1. Introduction
COVID-19 is typically a mild or asymptomatic disease in children, but some children with underlying conditions are at increased risk of severe disease. Although children without underlying medical conditions can experience severe illness (1). Based on data reported to the WHO between December 30, 2019, and September 6, 2021, children under 5 years old were a very small number of the under 24 years old cases, about 1.8% of global cases; the 5 - 15 years and 15 - 24 years old groups were 6.2% and 14.3% of global cases, respectively (2). According to the MPIDR COVerAGE database (Max Planck Institute of Demographic Research) in Rostock, Germany, 4.4 million deaths due to COVID-19 disease were reported in 2023 from 120 countries. Of these, 0.4 percent (17,400 cases) occurred in children and adolescents under 20 years, with 53% in the 10 - 19 years age group and 47% in the 0 - 9 years age group (3). Neurological involvement is frequent in the pediatric age group, in patients affected by both COVID-19 and, even more, MIS-C. Neurological symptoms and signs are highly heterogeneous. The frequency of certain neurological manifestations varies depending on the patient’s age. Symptoms and signs can even be differentiated in the two groups, COVID-19 and MIS-C, but consciousness impairment is the most frequent manifestation in both groups and may underlie an encephalopathy. The latency of neurologic manifestations was greater in the MIS-C group, so suspicion should remain high in the days after onset. Most neurological manifestations were mild in our series; however, severe complications, such as ischemic stroke and GBS, are noteworthy (4). COVID-19 disease is mild in children, but severe COVID-19, myocarditis, heart problems, Kawasaki disease, MIS-C, and long-term COVID-19 may occur in children, with the probability increasing if there are risk factors. Neurologic complications may occur in 7% of children with COVID-19 and include febrile seizure, afebrile seizure, encephalopathy, brain abscess, bacterial meningitis, and cerebral infarction. The least common complication is cerebral infarction (0.05%) (5). In the USA, 20% of children admitted to the PICU with COVID-19 had heart complications, consisting of arrhythmia, myocarditis, pericarditis, and cardiac vessel vasculitis (6). In this article, a child who suffered from MIS-C followed by COVID-19, myocarditis, and brain complications is reported, and the mechanism and treatment options are discussed.
2. Case Presentation
The patient, a 4-year-old girl with no known past medical history, presented with a recent episode of flu-like symptoms and abdominal pain persisting for 12 days without response to oral medications, culminating in severe respiratory distress. The parents denied consanguinity. Upon admission to the hospital, the child exhibited signs of respiratory distress, including tachypnea, decreased oxygen saturation levels, and the use of accessory muscles. Initial assessment revealed pleural effusion on chest X-ray, and after chest tube insertion, massive pleural effusion was observed. Heart sounds revealed a 3/6 murmur. Following chest tube insertion, the patient experienced a further drop in oxygen saturation, necessitating intubation. After intubation, negative pressure pulmonary edema occurred due to non-stepwise and large-volume pleural fluid drainage, presenting with pink foam discharge from the mouth and tracheal tube. Pleural fluid analysis showed cholesterol 9 mg/dL, TG 18 mg/dL, LDH 465 U/L, glucose 170 mg/dL, protein 1480 mg/dL, WBC 4, and RBC 1000 (Table 1). Aerobic and anaerobic pleural fluid cultures were negative.
