1. Background
The sudden outbreak of a viral infection in December 2019 in Wuhan, China, led to a global tragedy, officially declared a pandemic by the World Health Organization (WHO) in March 2020. The responsible pathogen, Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2), caused COVID-19 infection. It rapidly spread worldwide, leading to hospitalizations and large numbers of patients requiring intensive care within weeks. Initially, the primary symptoms were nonspecific, such as fever, cough, dyspnea, muscle pain, and headache, but over time, the spectrum of symptoms expanded (1, 2).
With increasing global life expectancy, quality of life (QoL) has become one of the most important indicators of modern society. The WHO defines quality of life (WHOQoL) as “people's perception of their position in life in the context of the culture and value system in which they live and in relation to their goals, expectations, standards, and concerns" (3). Research on the impact of the COVID-19 pandemic on QoL in several countries has revealed significant influences on physical, mental, social, and spiritual health (4-7).
In the Iranian population, studies have shown a severe decline in health-related QoL (HRQoL) in the short-term follow-up after COVID-19 infection (8). Female gender and older age (≥ 40 years) were associated with both physical and mental impairments one month after recovery (9). However, the mid- and long-term complications for COVID-19 survivors post-hospital discharge remain less understood. A study in Italy found that, seven weeks after discharge, 53% of patients reported fatigue, 43% had shortness of breath, and 27% experienced persistent joint pain (7). Severe lower respiratory complications, such as pneumonia and acute respiratory distress syndrome (ARDS), were early recognized complications requiring oxygen support or ventilators (10, 11).
The NHS in England has predicted a high burden of physical, neurological, and social needs for COVID-19 survivors, much of which stems from ARDS (12). As the infection spread, more complications involving cardiovascular, renal, and neurological systems emerged. Some were caused by the virus itself, while others were due to long hospital admissions or medications used in COVID-19 treatment. Complications seem to persist long after recovery from the acute phase, with hypoxic damage, neurological sequelae (such as dysgeusia, anosmia, ataxia, convulsions) (13), and impaired respiratory function (14) significantly impairing patients' future QoL.
The pandemic's impact on mental health has been substantial, with anxiety and depression being particularly concerning. Different populations, depending on socioeconomic status and available resources, may experience the pandemic's effects differently.
2. Objectives
This study aims to assess the physical and psychological impairments (levels of anxiety and depression) observed in patients six months after recovery from acute COVID-19, using HRQoL assessments via a validated questionnaire.
3. Methods
This cross-sectional study included patients from emergency departments, infectious wards, and clinics designated for COVID-19 management. Ethics approval was obtained from the Shiraz University of Medical Sciences (IR.SUMS.REC.1399.1007). Informed consent was collected from all participants.
Inclusion criteria were: Confirmed COVID-19 infection via RT-PCR, candidacy for one of the available treatment modalities (remdesivir, favipiravir, tocilizumab, or pirfenidone), and consent to participate. Patients were interviewed during the acute phase, with demographic data being collected. Six months after their confirmed infection, patients were re-interviewed to assess their QoL post-COVID-19 infection. This assessment was based on the validated Persian version of the EQ-5D-3L questionnaire, which measures health-related quality of life (HRQoL) regardless of the disease (EuroQol. EQ‐5D is available upon request from https://euroqol.org). Using this questionnaire, five areas were evaluated: Mobility, personal care, usual activities, pain, and anxiety/depression. The questionnaire consisted of three main sections: Demographic information, including gender, age, education level, marital status, and employment status; general health status, where participants were asked about their perceptions of their health and any existing illnesses or health issues using the question, "Do you have any illness, health problem, condition, or disability?" Those who reported any issues were prompted to identify specific conditions from a list or specify their illnesses, with the option to mention multiple conditions; and the EQ-5D-3L assessment, which was used to evaluate the participants’ HRQoL score. Each area was graded at three levels: No problems, some problems, and extreme problems. Patients confirmed their health status by marking their current condition, and each section was assigned a score reflecting the level of impairment. The overall assessment was represented by a five-digit number describing the patient's overall health status. EQ-5D-3L items were assessed at both time points, before and after the infection, to allow for a better comparison of HRQoL impairment. At the end of the questionnaire, participants rated their overall QoL post-COVID-19 infection on a scale of 1 - 100, assuming their pre-infection QoL score was 100.
