1. Introduction
Basidiobolomycosis is a rare fungal infection caused by the saprophytic fungus Basidiobolus ranarum, which naturally thrives in soil, decomposing plant matter, and the gastrointestinal tracts of reptiles, amphibians, and certain mammals (1, 2). Transmission typically occurs through contact with infected soil, organic material, gecko secretions, or via minor skin abrasions, particularly in warm and humid tropical or subtropical regions (3). Although subcutaneous basidiobolomycosis was previously the most reported type, there has been a concerning rise in gastrointestinal basidiobolomycosis (GIB) in recent years (4, 5). This more severe and invasive condition, particularly seen in children, underscores the need for early diagnosis and treatment in regions where the fungus is endemic to prevent serious health complications (5, 6).
Gastrointestinal basidiobolomycosis poses considerable diagnostic challenges due to its nonspecific and overlapping symptoms, which can mimic conditions like inflammatory bowel disease (IBD), intestinal tuberculosis, appendicitis, or gastrointestinal malignancies (7, 8). Commonly reported symptoms include abdominal pain, fever, weight loss, and eosinophilia, often accompanied by mass formation or signs of intestinal obstruction (9). Histopathological evaluation plays a pivotal role, often revealing features such as granulomatous inflammation, necrosis, and fungal hyphae surrounded by eosinophilic material, known as the Splendore-Hoeppli phenomenon (6, 10, 11). A delayed diagnosis can lead to severe complications like intestinal perforation or abscess formation, emphasizing the need for heightened clinical vigilance in endemic regions (2, 5, 12).
This case of an 11-year-old boy with GIB highlights the complex diagnostic and therapeutic challenges associated with this illness. Initially misdiagnosed with IBD and lymphoma, the true diagnosis of basidiobolomycosis was confirmed only after comprehensive diagnostic evaluations, including imaging and pathology. By detailing this case, we aim to stress the significance of early diagnosis and intervention in managing fungal infections, especially in endemic regions, to reduce complications and improve patient recovery.
2. Case Presentation
An 11-year-old boy presented with an 8-month history of abdominal pain, bloody diarrhea, significant weight loss, and generalized weakness. Ulcerative lesions were discovered during the initial diagnostic workup through colonoscopy, leading to an initial diagnosis of IBD. Treatment was initiated with prednisolone and anti-TNF therapy (Infliximab). However, his symptoms persisted, with ongoing fever, abdominal pain, and worsening anemia, despite this therapeutic approach. This necessitated further investigation into the etiology of his persistent problems.
At a secondary care center, imaging studies revealed a large retroperitoneal mass originating from the kidney, encircling the aorta and inferior vena cava (IVC), and causing bilateral hydronephrosis by compressing the ureters. A bone scan indicated areas of hyperactive uptake in the L3-L5 vertebrae and the right proximal radius, raising suspicion of metastatic involvement. Bone marrow biopsy excluded hematologic malignancies, and MRI with contrast further ruled out infiltrative tumors in these regions. A CT-guided biopsy of the kidney lesion demonstrated necrotizing inflammatory changes without evidence of malignancy. Histopathological analysis of the biopsy confirmed basidiobolomycosis, a rare fungal infection. Due to the inability to perform surgical intervention at this facility, the patient was referred to our hospital for definitive diagnosis and management.
2.1. Investigations
Initial laboratory and imaging investigations were conducted to assess the underlying cause of the patient’s symptoms and complications.
2.2. Laboratory Findings
The laboratory findings demonstrated the following:
- Severe anemia (Hb: 5.8 g/dL), hypoalbuminemia (Alb: 3.2 g/dL), leukocytosis (WBC: 25.1 × 109/L), and elevated C-reactive protein (CRP: 91 mg/L).
- Despite significant hydronephrosis, renal function remained normal (creatinine: 0.7 mg/dL).
