1. Background
Following kidney transplantation, both infectious and non-infectious gastrointestinal complications such as mouth sores, esophagitis, colitis, peptic ulcers, diarrhea, and even malignancies are likely to occur (1, 2). These complications are common in about half of kidney transplant recipients, with gastritis and peptic ulcers being particularly significant and observed with much greater severity in these patients (3, 4). Helicobacter pylori, a gram-negative microaerophilic bacterium that primarily accumulates in the stomach, is a major cause of chronic gastritis and peptic ulcers and can potentially lead to gastric cancer as well (5). Previous studies indicate a significant relationship between H. pylori infection and poor socioeconomic status (6, 7). The overall prevalence of this infection remains more than 30% to 50% (8). In renal transplant recipients, higher rates of gastric and duodenal mucosal lesions and H. pylori infection before transplantation may result from higher serum levels of urea, anemia, and fluctuations in gastric blood supply in the chronic renal failure state and during hemodialysis. Furthermore, after transplantation, the use of immunosuppressive drugs leads to hypogammaglobulinemia and reduces the optimal immune response against infections (9). Therefore, it is necessary to detect H. pylori infection before kidney transplantation and evaluate the effect of various treatments to eradicate it in these patients.
2. Objectives
This study aimed to determine the prevalence of H. pylori infection in pediatric kidney transplant patients after transplantation compared to before. Additionally, the factors related to the rate of infection in these patients were evaluated.
3. Methods
This was a case series cross-sectional study conducted as a before-and-after evaluation at Rasul-e-Akram and Ali Asghar hospitals in Tehran, Iran. In this study, 65 kidney transplant patients aged between 5 and 18 years were included from 2018 to 2022. Before transplantation, all patients underwent endoscopy, and an antral biopsy was taken to detect H. pylori. Patients who had H. pylori infection received eradication treatment; all transplanted patients were negative for H. pylori infection. Sequential therapy for H. pylori infection consisted of a proton pump inhibitor (PPI) plus amoxicillin for the first week, followed by a PPI plus metronidazole and clarithromycin for the second week. One to eight years after kidney transplantation, all patients were evaluated for H. pylori infection using the Urease Breath Test (UBT). A questionnaire was completed for all patients, including demographic characteristics, the type of disease that led to the transplant, the type of drugs used, and the duration after the transplant. Written consent was obtained from the parents and patients participating in the study. SPSS Statistics version 26 was used for statistical analyses. Descriptive variables were expressed as numbers and percentages; mean numeric variables were expressed as mean ± standard deviation (SD). The Mann-Whitney U test was used for comparisons before and after transplantation. The difference between categorical variables was tested with the chi-square (χ2) test. A P-value of less than 0.05 was considered statistically significant. The research was approved by the ethics committee of Iran University of Medical Sciences with the code number IR.IUMS.REC.1397.785 and was conducted in accordance with the Helsinki Declaration.
4. Results
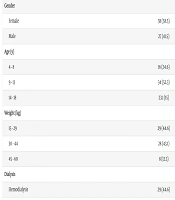
Among the 65 pediatric kidney transplant patients who participated in the study, 38 (58.5%) were girls and 27 (41.5%) were boys. Regarding the underlying diseases leading to renal transplant, the most common was reflux nephropathy with neurogenic bladder in 16 patients (24.61%). This was followed by hypoplastic kidney disease (21.53%), familial focal segmental glomerulosclerosis (FSGS) (21.53%), undetermined causes (21.53%), cystinosis (4.61%), nephronophthisis (4.61%), congenital nephrotic syndrome (3.07%), and autosomal recessive polycystic kidney disease (3.07%). The least common underlying diseases leading to kidney transplant were renal tubular acidosis (RTA), Alport syndrome, and chronic glomerulonephritis, each occurring in one patient (1.53%).
Before kidney transplantation, only one patient had not undergone dialysis. Of the other 64 patients, 29 (44.6%) had undergone hemodialysis, 16 (24.6%) had experienced peritoneal dialysis, and 19 (29.2%) had undergone both hemodialysis and peritoneal dialysis. In terms of the immunosuppressive drug regimen to prevent transplant rejection, all patients (100%) received mycophenolate mofetil (MMF). Additionally, 64 patients (98.46%) received tacrolimus, while only one patient (1.53%) received cyclosporine (Sandimmun) due to the occurrence of diabetes mellitus.
