1. Background
Exudative diarrhea in children under five is characterized by the presence of abnormal blood, mucus, or pus in the stool, indicating inflammation or damage to the intestinal lining (1). This condition can be particularly severe in young children, often leading to dehydration and malnutrition (2, 3).
Clinical manifestations of exudative diarrhea include the presence of blood and/or mucus in the stool, increased stool frequency and volume, fever, nausea, abdominal pain, irritability, and mild to moderate dehydration (4-6). Bloody diarrhea is a clear indicator of exudative diarrhea, suggesting involvement of the lower intestine. The presence of white blood cells in the stool further signals an ongoing inflammatory process. Exudative diarrhea is generally more severe than watery or non-bloody diarrhea and, if untreated, can lead to complications such as electrolyte imbalances, malnutrition, and dehydration (7, 8).
The causes of exudative diarrhea are often multifactorial, involving various bacterial pathogens. Understanding the prevalence and distribution of these pathogens is essential for effective disease management and prevention (9). Research has shown that hospital-acquired diarrhea in this age group frequently involves diarrheagenic Escherichia coli (DEC) and Cryptosporidium, with DEC being the most commonly identified pathogen in hospital settings (5, 10, 11).
Polymerase chain reaction (PCR) has proven to be an effective molecular technique for the rapid and accurate detection of bacterial pathogens, enabling extensive epidemiological studies across different regions and populations (12). In Iran, exudative diarrhea remains a major health issue among children under five, contributing to increased morbidity and mortality. Despite the significant role of bacterial pathogens, comprehensive data on their frequency and distribution across various regions of Iran remain limited (13).
2. Objectives
The objective of this study was to examine the frequency of bacteria responsible for exudative diarrhea in samples from children under five years of age.
3. Methods
3.1. Study Design and Sampling
In this multicenter cross-sectional descriptive study, 104 children with exudative diarrhea, referred to Mofid Children's Hospital in Tehran, as well as hospitals in Hamedan, Ardebil, and Bandar Abbas between December 2020 and March 2022, were enrolled.
3.1.1. Inclusion Criteria
Children under five years of age with confirmed exudative diarrhea at the time of sampling were included in the study.
3.1.2. Exclusion Criteria
Children with diarrhea types other than exudative were excluded.
3.1.3. Sample Collection and Handling
Stool samples were collected from patients and transferred to the laboratory at the Pediatric Infections Research Center (PIRC) within six hours of collection.
3.1.4. Data Collection
A questionnaire was used to gather information regarding age, gender, clinical manifestations, and the bacterial agents identified in the exudative stool samples.
The study was approved by the Ethics Committee of Shahid Beheshti University of Medical Sciences.
3.2. Samples Preparation
Stool samples were processed by adding 1000 µL of sterile, DNase- and RNase-free water to 5 grams of stool, followed by thorough mixing. The mixture was then centrifuged at 5000 rpm for 5 minutes to separate the upper supernatant, from which DNA was subsequently extracted.
3.3. Molecular Detection of Bacteria
The DNA extraction from all samples was performed using a commercial extraction kit (SIMBIOLAB Company) in accordance with the manufacturer’s protocol. The identification of causative bacteria was conducted using various PCR methods, as outlined in Table 1.
| Methods | Bacteria |
|---|---|
| Multiplex RT-PCR a | Clostridium difficile |
| Yersinia enterocolitica | |
| Multiplex conventional PCR | Campylobacter spp. |
| Salmonella spp. | |
| Multiplex conventional PCR | E. coli-Stx1 |
| E. coli-Stx2 | |
| Conventional PCR | Shigella spp. |
a Real-time PCR
The primers and PCR conditions used in this study were based on those described in previous studies (14, 15). The specific primers used are listed in Table 2.
