KD is oligoclonal, meaning it responds to a common antigen rather than polyclonal, (9, 10) as seen in antigen-based responses. Over the years, various infectious agents have been suggested, but none have been identified as the primary cause. It is also possible that multiple infectious agents provoke a shared inflammatory pathway leading to KD in vulnerable individuals (11). A plausible explanation is that KD may be caused by an infection that triggers an inappropriate immune response in a small subset of genetically susceptible children (12, 13).
We report a rare case of incomplete KD triggered by septic arthritis, wherein timely administration of IVIG resulted in clinical improvement and may have prevented cardiac complications. In this patient, arthritis was observed in multiple joints. Physical examination, imaging findings of the hip joints, blood tests, and synovial fluid cell pattern support a diagnosis of septic arthritis in the right hip and sympathetic arthritis in the left hip. Initially diagnosed with septic arthritis, the patient was treated with antibiotics. However, on the second day of treatment, despite improvement in articular symptoms, the patient's fever, which had initially decreased, increased again and did not respond to antibiotics. The diagnosis of KD was not initially considered due to the likelihood of other bacterial or viral causes for the fever, which were ruled out. The patient's fever persisted for five days, during which he developed a maculopapular rash on his body surface in addition to obvious redness of the lips and oral mucosa.
Despite consultation with infectious disease specialists and the prescription of appropriate antibiotics, the patient's fever persisted for 5 days, accompanied by two main clinical features of Kawasaki syndrome: Skin rashes and redness of the lips and oral mucosa. Consequently, the possibility of incomplete Kawasaki syndrome was considered. Blood test results revealed an elevated ESR above 40, a white blood cell count exceeding 15 000, platelet levels above 450 000, and elevated liver enzyme (ALT) levels above 50. According to guidelines related to incomplete Kawasaki syndrome, the patient was diagnosed with KD, and IVIG treatment was initiated (14).
Within 24 hours of starting IVIG, the patient's fever subsided, and his overall condition significantly improved. His condition was diagnosed as incomplete Kawasaki syndrome triggered by septic arthritis. Given that KD may be associated with coronary arteritis, coronary aneurysms, and thrombotic occlusion of coronary arteries, timely diagnosis is crucial. Appropriate treatment with IVIG can greatly reduce the risk of cardiac complications, as well as morbidity and mortality associated with the disease. In conclusion, recognizing the potential role of septic arthritis in triggering KD is essential (15).