| Lab Findings | Normal Range | Result |
|---|---|---|
| Hb (g/dL) | 11.9 - 15 | 10.9 |
| WBC (mm3) | 4800 - 10800 | 15100/mm3 |
| PLT (mm3) | 150000 - 280000 | 259000 |
| ESR (mm/h) | 0 - 10 | 10 |
| CRP (mg/dL) | 1 - 10 | 2 |
| BUN (mg/dL) | 5 - 18 | 18 |
| Creatinine (mg/dL) | 0.3 - 0.7 | 0.6 |
| AST (IU/L) | 10 - 40 | 72 |
| ALT (IU/L) | 10 - 40 | 81 |
| LDH (Unit/L) | 143 - 370 | 1324 |
| CPK (mcg/L) | 10 - 120 | 543 |
| Uric Acid (mcg/dL) | 2.4 - 5.5 | 5.1 |
| Total Pro (g/dL) | 5.7 - 8 | 5.2 |
| Alb g/dL | 3.4 - 5.4 | 3.2 |
| D-Dimer (ng/mL FEU) | 90 - 530 | 400 |
| Ferritin (ng/mL) | 7 - 140 | 47 |
| Fibrinogen (mg/dL) | 200 - 400 | 303 |
| Triglyceride (mg/dL) | Under 75 | 70 |
| Cholesterol (mg/dL) | Under 100 | 94 |
| LDL (mg/dL) | Under 100 | 79 |
| HDL (mg/dL) | Greater than 45 | 54 |
| Anti-ds-DNA (units/mL) | Less than 170 | Negative |
| ANA | Less than 1/80 | Negative |
| Protein C (IU/dL) | 65 - 135 | NL |
| Protein S (IU/dL) | 49 - 150 | NL |
| Anti-thrombin 3 (%) | 80 - 130 | NL |
| Anti-smith (U) | < 1.0 (negative) | Negative |
| IL6 (pg/m) | Under 30 | NL |
| U/A | - | NL |
| PT (s) | 12.5 - 17 | 13 |
| PTT (s) | 25 - 30 | 25 |
| Lupus anti-coagulant (MPL) | 20 - 39 | Negative |
| Anti-cardiolipin (U/mL; GPL) | < 10 | < 10 |
| IgG (mg/dL) | 490 - 1610 | 407 |
| IgM (mg/dL) | 25 - 95 | 160 |
| IgA (mg/dL) | 34 - 305 | 57 |
| IgE (KU/L) | ≤ 307 | 90 |
| HSV PCR | < 0.9 | Negative |
Immediate management involved initiating ventilator support with high positive end-expiratory pressure (PEEP) to ensure adequate oxygenation and ventilation. Furosemide was administered to control pulmonary edema, and inotropic support along with Milrinone was provided to augment myocardial contractility and optimize cardiac output. Meropenem and Vancomycin were used for possible pneumonia, while Remdesivir, intravenous immunoglobulin (IVIG) therapy, and methylprednisolone pulse were initiated to modulate the immune response and control potential inflammatory processes contributing to the possible MIS-C, as the following day nasopharynx PCR revealed COVID-19 infection. Additionally, enoxaparin was administered to reduce the coagulation cascade.
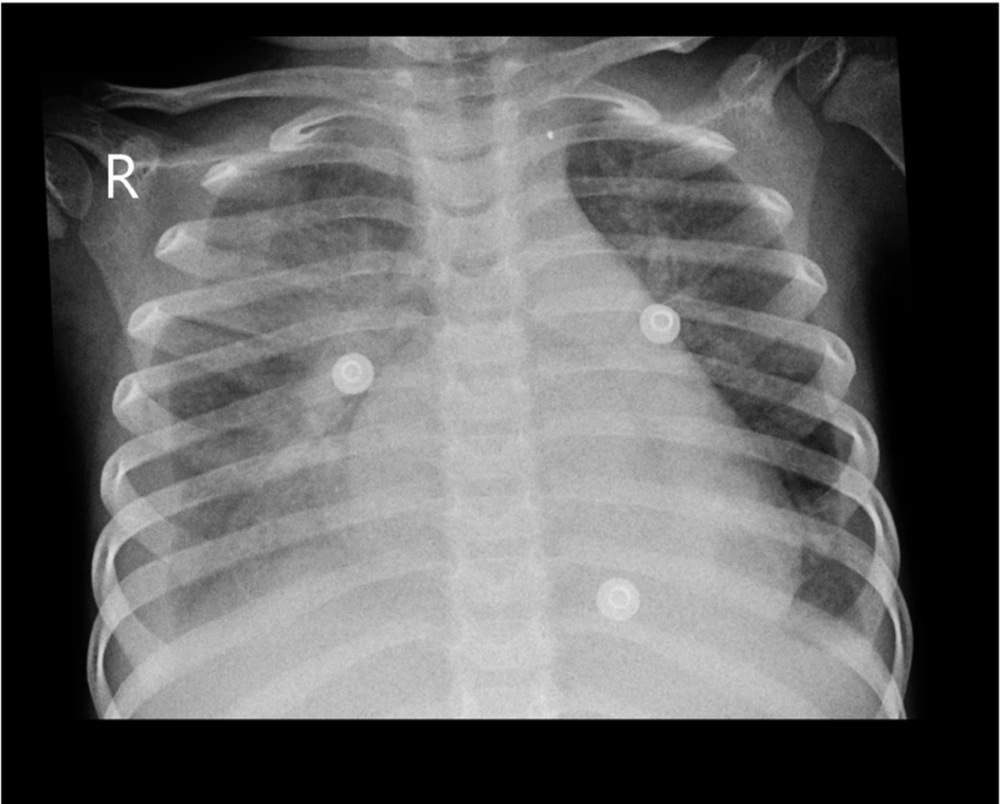
Over the course of treatment, the patient’s respiratory distress gradually improved, with stabilization of vital signs and oxygenation. Serial monitoring of cardiac function and fluid status guided adjustments in inotropic support and diuretic therapy. Repeat imaging demonstrated resolution of pulmonary edema and pleural effusion, indicative of a favorable response to treatment (Figure 1). The patient was successfully weaned off ventilator support. Laboratory findings are shown in Table 1. Cardiac function returned to normal, and the child remained in a stable hemodynamic situation.
