1. Introduction
Adverse reactions after Bacillus Calmette-Guerin (BCG) vaccination include regional lymphadenopathy and pustule formation at the injection site; which can persist for as long as 3 months after vaccination. More serious local reactions include ulceration at the vaccination site, regional suppurative lymphadenitis with sinus formation or purulent draining at the puncture site. These manifestations might occur up to 5 months after vaccination and could persist for several weeks. The intensity and duration of the local reaction depends on the depth of penetration of the multiple puncture device and individual variations in patients' tissue reactions. Other post vaccinal cutaneous lesions include Tuberculosis (TB) chancre, Lupus vulgaris, Scrofuloderma, Papulonecrotic tuberculids. Severe adverse reactions such as osteitis, disseminated BCG disease were reported after vaccination (1).
Lupus vulgaris is one type of skin involvement with Mycobacterium TB, but the incidence of lupus vulgaris after BCG immunization is very rare, estimated to be approximately 1 per 100000 to 200000 vaccinations (2, 3).
This form of cutaneous TB may present with persistent and progressive reddish-brown papules or nodules with a gelatinous consistency (called apple-jelly nodules because of yellowish-green color on diascopy) followed by scar formation (3). We present a 13 month-old boy with a large lesion after single BCG vaccination, which was confirmed by Polymerase Chain Reaction (PCR). Genetic susceptibility may affect on BCG-induced LV (4). Our patient was a known case of trisomy 9. Since we did not find any published report about relationship between LV and trisomy 9, we do not have any knowledge about difference between LV in healthy children and children with trisomy 9.
2. Case Presentation
A 13-month-old boy presented with an extending plaque on his right upper arm and shoulder for a year. He had received BCG vaccine on his right arm on the day after his birth. The lesion appeared a month later as a small papule at the injection site that enlarged gradually changing to an erythematous, edematous plaque. His medical history was positive for trisomy 9. He was afebrile. clinical examination revealed a 20 - 25 cm infiltrated plaque with reddish-brown nodules that showed apple-jelly appearance on diascopy. This plaque has extended from right upper arm to right shoulder and to the anterior part of right hemithorax (Figures 1 and 2).
There was no regional or generalized lymphadenopathy or BCG adenitis. Results of laboratory tests were: WBC 18110/mm3, Neut 62%, Lymph 30%, Mono 7.5% and Eos 0.3%, Hb 10 mmol/L, and platelet count was 241000/mm3. ESR was 13 mm/h, CRP +.
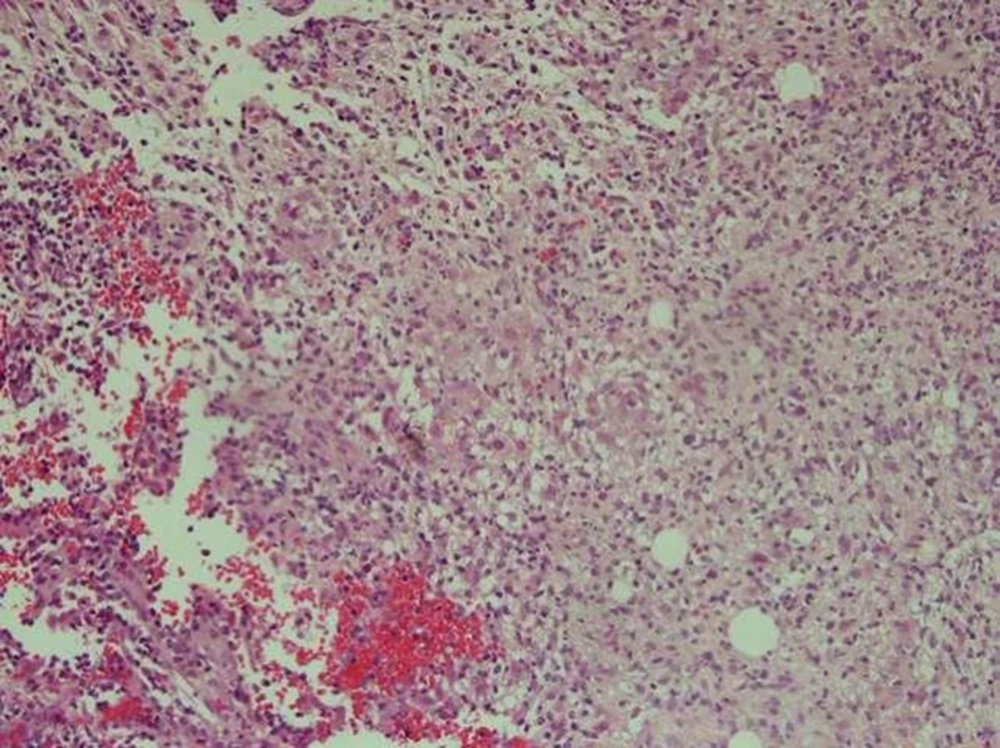
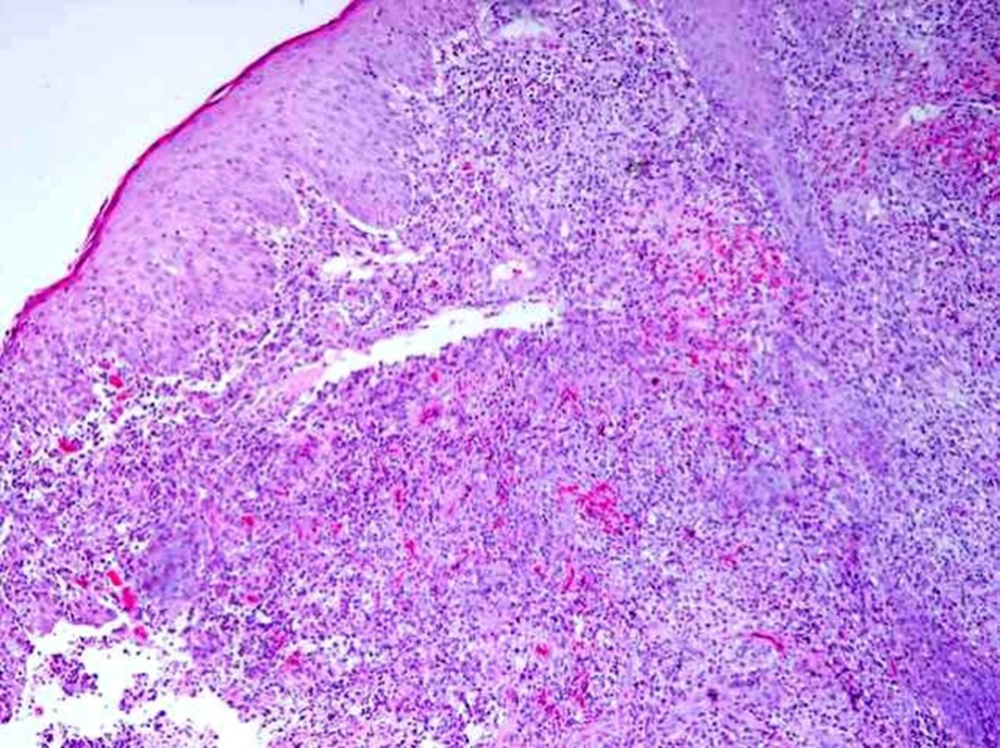
Wound culture grew staph coagulase negative that considered to be skin contamination. No Mycobacterium was seen in acid fast staining and culture. Smear and culture were negative for fungi. Immunological evaluation was done with following results: IgM, IgA, IgG were 90, 178, 590 g/L, respectively and IgE was 1 IU/mL. CD4 was 22.65% and CD8 22.87%, NBT was 100% and HIV was negative. The diameter of induration after Tuberculin Skin Test (TST) was about 20 mm at 72 hours. Chest X-ray was normal. Histopathological examination revealed tuberculoid granulomas consisting of epithelioid histiocytes, plasmocytes, and langerhans giant cells in the papillary dermis and also suppurative granuloma suggestive of LV. No acid fast bacillus was detected in Ziehl-Neelson and PAS staining (Figures 3 and 4).