Statistical analysis was conducted using IBM SPSS 28 software. For quantitative data, the mean ± SD was used, while qualitative data were summarized using medians. Data frequency was expressed as a percentage. The comparison of qualitative parameters in the questionnaire was performed using the chi-square test, and the overall QoL before and after COVID-19 infection was evaluated with an independent t-test. A P-value < 0.05 was considered statistically significant. Kruskal-Wallis analysis was employed to evaluate differences between pre- and post-COVID-19 assessments across different categories. Since various factors might interfere with the study outcome, baseline characteristics documented at the beginning of the study were analyzed for their association with patients’ HRQoL using a regression analysis model. Factors such as age, gender, education level, history of comorbid diseases, and ICU admission were evaluated for their potential association with impairments in HRQoL in this study population.
4. Results
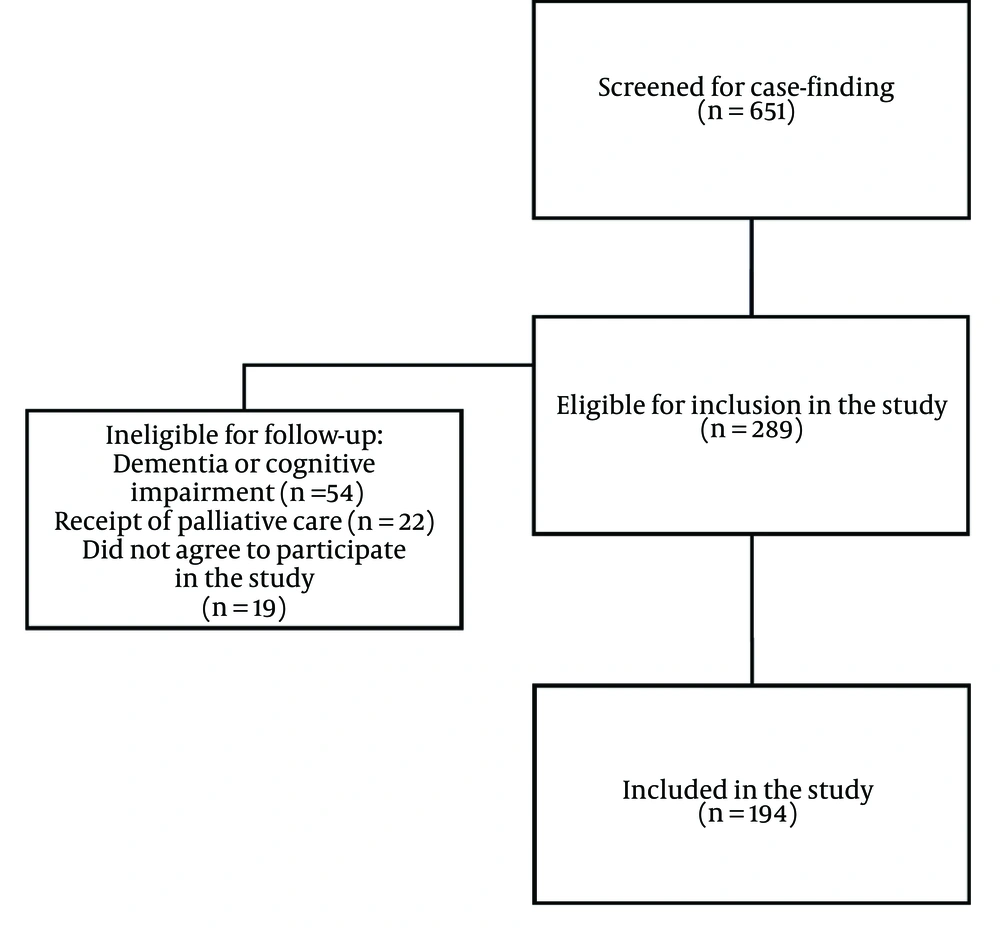
Out of 651 COVID-19 infected patients initially surveyed for inclusion, 289 potential participants were identified, with 95 subsequently excluded, as shown in the study’s flow diagram. Ultimately, 194 patients met the inclusion criteria and were enrolled in this cross-sectional study (Figure 1). The baseline demographic and clinical data of the patients are presented in Table 1. The study population consisted of a nearly equal number of male (95) and female (99) patients, with a mean age of 50.1 ± 15.8 years. The majority of participants had a low level of education, and most had a history of diabetes mellitus and hypertension. While most patients were hospitalized during the course of their infection, the majority did not experience a severe form requiring ICU admission. The average duration of COVID-19 infection with acute symptoms was 28 ± 2.1 days.