The two patients with positive UBT results after transplantation were new cases of H. pylori infection, and both received MMF and tacrolimus as immunosuppressive drugs. The duration since kidney transplantation varied from 1 to 8 years, with the majority of cases (23.07%) evaluated two years post-transplant for H. pylori, and only one patient (1.53%) evaluated 7 and 8 years post-transplant. The duration of dialysis before transplantation was less than one month in 22 patients, more than 36 months in 11 cases, and between 1 to 36 months in the remaining patients (Table 1).
| Parameters | No. (%) |
|---|---|
| Gender | |
| Female | 38 (58.5) |
| Male | 27 (41.5) |
| Age (y) | |
| 4 - 8 | 16 (24.6) |
| 9 - 13 | 34 (52.3) |
| 14 - 18 | 23.1 (15) |
| Weight (kg) | |
| 15 - 29 | 29 (44.6) |
| 30 - 44 | 28 (43.1) |
| 45 - 60 | 8 (12.3) |
| Dialysis | |
| Hemodialysis | 29 (44.6) |
| Peritoneal | 16 (24.6) |
| Hemo-peritoneal | 19 (29.2) |
| None | 1 (1.5) |
| Immunosuppressive drug | |
| MMF + Cyclosporine | 1 (1.5) |
| MMF + Tacrolimus | 64 (98.4) |
Out of 65 patients evaluated before transplantation by antral biopsy, 8 had H. pylori infection, resulting in a prevalence of 12.3%. After transplantation, only 2 (3.1%) had a positive UBT. The prevalence of Helicobacter infection before and after transplantation did not show a significant difference between sexes, with p-values of 0.301 and 0.644, respectively. Additionally, there was no relationship between age and the presence of Helicobacter infection before and after kidney transplantation, with P-values of 0.547 and 0.474, respectively.
5. Discussion
In this study, the incidence of H. pylori infection in pediatric renal transplant patients was 3.1% after transplantation and 12.3% before transplantation. A study by Cheungpasitporn et al. showed that between 1990 and 2000, the estimated prevalence of H. pylori infection in transplant patients was 50%, with 46% in developed countries and 55% in developing countries. Between 2000 and 2016, the incidence of infection decreased to 35%, with 28% in developed countries and 45% in developing countries. In general, the relative risk of infection in transplant patients was reported as 0.57 (10).
In the study by Bunchorntavakul and Atsawarungruangkit, 107 patients with end-stage renal disease were evaluated. Positive esophagogastroscopic findings were observed in 46% of patients, mainly in the form of erosive gastroduodenitis and peptic ulcers. The prevalence of H. pylori infection in these patients was 27.1% (11).
In the study by Hooman et al. in 2011, data from 117 children aged 5 to 18 years with end-stage renal disease who underwent renal transplantation were evaluated. Gastrointestinal symptoms were reported in 12% of children, and H. pylori infection was reported in 24% of children (12).
In the study by Cocchiara et al., patients with ESRD who were candidates for kidney transplantation underwent esophagogastroduodenoscopic evaluation to rule out H. pylori infection. In total, 32 patients were affected by H. pylori infection (52.4%) (13).
In a multicenter prospective cohort study on adult chronic kidney disease patients, Maioli et al. demonstrated a high prevalence (61.4%) of H. pylori and a low eradication rate after long-term treatment (48.5%). However, in our study, the total prevalence of H. pylori was lower (12.3%), and the eradication rate was higher (14). The prevalence of H. pylori in our study decreased after transplantation despite immunosuppressive treatment. Higher rates of H. pylori infection before transplantation may have resulted from higher serum levels of urea, anemia, and fluctuations in gastric blood supply in the chronic renal failure state and hemodialysis. The decreased rate of H. pylori infection after transplantation in this study is related to the correction of the uremic state and anemia and improved gastric blood supply.
In another study conducted on 61 adult renal transplant candidates in Turkey, 14% of patients were H. pylori positive. The infection was closely associated with the presence of peptic ulcers in these patients' endoscopy (15).
5.1. Conclusions
Due to uremia, anemia, and fluctuations in gastric blood supply before transplantation, and the use of immunosuppressive drugs after transplantation, it is recommended to evaluate pediatric renal transplant recipients for H. pylori and treat infected patients both before and after kidney transplantation.