The diagnosis of LV was confirmed in our patient using the PCR for Mycobacterium bovis in dermis. Lupus vulgaris could be differentiated from suppurative local lesion by prolonged duration (more than several weeks), skin lesion distinct from the vaccination site, apple-jelly appearance, absence of regional lymphadenopathy, and also histopathologic data. Therefore, treatment with anti-TB drugs was started. The patient was treated with Isoniazid (INH), Rifampin (RIF), Ethambutol (ETM). After two months, the lesion showed marked improvement.
3. Discussion
BCG immunization has some complications include: Local reaction such as axillary or cervical lymphadenopathy, local subcutaneous abscess and keloids, skin lesions distinct from the vaccination site such as TB chancre, lupus vulgaris, scrofuloderma, papulonecrotic tuberculids, and BCG-osis in immunocompromising diseases such as Chronic Granulomatous Disease (CGD), T-cell dysfunction, and impairment of IL12 and gamma interferon (2). Lupus vulgaris is a rare skin complication of the BCG vaccine and is presented by reddish brown plaque with apple-jelly nodules occur usually on the face and neck. Skin biopsy shows accumulations of epithelioid histiocytes with Langerhans giant cells and varying amount of caseation necrosis in the center; however, the absence of caseation necrosis may not rule out the diagnosis of TB (5). Prevalence of LV is 1 per 100000 to 200000 vaccinations (3, 6). Incidence of LV increases by multiple vaccinations (7). Our patient had received a single BCG vaccine. Lupus vulgaris is a progressive form of TB. It might be caused by hematogenous or lymphatic spread of tuberculosis bacilli from other sites or it can be induced by inoculation of skin by bacilli (8). Virulence of organism, amount of inoculum, technical errors and genetic susceptibility may affect on BCG-related LV (4). Lupus vulgaris develops few weeks to 8 years after BCG vaccination and mean duration for BCG-induced LV is one year (6, 9). The largest reported size of LV lesion is 60 × 45 cm (10). The lesion in our patient was 20 × 25 cm in size. Usually Mycobacterium is not found in culture because LV is a paucibacillary form of TB (8). We did not detect the Mycobacterium in acid fast staining and culture (11). Diagnosis is usually confirmed by PCR, Tuberculin Skin Test (TST), histopathological results and response to therapy (8, 12). Although tuberculoid granuloma formation is highly characteristic of cutaneous TB, it is not pathognomonic because histological pattern may be similar to fungal infection, syphilis, leprosy and clinical judgment can help to make the diagnosis (5). When the sample is smear negative, PCR sensitivity will decrease and the result may be negative (13, 14). The physician should consider the rare complication of LV after BCG vaccination, especially in some patients with underlying disease. Our patient was a known case of trisomy 9 with LV; however, we could not find any published report about the relationship between LV and trisomy 9 in PubMed and Google Scholar.