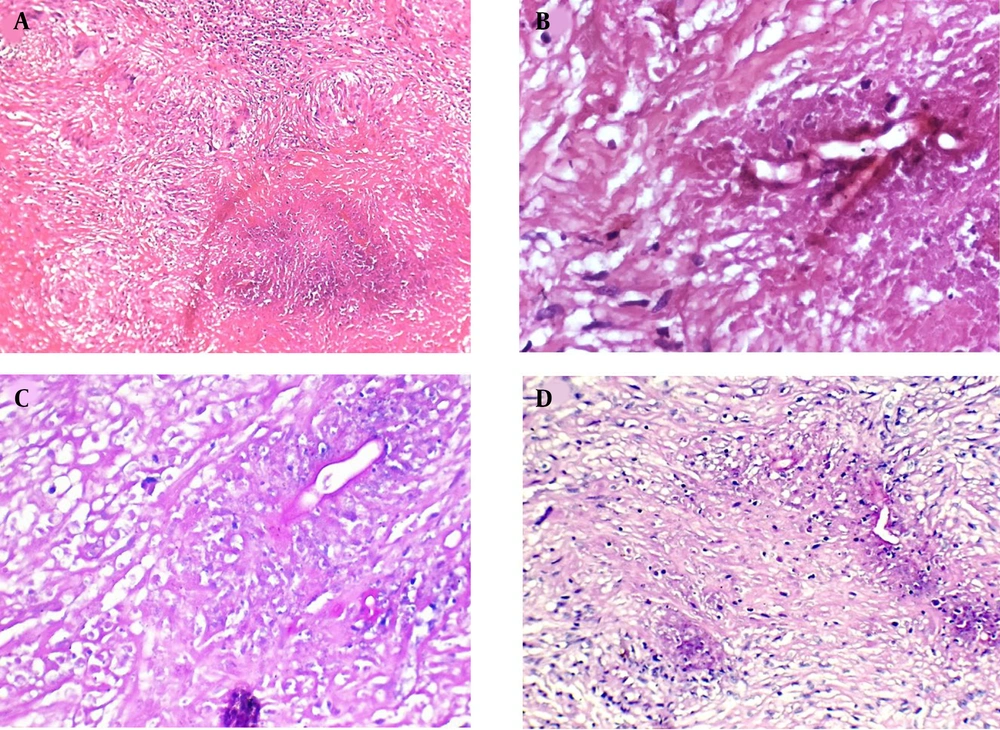
2.3. Histopathology
A biopsy from the kidney lesion performed at the secondary facility revealed necrotizing granulomas with broad fungal hyphae. Periodic acid-Schiff (PAS) and PAS-diastase (PAS-D) stains confirmed the presence of fungal components, leading to the diagnosis of basidiobolomycosis.
2.4. Imaging Studies
2.4.1. Ultrasonography
Bilateral moderate hydronephrosis with pelvic anteroposterior diameters of 17 mm (right) and 14 mm (left) due to compression of the ureters by the retroperitoneal mass.
2.4.2. Venous Doppler Ultrasound
Acute thrombosis in the left common femoral vein (CFV), superficial femoral vein (SFV), and iliac veins, with collateral venous dilation manifesting as variceal vessels throughout both legs, attributed to impaired venous return caused by the mass effect.
2.4.3. Spiral Abdominal CT Scan
A large retroperitoneal mass encasing the aorta, IVC, superior mesenteric artery (SMA), and ureters (Figure 1). Thrombosis extended into the IVC and right iliac vein, with moderate bilateral hydronephrosis.
2.4.4. MRI
Retroperitoneal mass measuring 38 × 31 mm encasing major vessels and ureters, with persistent hydronephrosis.
2.5. Surgical Intervention
The patient underwent an exploratory laparotomy to assess the retroperitoneal mass. During the procedure, the mass was found to be fibrotic and extensive, with adhesions involving the aorta, IVC, and adjacent structures such as the ureters, kidneys, and surrounding lymphatic tissues, rendering complete resection unfeasible. A biopsy was taken during the operation, and the abdomen was subsequently closed. Histopathological examination of the specimen verified basidiobolomycosis, consistent with previous diagnoses (Figure 2).
2.6. Treatment and Clinical Outcome
The patient was treated with an extensive antifungal and antibiotic regimen, including amphotericin B for 12 days, voriconazole for 12 days, and adjunct antibiotics such as meropenem for 12 days and vancomycin for 7 days. Initial treatment with itraconazole was attempted but discontinued due to disease progression and a lack of clinical response, necessitating a switch to alternative antifungal agents. Bilateral double-J (DJ) stents were inserted to manage hydronephrosis resulting from ureteral compression by the retroperitoneal mass. Despite the procedure, the obstruction persisted due to the ongoing mechanical pressure exerted by the mass.
Enoxaparin was initiated as anticoagulation therapy to manage thrombosis identified in the left common femoral, superficial femoral, and iliac veins. Post-discharge, follow-up monitoring of anti-Xa levels was planned to ensure the efficacy of anticoagulation therapy. At the time of admission, the patient was febrile, unable to tolerate oral intake, and had a firm abdomen on examination. Following the initiation of antifungal therapy, anticoagulation, and supportive care, the fever resolved completely. Gastrointestinal symptoms improved markedly, allowing the patient to return to a full oral diet. Abdominal examination findings normalized, transitioning from a firm and tense state to soft by the time of discharge.
