1. Background
Infection control is of paramount importance in any healthcare setting, but it becomes even more critical in children's hospitals (1). The vulnerability of young patients to infections necessitates a strong commitment from healthcare workers (HCWs) to ensure a safe and healthy environment (2). This article explores the significance of infection control commitment among HCWs in children's hospitals and highlights the measures undertaken to protect the well-being of their young patients (1, 2).
Improper utilization of personal protective equipment (PPE), along with other issues related to PPE, can increase the likelihood of healthcare-associated infections among HCWs due to self-contamination (3). Some studies have indicated that nurses demonstrate a higher degree of compliance with infection control protocols compared to other HCWs (3-5). However, it should be noted that, according to the World Health Organization (WHO), there is a global shortage of PPE, which poses significant risks to healthcare professionals' health and safety (6). Ensuring patient safety has become a key focus for healthcare institutions. Creating a safer patient environment is associated with a reduced risk of serious complications (7). Thus, fostering a secure patient care environment is crucial for delivering high-quality care and ensuring the safety of both patients and HCWs, enabling them to perform at their best (7, 8). The coverage rate of hepatitis B and diphtheria-tetanus (DT) vaccination among HCWs can vary depending on factors such as geographical location, healthcare facility policies, and individual compliance (9, 10). It is generally recommended that HCWs be vaccinated against hepatitis B and DT to protect themselves and their patients from potential infections. Regular monitoring and evaluation of vaccination coverage rates can help identify areas for improvement and guide the implementation of targeted interventions.
Healthcare workers understand the importance of maintaining up-to-date vaccinations and immunizations. By ensuring their own immunization status, they protect themselves and prevent the spread of vaccine-preventable diseases to vulnerable patients.
2. Objectives
This study aimed to investigate the level of compliance with all relevant infection control protocols, including hand hygiene, PPE usage, and vaccine coverage, among the staff of a children's hospital.
3. Methods
Mofid Children's Hospital is a tertiary referral center with multidisciplinary and subspecialty wards, located in Tehran, the capital city of Iran.
In this cross-sectional study, conducted over three months from May to August 2023, we objectively assessed the commitment of HCWs to personal infection control protocols using checklists recommended by the Iranian Ministry of Health (11).
The assessment of adherence to protocols was based on forms provided by the Ministry of Health of Iran, completed by the hospital's infection control nurse. Observations were recorded in the forms solely through direct observation and without any intervention.
List of variables assessed in this study:
- Adherence to strict hygiene practices
- Vaccination and immunization
- Use of PPE
- Patient isolation
3.1. Inclusion Criteria
The study included all HCWs at Mofid Children's Hospital, including doctors, nurses, and staff.
3.2. Exclusion Criteria
Medical students, interns, residents, and fellows were not included in this study because they were not considered permanent staff.
3.3. Adherence to Strict Hygiene Practices
Healthcare workers diligently followed stringent hygiene practices, including regular handwashing and the proper use of PPE. Trained observers assessed adherence to these protocols by directly observing HCWs during routine tasks. They documented whether each step on the checklist was followed correctly and noted any deviations or instances of non-compliance.
3.4. Vaccination and Immunization
To evaluate the vaccine coverage rate, we reviewed vaccination records and conducted interviews with HCWs. This approach provided objective data on the vaccination status of the individuals.
3.5. Personal Protective Equipment
We evaluated the appropriate use of PPE in our hospital using a query provided by the Iranian Health Ministry. This tool assessed variables such as whether staff used plastic boots when patients were likely to bleed profusely, wore double gloves during surgery or prolonged invasive procedures, and utilized masks and goggles/face shields when there was a possibility of splashing or spraying blood, body fluids, secretions, or excrement from patients.
3.6. Environmental Health
The survey of environmental health in our hospital was conducted based on an Iranian Health Ministry query, which evaluated various factors categorized as poor, average, or acceptable. The assessed items included:
- The condition of floors, walls, ceilings, and windows in different parts of the hospital
- Compliance with environmental health standards separately for HCWs and patients
- Monitoring the health condition of refrigerators in patients' rooms
- Investigating the ventilation conditions of patients' rooms, the process of separating infected sheets, and their transportation to the laundry.