| Characteristic | Frequency (%) |
|---|---|
| Gender | |
| Female | 95 (49) |
| Male | 99 (51) |
| Level of education | |
| Illiterate or some elementary school degree | 71 (36.6) |
| Middle school to high school diploma | 49 (25.3) |
| Bachelor’s degree to master’s degree | 62 (32) |
| Doctorate’s degree or more | 12 (6.2) |
| Past medical history | |
| Hypertension | 33 (17) |
| Diabetes | 32 (16.5) |
| Ischemic heart disease | 23 (11.9) |
| Thyroid disorders | 8 (4.1) |
| Asthma/allergy | 7 (3.6) |
| Autoimmune disease | 3 (1.5) |
| Malignancy | 4 (2.1) |
| Type of medication used for COVID-19 infection | |
| Remdesivir | 50 (26) |
| Favipiravir | 50 (26) |
| Tocilizumab | 50 (26) |
| Pirfenidone | 44 (22.9) |
| Course of COVID infection | |
| Outpatient | 81 (41.8) |
| Inpatient (ward admission) | 86 (44.3) |
| Inpatient (ICU admission) | 27 (13.9) |
Abbreviation: ICU; intensive care unit.
The assessment of patients’ HRQoL before and after COVID-19 infection, using the EQ-5D-3L questionnaire, is shown in Table 2. Impairment was observed across all fields. In terms of mobility, patients in the post-COVID-19 phase mostly reported difficulty walking compared to their pre-infection ability. Regarding self-care, there was mild impairment, with difficulties in daily activities such as showering or dressing independently. There was slight impairment in usual activities after the infection, while pain and discomfort significantly increased. Mental and psychological effects, particularly anxiety and depression, were also significantly heightened after the infection, with anxiety, depression, and difficulty walking being the most prominent issues.
| Category of Impairment and Timing | Frequency (%) | Deterioration Rate (%) |
|---|---|---|
| Mobility | ||
| I have no problem in walking about | 37.7 | |
| Pre-infection | 193 (99.5) | |
| Post-infection | 120 (61.8) | |
| I have some problems in walking about | 36.1 | |
| Pre-infection | 0 | |
| Post-infection | 70 (36.1) | |
| I am confined to bed | 1.6 | |
| Pre-infection | 1 (0.5) | |
| Post-infection | 4 (2.1) | |
| Self-care | ||
| I have no problems in self-care | 3.6 | |
| Pre-infection | 192 (99) | |
| Post-infection | 185 (95.4) | |
| I have some problems with washing or dressing myself | 3.1 | |
| Pre-infection | 0 | |
| Post-infection | 6 (3.1) | |
| I am unable to wash or dress myself | 0.5 | |
| Pre-infection | 2 (1) | |
| Post-infection | 3 (1.5) | |
| Usual activities (work, study, housework, …) | ||
| I have no problems in performing my usual activities | 12.9 | |
| Pre-infection | 192 (99) | |
| Post-infection | 67 (86.1) | |
| I have some problems with performing my usual activities | 11.9 | |
| Pre-infection | 1 (0.5) | |
| Post-infection | 24 (12.4) | |
| I am unable to perform my usual activities | 1 | |
| Pre-infection | 1 (0.5) | |
| Post-infection | 3 (1.5) | |
| Pain/discomfort | ||
| I have no pain or discomfort | 10.8 | |
| Pre-infection | 188 (96.9) | |
| Post-infection | 167 (86.1) | |
| I have moderate pain or discomfort | 10.3 | |
| Pre-infection | 4 (2.1) | |
| Post-infection | 24 (12.4) | |
| I have extreme pain or discomfort | 0.5 | |
| Pre-infection | 2 (1) | |
| Post-infection | 3 (1.5) | |
| Anxiety/depression | ||
| I am not anxious or depressed | 42.2 | |
| Pre-infection | 190 (97.9) | |
| Post-infection | 108 (55.7) | |
| I am moderately anxious or depressed | 33.5 | |
| Pre-infection | 4 (2.1) | |
| Post-infection | 69 (35.6) | |
| I am extremely anxious or depressed | 8.8 | |
| Pre-infection | 0 | |
| Post-infection | 17 (8.8) |
After evaluating responses in the five categories, significant impairment in all HRQoL categories was observed when comparing pre- and post-COVID-19 scores (P-value < 0.05), as presented in Table 3. According to Table 4, older age (≥ 40 years), female gender, and ICU admission were associated with worsened health status post-COVID-19 infection.
