1. Introduction
Pediatric nephrolithiasis, or kidney stones in children, is a significant health concern worldwide. Although there is no precise global prevalence data, the prevalence in the United States is reported to be approximately 0.1% (1). Recurrent nephrolithiasis is more common in pediatric patients than in adults (2). Management of recurrent nephrolithiasis includes dietary modification, supportive care, drug therapy, and surgical procedures (3).
Hydatid cyst is an uncommon medical condition resulting from Echinococcosis infection (4). Echinococcus enters the human body via the oral route and can affect various organs, most commonly the liver and lungs (5). This infection is endemic in regions such as South America, the Middle East, Asia, the Mediterranean, and East Africa (6). Although exact incidence rates are unavailable, Brunetti et al. reported in 2010 that the incidence rate in endemic areas was approximately 0.0005 persons annually (7). Hepatic hydatidosis is the most common form, followed by pulmonary hydatidosis (8). Many cases of pulmonary hydatidosis are asymptomatic and are incidentally diagnosed via chest X-ray CXR (9).
Partial anomalous pulmonary venous connections (PAPVC) encompass a range of congenital heart anomalies characterized by the abnormal drainage of one or more pulmonary veins into the right atrium, either directly or via systemic veins, while not all pulmonary veins are affected (10). The PAPVC is a rare cardiac anomaly, with an incidence of less than 1% of all cardiac disorders (11). In this report, we present a 6-year-old boy with recurrent nephrolithiasis episodes who was incidentally diagnosed with pulmonary hydatidosis. During pre-surgical evaluations, a sinus venosus atrial septal defect (ASD) and PAPVC were also diagnosed.
2. Case Presentation
A 6-year-old boy was referred to our nephrology clinic for the treatment of nephrolithiasis, with a history of undergoing ultrasound shock wave therapy twice for previous episodes. In the most recent episode, the patient had a stone measuring 6 millimeters (mm) in diameter, which was reduced to 4 mm following ultrasound shock wave therapy, but it did not pass. The patient experienced prolonged fever for 40 days, flank pain, and vomiting. His mother also reported occasional mild coughs. A urine analysis (U/A) was performed, and a urinary tract infection (UTI) with Pseudomonas aeruginosa was diagnosed, leading to a 10-day hospitalization for treatment.
A few days later, the patient returned to our clinic with fever, abdominal pain, and dysuria. Physical examination revealed no significant findings. Urine analysis was conducted, revealing P. aeruginosa resistant to all antibiotics. The patient was admitted, and treatment with meropenem was initiated. Further evaluation, including a voiding cystourethrogram (VCUG) (Figure 1), revealed high-grade right urinary reflux. A dimercaptosuccinic acid (DMSA) scan showed significantly reduced size and contrast uptake in the right kidney. Laboratory data are presented in Table 1.
| Tests | Results |
|---|---|
| WBC | 6700 - 8700 |
| Serum neutrophil | 30% |
| Serum lymphocyte | L 60% |
| Hemoglobin | 11.1 - 12.8 |
| Platelet | 300000 - 474000 |
| BS | 104 |
| CRP | 1 - 6 |
| ESR | 12 - 20 |
| BUN | 6.6 - 20.6 |
| Creatinine | 0.57 - 0.59 |
| Sodium | 138 |
| Potassium | 4.7 |
| Calcium | 10.3 |
| Phosphorus | 5 |
| Uric acid | 2.7 |
a First urine analysis: Appearance: Clear, SG: 1010, PH :7, Protein: Negative, WBC: 60 - 70, RBC: 1 - 3, EP cell: 2 - 3, Blood: Negative, Bacteria: Few. First U/C: Colony count > 100000 P. aeruginosa.
b Second urine analysis: Appearance: Clear, SG: 1025, PH :5, Protein: Negative, WBC: Many, RBC: 1 - 3, EP cell: 1 - 2, Blood: Negative, Bacteria: Negative; Second U/C: Colony count = 30000 P. aeruginosa.
c Urine analysis before surgery: Appearance: Clear, SG: 1030, PH :7, Protein: Negative, WBC: 6 - 8, RBC: 0 - 1, EP cell: 1 - 2, Blood: Negative, Bacteria: Negative; U/C before surgery: Negative.