3.7. Patient Isolation
Appropriate isolation plays a key role in preventing infections in hospitals. Therefore, we evaluated our adherence to suitable respiratory and contact protocols based on the guidelines provided by the Iranian Health Ministry.
3.8. Statically Analysis
The frequency and percentage of the evaluated variables were analyzed using SPSS version 23.
4. Results
4.1. Hand Hygiene
During the research period, a total of 936 HCWs, including 285 staff members, 260 doctors, and 391 nurses, were enrolled to evaluate adherence to hand hygiene protocols. Overall, the level of compliance ranged from 51%, observed among nurses, to 31%, observed among auxiliary personnel. The findings of our evaluation are presented in Figure 1 and Table 1.
| Variables | History of DT Vaccination | Compliance with Hand Hygiene Protocol | |||
|---|---|---|---|---|---|
| Yes | No | Unknown | Yes | No | |
| Doctors | 79 | 12 | 9 | 42 | 58 |
| Nurses | 79 | 1 | 20 | 51 | 49 |
| Staffs | 26 | 33 | 41 | 31 | 69 |
Abbreviation: DT: diphtheria-tetanus.
a Values are expressed as (%).
4.2. Vaccination
After conducting interviews with all staff, we evaluated their vaccination status based on self-reports and vaccination cards. The total coverage rate for the hepatitis B vaccine was 66%. Additionally, 18% of staff members had not received the vaccine, while 16% could not recall or provide documentation regarding their vaccination status.
Out of a total of 150 doctors, 145 reported a positive HBV vaccination history, while 3 had not received any vaccines, and 2 could not recall their vaccination status. (Medical students, interns, residents, and fellows were not included in this evaluation, as they were not considered permanent staff.)
Among nurses, 380 out of 386 reported a positive history of HBV vaccination, 3 had not been vaccinated, and 3 could not recall their vaccination status.
Data regarding the history of DT vaccination among HCWs across different hospital wards are presented in Table 1 and Figure 1.
In addition to evaluating overall hand hygiene compliance, we assessed adherence at five specific moments. The highest compliance rate, approximately 79%, was observed when HCWs handled patients' body fluids. Conversely, the lowest compliance rate, only 17%, was recorded when HCWs touched the surroundings of patients.
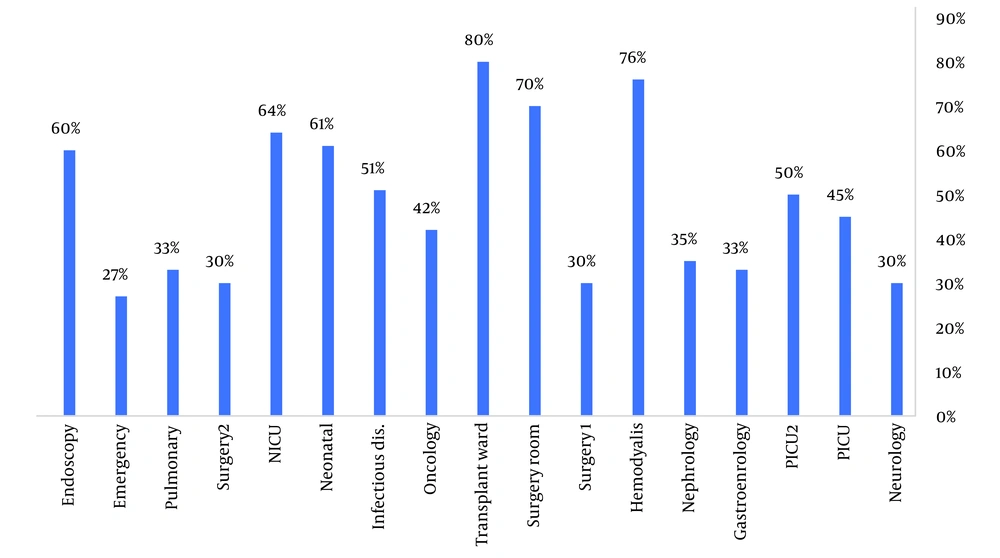
Compliance rates across various hospital wards showed that the transplantation and hemodialysis wards had the highest compliance levels at 80% and 76%, respectively. In contrast, the emergency ward demonstrated the lowest compliance rate at 27%. All data are presented in Figure 2.