| Category of Impairment | Score | P-Value | |
|---|---|---|---|
| Pre-COVID Infection | Post-COVID Infection | ||
| Mobility | 1 ± 0.2 | 1.49 ± 0.5 | < 0.001 |
| Self-care | 1.02 ± 0.9 | 1.06 ± 1 | 0.01 |
| Usual activities | 1.01 ± 0.5 | 1.15 ± 0.6 | < 0.001 |
| Pain/discomfort | 1.03 ± 0.6 | 1.15 ± 0.7 | < 0.001 |
| Anxiety/depression | 1.02 ± 0.3 | 1.5 ± 0.5 | < 0.001 |
a Values are presented as mean ± SD.
b Kruskal–Wallis one-way analysis of variance.
| Factors Affecting Health Status | Odds Ratio (95% CI) | P-Value |
|---|---|---|
| Age (ref: < 40 y) | 2.72 (1.54-3.38) | 0.025 |
| ≥ 40 | ||
| < 40 | ||
| Gender (ref: Male) | 2.64 (1.76-6.14) | 0.005 |
| Level of education (ref: Elementary school degree) | 0.87 (0.62-1.76) | 0.598 |
| Past medical history (ref: No) | 1.34 (0.82-2.92) | 0.355 |
| ICU admission (ref: No) | 2.22 (1.14-4.32) | 0.019 |
Abbreviations: ICU; intensive care unit, CI, confidence interval; ref, reference category.
The mean overall reduction in QoL score post-COVID-19 infection, as reported by the patients, was approximately 25%, with an overall score of 76.5 ± 26.6. The main complaints were fatigue, followed by anxiety, dyspnea, depression, and hair loss, all of which significantly impacted their QoL.
5. Discussion
During the past three years of the SARS-COV-2 outbreak worldwide, millions of deaths due to the infection have been reported (15, 16). Aside from its mortality, those who survived the infection were not spared from the long-term devastating effects of this deadly virus. Various studies have assessed QoL at different time intervals post-COVID-19 infection. Some studies evaluated the early continuation of symptoms within a month after the acute phase (17), while others examined the persistence of symptoms and impaired QoL over a longer duration (7). Most of these studies have shown significant impairment in QoL among hospitalized patients after recovery from COVID-19; however, the impact of persistent symptoms on QoL in non-hospitalized patients may have been underestimated. Similar studies in the region have focused on shorter time intervals (1-3 months) post-COVID-19 infection and on different age groups, such as children and adolescents. (18, 19). As evident in the results of this study, impairment of QoL was observed in all categories of assessment six months after recovery from the acute infection. The most significant damage was observed in patients’ mental health, with an approximately 30% rise in anxiety and depression six months after recovering from the acute phase of the infection. Deterioration of mental health has been reported in recent meta-analyses inspecting the effects of post-COVID syndrome on QoL (20), and the risk of developing depression in patients, particularly hospitalized patients, has been estimated to be high compared to the normal general population (21). Since almost 58% of the patients experienced hospital admission for their treatment, the increase in anxiety and depression may be attributed to both the infection itself and the course of treatment (22). Some reasons for increased anxiety and depression during the course of hospital admission and treatment are prolonged admissions, the unfamiliar environment of the hospital, ICU admissions with no visitors allowed, the course of intubation that the patient may not remember, disease stress, long-term high-dose corticosteroid therapy, discharge of the patient with a supplemental oxygen requirement, and the financial burden of admission. As evident in the results, ICU admission, indicative of a more severe disease, was negatively associated with the patient’s health status. Stress related to ICU admission has been a poor predictive factor for HRQoL outcomes in various settings (23, 24). Similarly, the socioeconomic status and level of literacy of patients can be influential factors in impaired QoL (25). The majority of the study population had a low level of education and likely low socioeconomic status. Health-related illiteracy toward preventive and therapeutic measures, as well as low-income status, have been found to predict deteriorated QoL (26, 27), although this variable did not significantly impact patients’ QoL in this study. Health literacy concerning anxiety and depression has shown beneficial effects in protecting against post-COVID impairment of QoL (28). Additionally, problems in mobility increased, with a 37% rise in patients reporting some difficulties in walking