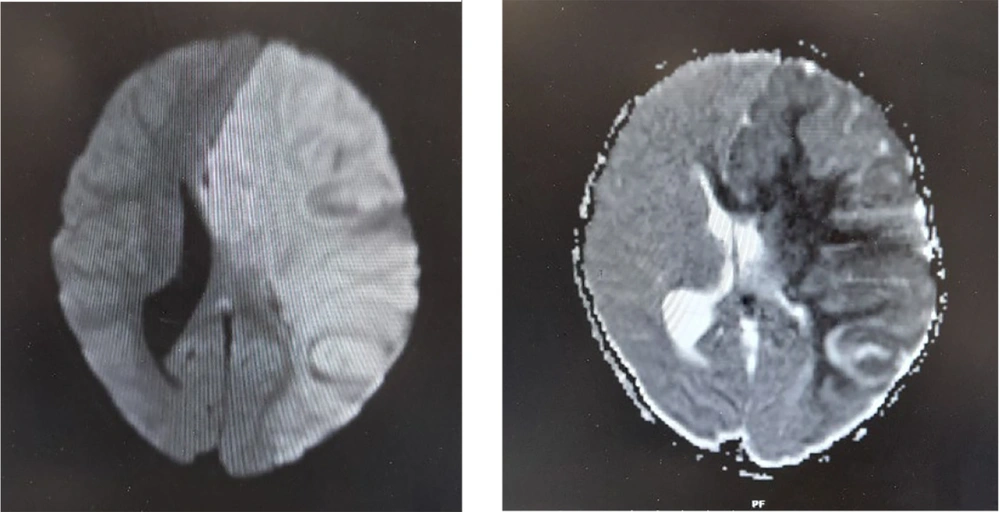
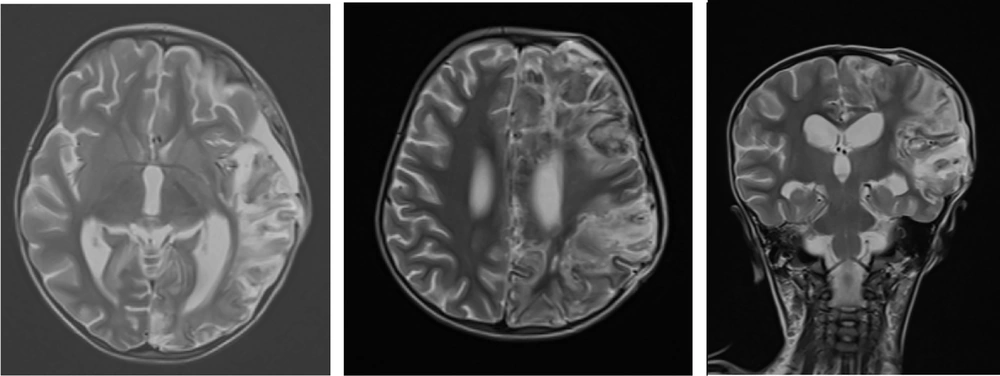
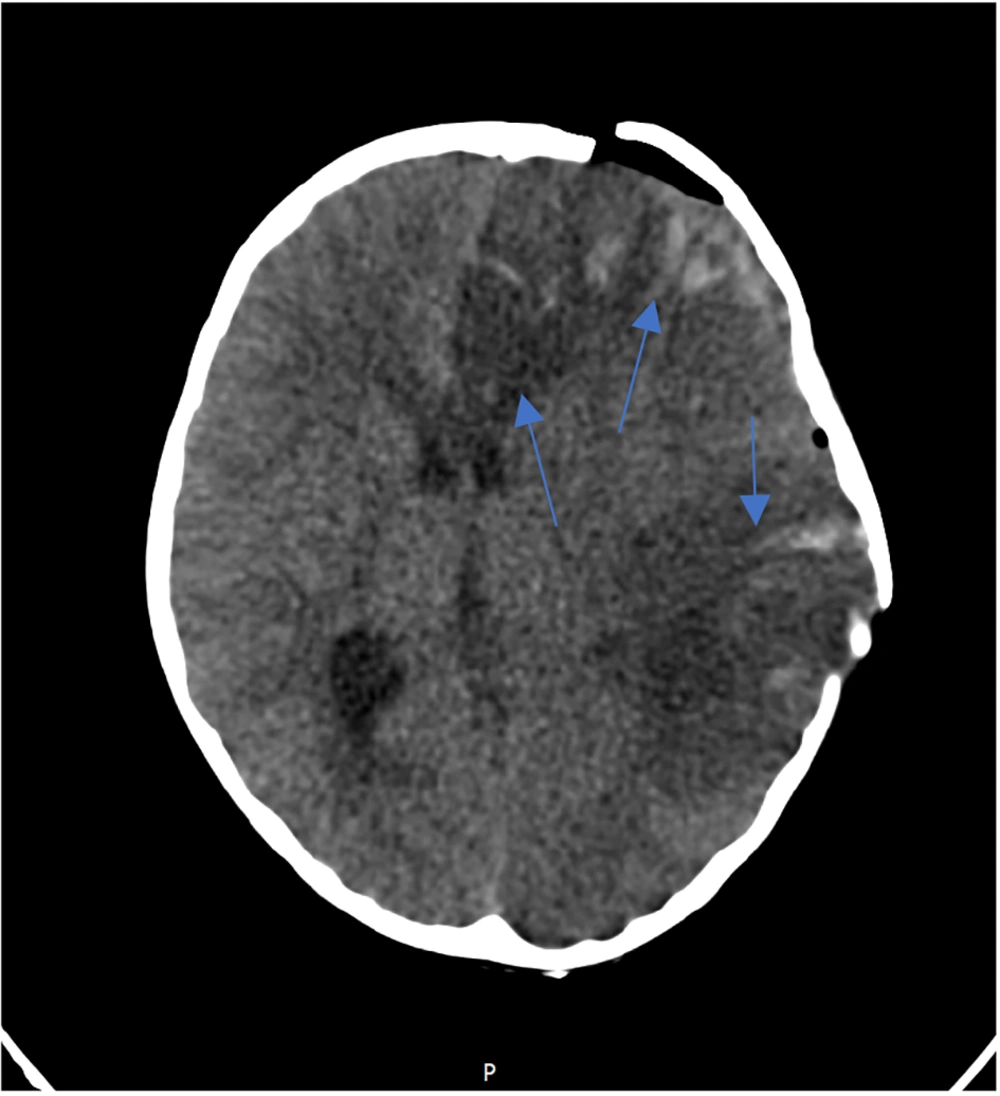
Three days after successful extubation, the patient demonstrated abnormalities in limb tone and force, as well as anisocoria. Brain MRI showed severe generalized edema, ischemia, and herniation (Figure 2). Antiepileptic drugs were started due to brain damage. Following a severe increase in intracerebral pressure, a craniotomy was performed, and supportive treatment continued. A brain biopsy showed inflammation and bleeding. MRA (Magnetic Resonance Angiography) showed a filling defect in the right vertebral artery. Post-craniotomy MRI reported mild herniation through the craniotomy site. An abnormal T2/FLAIR high signal was noted in the left cerebral hemisphere, left basal ganglia, and left thalamus as a sequel of infarction. Hemorrhagic changes in the left frontal lobe were seen, with multiple areas of gyral T1-high signal mostly suggestive of cortical laminar necrosis (Figure 3). There were no changes in favor of HSV in the MRI. Post-craniotomy CT scan showed parenchymal edema and hemorrhagic changes in the left frontal lobe, with abnormal hyper-dense foci noted in the genu and splenium of the corpus callosum and left caudate nucleus (Figure 4). The patient was diagnosed with cerebral stroke. CSF PCR for HSV from the brain biopsy, serum HLA B51, IgA, IgG, IgM, IgE, ANA, lupus anticoagulant, TG, cholesterol, HDL, LDL, pANCA, cANCA, anti-coagulant IgG and IgM, anti-cardiolipin IgG and IgM, protein C, protein S, anti-thrombin 3, F-ANA, anti-B2 glycoprotein, anti-DNase, IL-6, and anti-Smith were performed (Table 1).