We evaluated the frequency of correct PPE usage across different hospital wards. The findings showed an overall compliance rate of approximately 79%. The highest compliance with PPE protocols was observed in the transplant ward, while the lowest compliance was noted in the emergency department.
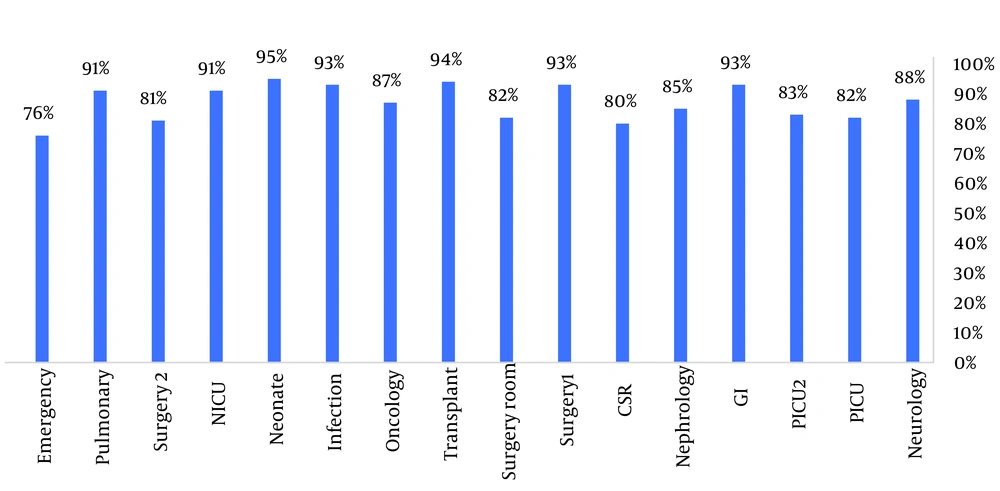
Additionally, we assessed the state of environmental health within the hospital, following the guidelines provided by the Iranian Ministry of Health. The results of this evaluation, categorized by ward, are presented in Figure 3.
We evaluated patient isolation practices and adherence to suitable contact, droplet, and airborne protocols based on the Iranian Health Ministry guidelines. Within the hospital, adherence rates were found to be 80%.
5. Discussion
The present research examined how well HCWs adhered to contact precautions and maintained environmental health across different hospital wards. Our findings showed an average compliance rate of 41% with hand hygiene protocols, with nurses demonstrating the highest adherence rates.
A study conducted in public health facilities in India reported a compliance rate of 19.4% with hand hygiene protocols, which may be attributed to increased workload and reduced nursing staff during the COVID-19 pandemic (12). In a different study conducted in Saudi Arabia, the compliance rate in a pediatric leukemia ward was 55.8% (13). These variations may be influenced by several factors, including the level of knowledge, patient load, and the availability of hand sanitizers in sufficient quantities and at appropriate locations. Similar to our findings, a 2023 study in Bangladesh reported an overall hand hygiene compliance rate of 25.3%, with the highest rate observed among nurses (28.5%), aligning with our results (14).
Consistent with our study, research from Bangladesh, the USA, and Japan also documented varying rates of compliance with PPE usage among HCWs (14-16).
Our study revealed a hand hygiene compliance rate of 51% among nurses, which is higher than the findings of a systematic review by Nouri et al., analyzing studies from 2005 to 2018 (17). The increased adherence observed in our study is likely due to the setting in a children's hospital, where pediatric patients are particularly vulnerable to infections.