| Bacteria and Primer Sequencing 5’ to 3’ | Target Genes | PCR Product Size (bp) | References |
|---|---|---|---|
| C. difficile | 16srRNA | 157 | (14) |
| Forward, TTGAGCGATTTACTTCGGTAAAGA | |||
| Reverse, CCATCCTGTACTGGCTCACCT | |||
| Y. enterocolitica | ail | 91 | |
| Forward, GGTCATGGTGATGTTGATTACTATTCA | |||
| Reverse, CGGCCCCCAGTAATCCATAA | |||
| Campylobacter spp. | 16srRNA | 812 | (15) |
| Forward, GGATGACACTTTTCGGAGC | |||
| Reverse, CATTGTAGCACGTGTGTC | |||
| Salmonella spp. | ttRSBCA | 344 | |
| Forward, CCTGTCAGCCAAATATTACG | |||
| Reverse, ACGACGGGTTAAATTAGCCA | |||
| E. coli-Stx1 | stx1 | 329 | |
| Forward, TGACAGTAGCTATACCACGT | |||
| Reverse, GAACAGAGTCTTGTCCATGA | |||
| E. coli-Stx2 | Stx2 | 376 | |
| Forward, GGACCTCACTCTGAACTG | |||
| Reverse, CCGCCATTGCATTAACAGAA | |||
| Shigella spp. | ipaH | 342 | |
| Forward, TGAAGTTTCTCTGCGAGCAT | |||
| Reverse, CAATACCTCCGGATTCCG |
3.4. Statistical Analysis
Statistical analysis was performed using SPSS version 22 software (IBM, Chicago, USA). Quantitative data are reported as mean ± SD, and qualitative data are presented as counts (percentages). The chi-square test was conducted to assess the association between gender and age group in patients with exudative diarrhea. The results indicated no statistically significant relationship between the two variables (P = 0.0765), suggesting that gender distribution does not significantly vary across different age groups in this patient population.
4. Results
This study included children under the age of five, with most participants being either under 12 months (31%) or between 12 and 24 months (22%). Among the patients, 66% were male. Fever was present in approximately 70% of cases, while the remaining 30% had normal body temperature. Vomiting was reported in 58% of the patients, and 56% exhibited signs of dehydration. Additional details are provided in Table 3.
| Variables | No. (%) |
|---|---|
| Age (mo) | |
| ≥ 12 | 33 (31) |
| 13 - 24 | 23 (22) |
| 24 - 36 | 12 (11) |
| 36 - 48 | 9 (0.08) |
| 48 - 60 | 9 (0.08) |
| < 60 | 18 (0.17) |
| Gender | |
| Male | 69 (66) |
| Female | 35 (34) |
| Fever | 73 (70) |
| Dehydration | 44 (42) |
| Vomiting | 60 (58) |
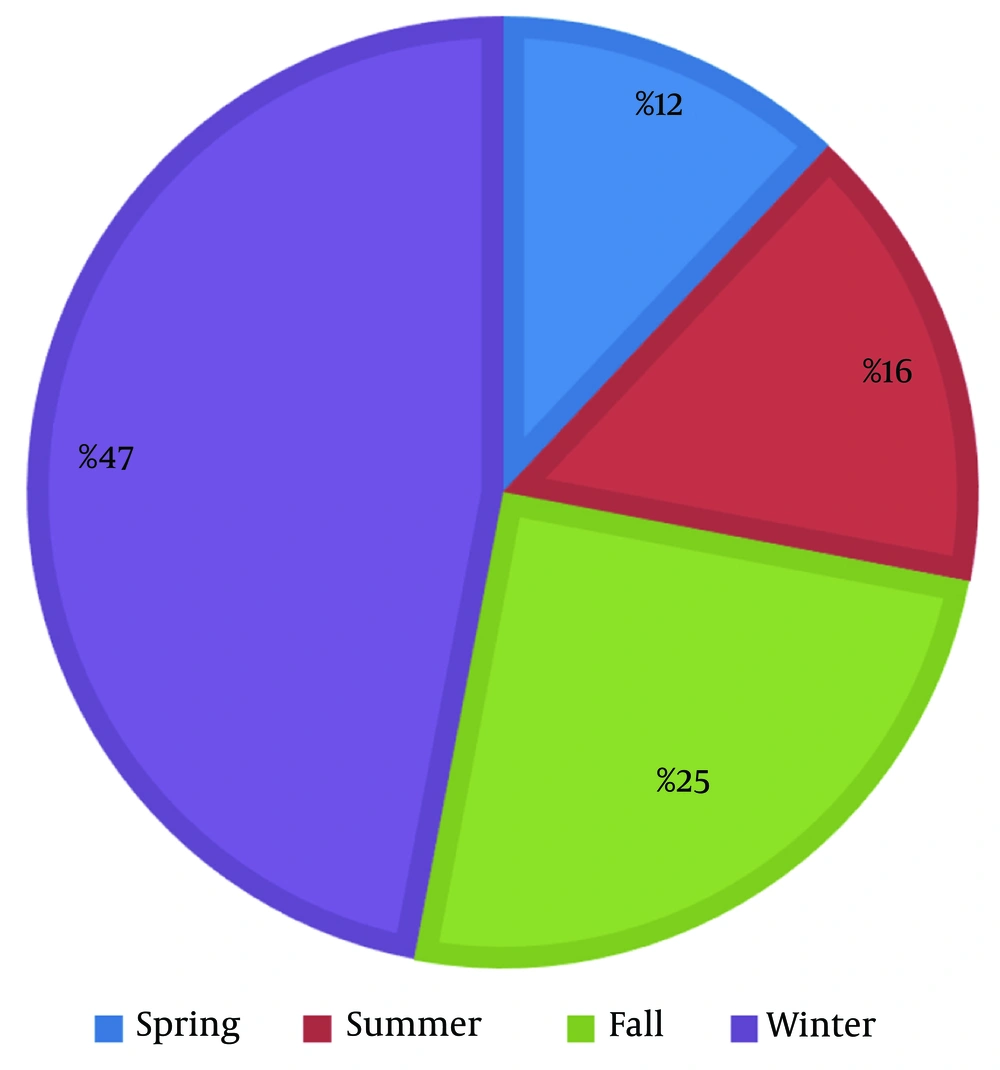
In this study, samples were collected from three cities, with 54.8% obtained from Tehran, 32.7% from Hamadan, and 4.8% from Bandar Abbas. The seasonal distribution of the samples is illustrated in Figure 1.