Despite the administration of nephrotoxic medications such as amphotericin B and voriconazole, renal function remained stable, demonstrating the effectiveness of comprehensive monitoring. Although the retroperitoneal mass could not be resected due to severe adhesions to vital structures, the patient showed notable clinical improvement. The patient was discharged with ongoing antifungal therapy and anticoagulation, and a comprehensive follow-up plan was established to monitor thrombosis resolution, renal function, and the response of the mass to continued treatment.
3. Discussion
Gastrointestinal basidiobolomycosis, caused by the fungus B. ranarum, represents a rare infectious disease associated with contact with contaminated soil or organic matter (1). This infection predominantly affects children living in tropical and subtropical zones and is frequently underdiagnosed due to its nonspecific presentation (4, 5). Presenting with prolonged abdominal pain, colonic ulcerative lesions, and systemic manifestations like fever and weight loss, the patient was initially diagnosed with IBD, specifically Crohn's disease, and treated with anti-TNF therapy due to unresponsiveness to common treatment. A considerable overlap in symptoms between GIB and IBD has been thoroughly documented, with diagnostic delays often worsening morbidity (3, 13).
In this case, the imaging findings introduced further complexity to the diagnostic process. The presence of a large retroperitoneal mass, bilateral hydronephrosis, and vertebral lesions raised suspicion for lymphoma, highlighting a common diagnostic pitfall in GIB cases (10, 14). Hypermetabolic activity observed in the L3-L5 vertebrae and proximal radius initially raised concerns for potential metastatic disease. These findings align with documented cases where GIB mimics neoplastic or granulomatous diseases, often delaying appropriate treatment (15, 16). Unresponsive symptoms, coupled with inconclusive imaging findings, prompted an exploratory laparotomy, underscoring the challenges in diagnosing such a rare condition (7).
Histopathological confirmation remains pivotal in diagnosing GIB, as demonstrated in this case. Biopsy findings showed necrotizing granulomas containing fungal hyphae surrounded by the Splendore-Hoeppli phenomenon, indicative of basidiobolomycosis (6, 10). The application of PAS and GMS stains was crucial in diagnosing basidiobolomycosis, as these techniques helped detect fungal elements and ruled out malignancies or chronic inflammatory conditions (3, 14). These findings underscore the importance of histopathological evaluation in cases where imaging and clinical characteristics are inconclusive, as it provides definitive confirmation of the diagnosis (2).
Antifungal therapy remains the foundation of GIB management, and while itraconazole has been traditionally used, recent evidence suggests that liposomal amphotericin B and voriconazole are more effective for invasive cases, especially those involving vascular or retroperitoneal complications (17, 18). In our patient, itraconazole was discontinued due to unresponsiveness, requiring a switch to amphotericin B and voriconazole, a regimen consistent with alternative therapies described in the literature (7, 13). Following voriconazole treatment, a significant reduction in the retroperitoneal mass was observed, validating its effectiveness. However, extended treatment and vigilant observation remain crucial to achieve complete resolution and address potential recurrence (4, 5). The successful preservation of renal function despite nephrotoxic treatment, particularly in the context of hydronephrosis, highlights the importance of vigilant monitoring and tailored management (7).
The complications associated with GIB in this case were significant. Despite the placement of bilateral DJ stents, hydronephrosis persisted, as the obstruction was due to mechanical compression from the retroperitoneal mass rather than functional obstruction. Hydronephrosis resulting from ureteral compression is also observed in abdominal GIB and typically requires surgical or urological management (5, 19). Additionally, the patient developed venous thrombosis in the iliac and femoral veins, accompanied by collateral variceal vessels, a rare but serious complication potentially attributable to mass effect (20). Anticoagulation therapy with enoxaparin was initiated, with plans for post-discharge follow-up to check anti-Xa levels, aligning with management protocols reported in previous cases (18).
The environmental conditions of Yazd, a hot and arid city in the central region of Iran, likely played a key role in the patient’s infection (14). Soil, a recognized reservoir for B. ranarum, likely served as the source of exposure, reflecting findings from comparable cases in endemic regions (9, 11). Public health awareness in endemic regions remains crucial to reduce the risk of soil-borne infections, particularly in children who are more likely to have frequent soil contact.
This case provides an important contribution to understanding GIB, highlighting its diagnostic challenges and mimicry of IBD and malignancies. The inclusion of skeletal involvement, vascular complications, and unrelenting mass effect underlines an expanded spectrum of GIB characteristics documented in the literature. This underscores the critical importance of early diagnosis through histopathology and the necessity for tailored therapy to effectively manage complications. Future research should prioritize developing advanced diagnostic tools for earlier detection, refining antifungal therapy protocols, and investigating adjunctive treatments to improve outcomes in this rare yet significant disease.