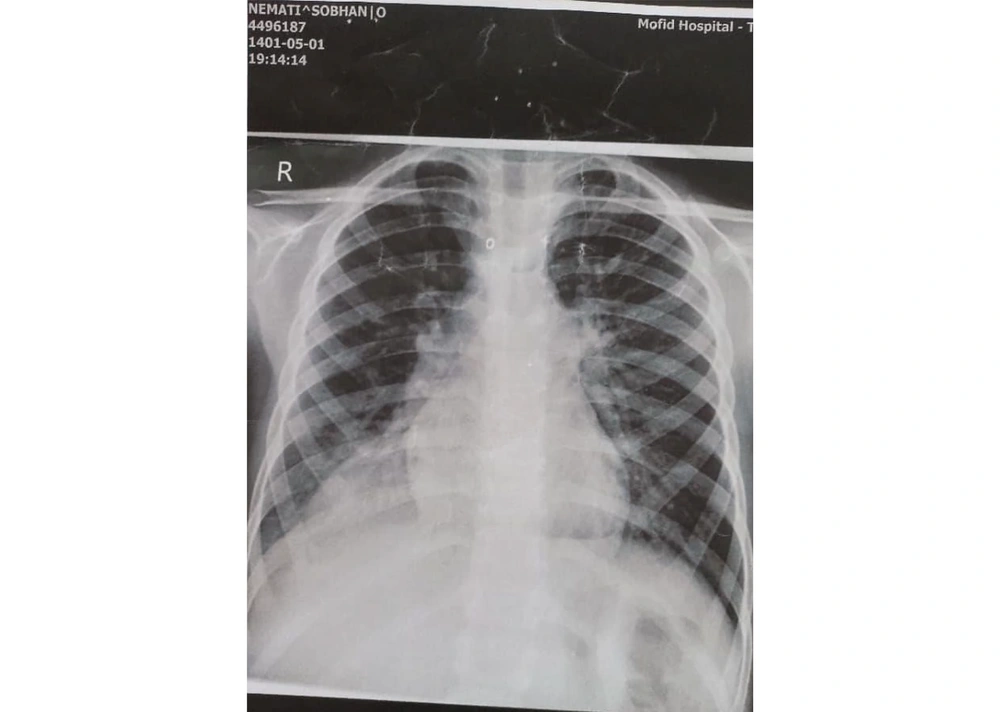
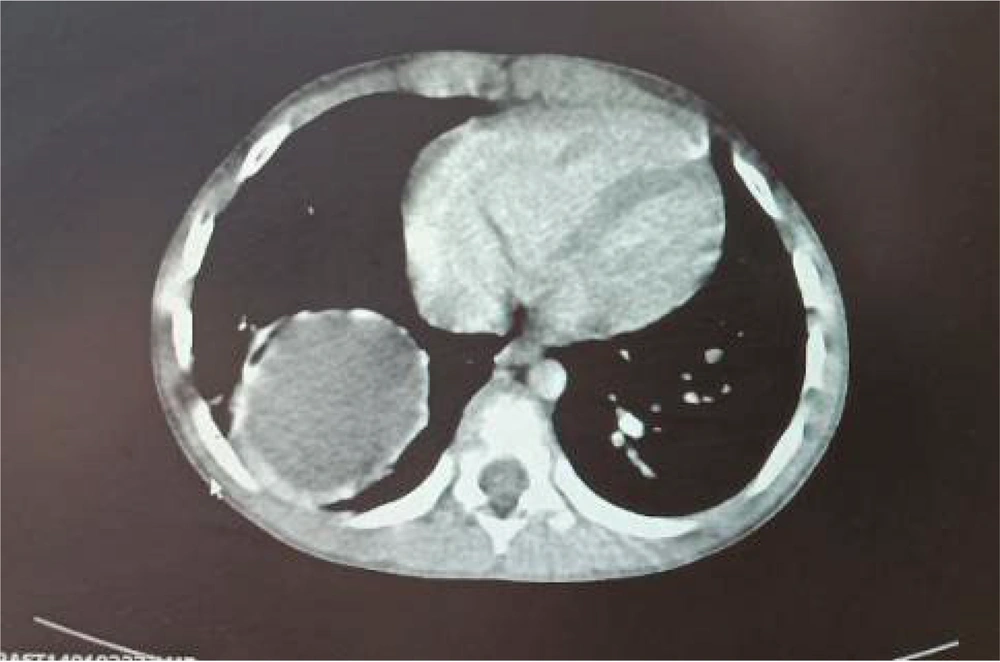
Chest and abdominal X-rays were performed to evaluate the abdominal pain and cough. The CXR revealed a suspicious lung finding (Figure 2). A computed tomography (CT) scan was requested to assess the lung lesion, and a hydatid cyst was incidentally diagnosed in the right lower lobe (Figure 3). The patient was treated with antibiotics for the UTI, and pre-surgical evaluations for the hydatid cyst were conducted. A cardiac consultation revealed mild pulmonary hypertension (systolic pulmonary arterial pressure: 40 - 45 mmHg), right ventricular dilation, right atrial dilation, and moderate tricuspid regurgitation on echocardiography. The CT angiography confirmed the diagnosis of PAPVC.