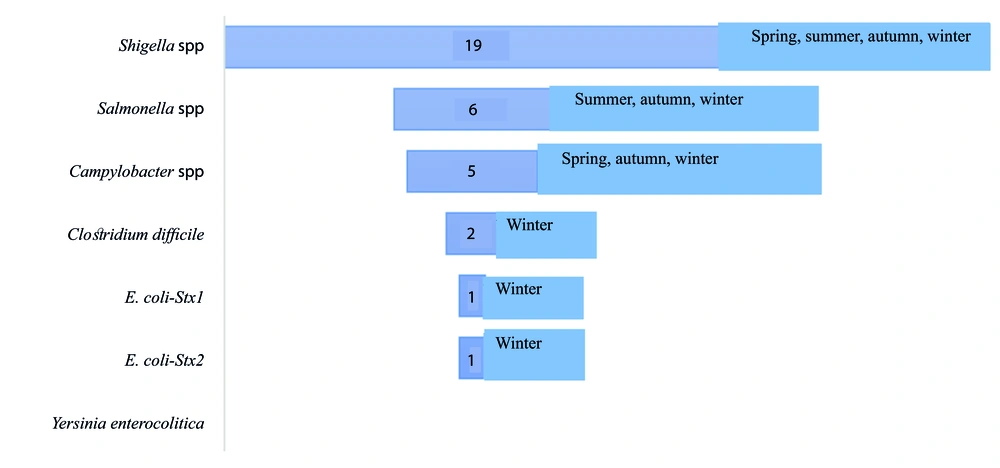
DNA extraction was performed on 104 stool samples. The most common pathogens associated with exudative diarrhea were Shigella spp., Salmonella spp., Campylobacter spp., Clostridium difficile, E. coli-Stx1, and E. coli-Stx2, in that order. Specifically, Shigella spp. and Salmonella spp. were identified as the leading causes of exudative diarrhea, as shown in Figure 2.
5. Discussion
This study aimed to investigate the frequency of the most common bacteria causing exudative diarrhea in children under five years of age across various cities in Iran. Our results revealed that the highest prevalence of diarrhea was observed in children aged 12 months or younger, with the lowest prevalence noted in those aged 36 - 48 and 48 - 60 months. This finding contrasts with Saeed et al.'s study, which reported the highest frequency of cases in the 49 - 60-month age group (66%), followed by the 37 - 48-month age group (18%) (14).
The gender distribution of the patients is also noteworthy, with 66% of the participants being male and 34% female. This aligns with Saeed et al.'s findings, where 55% of the cases were in male children (14), a trend observed in numerous previous studies (15).
Among the bacterial causes of exudative diarrhea, Shigella spp., Salmonella spp., Campylobacter spp., Clostridium difficile, E. coli-Stx1, and E. coli-Stx2 were identified as the most prevalent.
Figure 2 provides data on the bacterial agents identified in positive samples from patients with exudative diarrhea. A detailed analysis is as follows:
(1) Shigella spp.: This bacterium was the most frequently identified pathogen, found in 19 positive samples. Shigella spp. is a well-known cause of bacterial dysentery, particularly common in children under five years old, especially in developing regions. The high frequency of Shigella suggests it may be the leading cause of exudative diarrhea in this patient population.
(2) Salmonella spp.: Identified in 6 positive samples, Salmonella is a significant pathogen associated with gastrointestinal infections in children. Although less common than Shigella, it still contributes notably to diarrheal disease in this population.
(3) Campylobacter spp.: With 5 positive samples, Campylobacter spp. also plays a role in causing diarrhea in this group. Campylobacter is a common bacterial cause of gastroenteritis worldwide and is often linked to foodborne outbreaks.