compared to their condition before the infection. Loss of physical abilities has been reported previously, in line with the results of this study (29). Female gender and older age have been associated with impairment of physical ability and aspects of QoL (17). As shown in the results, female gender and age ≥ 40 years were factors that were associated with impaired health status (P-value < 0.05). In terms of the effect of age on the long-term COVID-19 effects, health impairment in children and younger age has also been studied. Variation in the prevalence of long-term effects of COVID-19 infection in children has been observed, and data are heterogeneous. High rates of fatigue, anosmia, arthralgia, headache, and long-standing dyspnea have been among the most frequent health-related complaints of children after recovering from COVID-19 infection (30, 31). It has been confirmed that comorbid medical conditions and prolonged hospital stays are predictive factors of impaired physical and mental QoL post-COVID-19 infection (32). The highest rate of preexisting medical conditions was diabetes and hypertension, the two major clinical conditions that predispose patients to severe disease and independently predict HRQoL values (24, 26), potentially leading to hospital stay. Although the length of the hospital stay was not recorded in this study, the use of tocilizumab as an anti-inflammatory agent confirms the severity of the disease in 26% of the study population. This confirms the devastating long-term physical and psychological effects of this deadly pandemic, which, despite appearing to have subsided, continues to cause lasting damage. The physical and mental issues associated with COVID-19 must be addressed, considering each nation’s beliefs and providing medical and economic support to prevent long-lasting damages to the future well-being of societies. Long-term fatigue has been introduced as a major complication lasting well beyond the acute symptoms (33). Persistent fatigue can significantly contribute to impairments in all QoL categories assessed in this study, including mobility, self-care, usual activities, pain, anxiety, and depression. The overall QoL post-COVID-19 infection has been shown to decline in various studies conducted in different regions with diverse populations (24, 34). This confirms the devastating long-term physical and psychological effects of this deadly pandemic, which, despite appearing to have subsided, continues to cause lasting damage. The physical and mental issues associated with COVID-19 must be addressed, considering each nation’s beliefs and providing medical and economic support to prevent long-lasting damages to the future well-being of societies.
Like any study, this study has limitations. The subjective nature of questionnaire-based studies may introduce variation in the overall report due to differences in each patient’s perception of their disabilities. Additionally, due to the profound mental impairment observed post-COVID-19, a significant number of patients allocated at the beginning of the study could not complete the trial and were not included in the final analysis, reducing the total study population. This further supports the severe negative impact of COVID-19 on patients’ mental health and QoL. Unfortunately, QoL assessments are mainly based on questionnaires, and the subjective quality of the assessment cannot be overcome, but cross-checking the questionnaire with a close caregiver who has observed the patient’s impairments during the infection and after recovery can be a suggestion that may improve the reliability of answers given to each question by the patient himself. This method may also be applied if profound mental impairment leads to patient loss during the study.
5.1. Conclusions
Impairment in QoL, physical and mental abilities of patients after COVID-19 infection was evident. Female gender, age ≥ 40 years, and ICU admission were independently associated with impairment of QoL. Impairments in QoL post-COVID-19 must be detected and addressed in different societies with diverse social, economic, and healthcare settings to mitigate the further damage to the well-being of populations. Prompt investigation and detection of the population with impairments in HRQoL is mandatory for developing health policies, including free-of-charge rehab and counseling sessions to prevent further damage and economic burden to societies and their healthcare systems.