Following this finding, a history of exertional chest pain or other cardiac symptoms was obtained from the parents, with no positive history of clinical cardiac involvement. After treating the UTI, the patient underwent cardiac surgery, and the hydatid cyst was resected. The patient was discharged in good condition.
3. Discussion
In this report, we present a 6-year-old boy with a history of recurrent nephrolithiasis and UTI. His mother also reported occasional coughs during admission. A CXR revealed a doubtful halo, prompting a lung CT scan, which diagnosed hydatidosis. During preparation for hydatidosis surgery, cardiac abnormalities were found on the electrocardiogram, leading to a diagnosis of PAPVC. The patient had no complaints related to cardiac function; both hydatidosis and PAPVC were incidentally diagnosed.
Recurrent nephrolithiasis occurs in 50% of pediatric patients with a history of nephrolithiasis. Risk factors include a positive family history, gout, renal dysfunction, certain antibiotics, and diseases such as arthritis. The most common complication of nephrolithiasis is UTI (12, 13).
Hydatid cysts are caused by Echinococcus granulosus and are common in individuals involved in farming or husbandry, with transmission via the fecal-oral route. Pulmonary involvement is more common in children than adults, particularly in the lower lobes and especially the right lobe. Patients may be asymptomatic, with common clinical manifestations including chest pain, hemoptysis, and cough (14, 15). Our patient had a hydatid cyst in the right lower lobe of the right lung and was asymptomatic, with only occasional coughs reported by his mother.
Data on the incidence rates of hydatidosis are regional. A study by Saghafipour et al. reported an incidence rate of 6.81 per 100,000 people over 8 years (16). Mustapayeva et al. found the incidence rate of hydatidosis in Kazakhstan from 2007 to 2016 to be ≤ 0.1% (17). Simple chest radiography (CXR) is the first diagnostic modality for pulmonary hydatidosis. If findings are inconclusive, a pulmonary CT scan can aid in detection (18). We observed a halo in the CXR of our case, prompting a CT scan that confirmed pulmonary hydatidosis. Surgery is the main treatment for pulmonary hydatidosis, with the surgical technique depending on factors such as cyst location, surgeon’s decision, and cyst wall tissue (19, 20). Our case underwent surgery for lung hydatidosis.
During surgical preparation, an echocardiogram was performed to assess cardiac function, revealing abnormalities. The CT angiography identified cardiac abnormalities, including a sinus venosus ASD and PAPVC. Clinical manifestations of PAPVC vary widely, depending on the degree of vessel involvement and associated cardiac defects. It is often accompanied by other congenital cardiac conditions, such as Turner’s syndrome or ASD. Isolated PAPVC typically lacks clinical manifestations (21). Our patient had no history of cardiac symptoms.
The main treatment for sinus venosus ASD and PAPVC is surgery, although patients may be monitored and surgery performed if cardiac symptoms develop (22). In our case, lung surgery was necessary due to hydatidosis, and cardiac surgery was indicated. The patient underwent surgery, successfully treating both PAPVC and hydatidosis.
3.1. Conclusions
We report a boy with recurrent nephrolithiasis who was incidentally diagnosed with a hydatid cyst, sinus venosus ASD, and PAPVC. Attention to patient history, even seemingly insignificant details, can lead to important diagnoses. Hydatid cysts and cardiac anomalies may be asymptomatic and discovered incidentally during examinations.