(4) Clostridium difficile: Identified in 2 positive samples, Clostridium difficile is typically associated with antibiotic-related diarrhea and can cause severe illness in young children. Although its prevalence in this study is low, its presence is clinically significant, particularly in healthcare settings.
(5) E. coli (Stx1 and Stx2): Each of these shiga toxin-producing E. coli (STEC) strains was found in 1 positive sample. Although less frequently identified, these strains can cause severe diarrhea and complications like hemolytic-uremic syndrome (HUS). The low numbers suggest a limited but potentially severe role in disease within this cohort.
(6) Yersinia enterocolitica: No positive samples were identified for Yersinia enterocolitica. This bacterium is less common and may not be a significant contributor to diarrheal illness in this specific population or region.
In summary:
- Shigella spp. is the dominant pathogen in this study, highlighting it as a primary target for interventions and treatment strategies.
- Salmonella spp. and Campylobacter spp. are also important pathogens, though less frequent.
- The presence of Clostridium difficile and shiga toxin-producing E. coli (STEC) underscores the diversity of bacterial agents responsible for exudative diarrhea, albeit less commonly.
- Yersinia enterocolitica appears to be absent in this patient group.
The data from Figure 2 emphasize the need for targeted treatment strategies and public health interventions focusing on the most common bacterial agents like Shigella spp., while also accounting for the less frequent but clinically significant pathogens.
The prevalence of the most common bacteria responsible for exudative diarrhea in children under five years old across various cities in Iran was examined using PCR. In contrast, Abed and Hassan reported that E. coli was prevalent in 55.56% of diarrheal infections (16). Variations in methodology and differences in sample size may explain this discrepancy.
In northwest Iran, Shigella species, particularly S. sonnei, were found in 85.7% of diarrheal patients (13). This contrasts with our findings, likely due to the smaller sample size in our study.
In the study by Eybpoosh et al., E. coli pathotypes were the most prevalent among children under five, accounting for 73% of cases (3). A recent systematic review in Iran also highlighted ETEC as a major pathotype, with a pooled prevalence of 16% (95% CI: 11% - 23%) (17). Moreover, previous studies in Iran have frequently identified ETEC as a common cause of diarrhea in young children (18, 19). However, our study’s findings do not align with these observations, likely due to regional and methodological differences.
In the study by Saeed et al., 48% of 437 stool samples from children with diarrhea tested positive for Escherichia coli, 8% for Shigella spp., 4% for Salmonella spp., and 2% for Campylobacter spp. (14). These results are consistent with our findings. Similarly, Jafari et al. reported a high prevalence of Shigella species in 148 samples and shiga toxin-producing Escherichia coli (STEC) in 105 samples. Additionally, EAEC, EPEC, Campylobacter, Salmonella, and ETEC were found in 92, 70, 60, 42, and 38 samples, respectively. Jafari et al.'s study did not isolate Yersinia from the stool samples, and most of the children studied (464 cases) were under one year old (19).
These results align with our findings. Like the study by El Qouqa, Yersinia enterocolitica was not detected in our study, and only a few Salmonella infections were reported (20). Furthermore, Asadi et al. found E. coli to be the most common pathogen causing diarrhea in children aged 2 months to 12 years (21). Identifying the causative agents of diarrhea, achieving rapid and accurate diagnosis, and implementing effective management strategies are crucial for preventing outbreaks.
This study has several limitations. Firstly, the small sample size is a notable limitation. Secondly, while samples were collected from various hospitals in different cities, they may not fully represent the broader population of children under five years of age in Iran. Future research addressing these limitations could provide a more comprehensive understanding of the epidemiology of bacterial exudative diarrhea in Iranian children and aid in the development of more effective prevention and control measures.
5.1. Conclusions
In conclusion, Shigella spp. emerged as the primary cause of diarrhea in children under five years of age in our study. It is recommended that future research involve specific molecular epidemiology studies with larger sample sizes to more accurately identify and understand the prevalence of diarrhea-causing infections.
The generalizability of these results may be influenced by several factors. First, while the study focused on children under five across various cities in Iran, providing valuable insights into the prevalence of exudative diarrhea in this population, the findings may not be universally applicable to all regions or age groups. Geographical, environmental, and demographic differences could affect the distribution of diarrheal pathogens. Additionally, variations in study methodologies and sample sizes, as seen in comparisons with other studies, may limit the broader applicability of the results. Future research with larger, more diverse sample populations across different regions could enhance the generalizability of these findings and provide a clearer understanding of the epidemiology of bacterial diarrhea in children.