When HCWs came into contact with body fluids, approximately 79% followed proper protocols. However, adherence to guidelines dropped significantly to 17% when HCWs interacted with the immediate environment surrounding patients. These findings are similar to those reported in a survey conducted in Nigeria (18).
We found that in certain medical wards where procedures were frequently performed, the utilization rate of PPE exceeded 85%. However, it was concerning to note that in the Emergency and Intensive Care Units (ICU), PPE usage fell below 85%. This lower rate could be attributed to the overwhelming influx of patients in the emergency ward, coupled with an inadequate nursing staff in the ICU. A previous study conducted at Mofid Children's Hospital in 2014 showed that disposable and surgical gloves were used in 41.82% of high-risk contacts. Notably, two studies conducted at the same hospital in different years reported similar results (19).
To improve adherence to PPE usage, a collaborative approach involving multiple stakeholders is essential. Furthermore, additional investigation is needed to better understand the factors influencing PPE compliance among HCWs.
Our research revealed that 66% of the workforce had received HBV vaccination prior to the study. Encouragingly, 98% of healthcare professionals, including doctors and nurses, had successfully completed their hepatitis B vaccinations, reflecting a remarkably high compliance rate. Regarding DT vaccination, studies indicate that approximately 79% of doctors and nurses had a positive vaccination history. However, the coverage dropped significantly to only 26% among other hospital staff not included in the medical profession.
The study by Hashemi et al. (20) reported higher HBV vaccination rates among HCWs in Hamadan, Iran, compared to the current study. These findings highlight the need for improved vaccination coverage in the hospital examined in this study.
Based on research conducted by Pruss-Ustun et al. in 2005, the estimated range of hepatitis B vaccination coverage among HCWs in different regions during the early 2000s varied between 18% and 77% (21, 22). However, more recent studies have shown improvements in vaccination coverage among HCWs in several countries. For instance, in Iran, the coverage was reported to be 84% over the past decade (20, 22). Similarly, Pakistan recorded a coverage of 74%, Saudi Arabia 63.3%, Libya 78.1%, and Turkey 72% (22-26). These figures demonstrate a notable increase in vaccination coverage among HCWs in these nations (22).
The results of the present study revealed that a higher percentage of doctors and nurses had received the DT vaccination compared to other hospital staff. On average, 52.5% of the hospital staff reported completing this vaccination. According to a recent study by Genovese et al. in Italy, 73% of hospital staff had received a diphtheria vaccination, while 77% had been vaccinated for tetanus (27).
Respiratory isolation was deemed appropriate in approximately 80% of cases. In comparison, research conducted in Canada indicated that only 74.6% of patients were placed in proper isolation. The primary factors contributing to noncompliance with isolation protocols included a lack of available isolation rooms and insufficient knowledge (28).
The findings of this study provided an overview of how well the Iranian Ministry of Health protocols are implemented in the hospital under investigation. By sharing this information with the hospital's infection control committee, strategies can be developed to enhance protocol adherence among HCWs, thereby improving infection control practices.
5.1. Limitations
This study has limitations in assessing the hand hygiene practices of HCWs and compliance with patient isolation protocols, as these factors should ideally be evaluated periodically. However, in this study, they were assessed during a specific timeframe.
Regarding the evaluation of personnel vaccination history, interns and fellows, who are technically part of the HCWs, were not included. This exclusion was due to their short-term presence in the hospital and frequent rotations to other hospitals. Additionally, maintaining a vaccine card in their records was not mandatory, resulting in a lack of data related to their vaccination status. The absence of a national vaccine card for adults in Iran further limited access to complete and accurate vaccination information, including for hospital staff. Consequently, we had to rely on self-reported data, which may not always be entirely accurate.
5.2. Conclusions
Although the protocols of the Ministry of Health are regularly taught and personnel demonstrate acceptable knowledge during periodic evaluations in our hospital, the results of this study revealed some shortcomings in the implementation and adherence to these protocols. Factors such as lack of time and overwhelming workloads, particularly in high-pressure wards like the emergency department, appear to hinder staff's ability to consistently comply.