As our neurosurgery consultants and hematology department consult indicated, the hyper-coagulation state had resulted in hemorrhage, and not only was anticoagulation therapy not contraindicated, but it was also a fundamental part of the treatment. Therefore, Enoxaparin was continued while palliative treatment was provided in the hospital. The patient was discharged with Aspirin and Levetiracetam. During follow-up, subsequent monitoring and management were conducted. The laboratory findings, including CBC, coagulation tests, and autoantibodies, were rechecked and all were within normal range. The patient is currently in a satisfactory state.
3. Discussion
This case highlights the pivotal role of expeditious identification and management of severe respiratory distress, cardiogenic shock, and neurological impairment in pediatric patients manifesting respiratory symptoms associated with the novel coronavirus (SARS-CoV-2). The therapeutic strategy encompassed early ventilator support with high PEEP, inotropic therapy, IVIG, methylprednisolone pulse therapy, enoxaparin, and diuretic therapy, in conjunction with antiviral therapy, which proved instrumental in stabilizing the patient's condition and facilitating recovery. A 7-year-old child was reported with COVID-19 right lung involvement from Iran (2022) with pleural effusion and normal cardiac function, who improved with treatment (7). Pleural effusion is relatively uncommon in patients with COVID-19 and is estimated to occur in 7.3% to 20% of cases. The mechanism involves direct viral invasion or parenchymal inflammation and increased interstitial fluid due to leaky microvasculature reaching the pleural space (8). In our case, decreased ejection fraction is another mechanism for the patient's pleural effusion. The pleural fluid was transudate. Myocardial involvement is an important aspect of organ involvement and is more common in MIS-C cases, with incidence ranging from 35% to 100%. The mechanism involves inflammation and dysfunction of the myocardium and damage to the coronary microvasculature. Interleukins, lymphocytes, and macrophages play an important role in its pathogenesis (9). A 9-month-old infant with fulminant myocarditis and acute COVID-19 was reported from Taiwan. He was treated with VA-ECMO and long-term intubation in the PICU, but hypoxic encephalopathy occurred despite supportive management (10). Two Mexican cases, aged 11 and 13 years, were reported with MIS-C, cardiogenic shock, and incomplete Kawasaki (2023), successfully treated with IVIG and supportive care (11). Despite cardiac function improvement, long-term morbidity may occur (9). A multicenter study in the USA in 2021 reported an incidence of 5% for severe neurologic complications in pediatric MIS-C.
Pathogenesis involves brain tissue endothelial injury and direct viral infection, resulting in para-infectious and post-infectious inflammation. Findings include encephalopathy, headache, febrile seizure, demyelination, ADEM, cerebral edema, and stroke (12). A 10-year-old girl was reported from Sanandaj, Iran, with seizure and COVID-19. Acute infarction occurred in the right putamen, globus pallidus, and posterior part of the insula. A small focal dilation in the left middle cerebral artery was observed. Risk factors for stroke include cardiac disease, sickle cell, prothrombotic disorders, cerebral vasculitis, cancer, and trauma. Certain infections such as mycoplasma, chlamydia, enterovirus, influenza A, Parvovirus 19, VZV, and COVID-19 may trigger a cytokine cascade that aggravates ischemic brain damage due to endothelial injury and brain vasogenic edema (13). A systematic review in the Philippines (2023) categorized pediatric ischemic stroke by COVID-19 into arterial and/or venous stroke, and sino-venous thrombosis. The clinical profiles and outcomes of patients reviewed support prior hypotheses that the virus can cause both vasculopathy and induce a derangement in the coagulation system, predisposing to ischemic strokes (14). Neurologic complications may occur in 11% to 30% of MIS-C cases (15). A rare case of subarachnoid hemorrhage (SAH) was caused by a ruptured vertebral artery (VA) dissecting aneurysm (DA) under severe COVID-19 treatment (16). Our case is diagnosed as brain stroke as a complication of MIS-C because other laboratory findings are normal and predisposing conditions are ruled out. Close monitoring and interdisciplinary collaboration are crucial in optimizing outcomes in such challenging cases. Table 1 presents the laboratory findings of a child with pulmonary, cardiac, and neurologic complications.
3.1. Conclusions
In conclusion, timely intervention and comprehensive management are imperative in addressing severe respiratory distress, cardiogenic involvement, and neurologic impairment in pediatric patients suffering from the catastrophic complications of COVID-19. This case emphasizes the need for a systematic approach, including supportive care along with pharmacological interventions such as early use of inotropes and IVIG alongside corticosteroids and enoxaparin, as well as close monitoring, to achieve successful outcomes in critically ill children with critical organ damage.