1. Background
Diarrhea is a change in the gastrointestinal tract functioning characterized by an increased frequency of bowel movements and water secretion. Mucosal, structural, and functional lesions of variable extent and severity lead to an imbalance in the functioning of the small and large intestines and in the absorption process of organic substrates and water (1). The consequences of this imbalance include metabolic acidosis, convulsions, unconsciousness, circulatory shock, and prerenal azotemia, with increased risk of death (2).
Although diarrhea is a preventable disease, it is considered a public health problem that generates a reduction in household income and increases health care expenses, not only because of the medications that the sufferers need to take but also because of the occupation of hospital beds and high demand for medical centers (3). Diarrheal disease is the second leading cause of child mortality in the world. Africa and South Asia account for over 80% of the disease (4). In Brazil, according to official data, in the 1995 - 2005 period, there were 39,421 deaths from diarrhea and 1,505,800 hospitalizations associated with this disease in children under 1 year of age (5).
Studies on the frequency of acute diarrhea and population characteristics have reported a consensus view that socioeconomic, demographic, and clinical factors exert a strong influence upon the disease occurrence and severity (4, 6-9). Global epidemiological data confirm this relationship in that they show that the morbidity and mortality rates due to diarrhea are higher in developing countries than in developed economies (4).
Clinical factors such as neonatal prematurity, birth weight, presence or absence of a genetic anomaly, and congenital infections, as well as access to medical care during the prenatal period, define the starting point of newborns in their lives outside the womb and in their adaptation and immune responses to an environment filled with potentially pathogenic agents (10).
The incidence rate of acute diarrheal disease in children is a health indicator, and the estimation of these data can help guide public health policies.
2. Objectives
The aim of this study was to estimate the incidence and risk factors associated with acute diarrheal disease in children aged 0 - 1 year, in a city in southern Brazil.
3. Patients and Methods
This study was approved by the Research Ethics Committee of the University of Southern Santa Catarina (code number 12.035.4.01 III) on April 27, 2012.
This was a prospective cohort study. The sample size determination (11) was based on the following: infants who were not breastfed and had a hazard ratio (HR) of 2.65 for the incidence of diarrhea and exclusive breastfeeding responsible for 80% protection, which resulted in a minimum sample size of 182 children (9). A loss estimate of 15% was included in the minimum sample size calculation, totaling 210 children. The demand for health care services was taken into account for sampling participants, with children enrolled consecutively.
The data were collected between June 2012 and September 2013 from women accompanying newborn babies at Hospital Nossa Senhora da Conceicao. Informed written consent was obtained, and the participants were interviewed to collect data regarding prenatal care, delivery details, and demographic and socioeconomic characteristics of the family. Mothers who agreed to participate were given a health diary to make weekly notes about their children’s clinical data. The health diaries were collected at each medical appointment, and a new one was handed out. Relevant data were also collected from medical records, prenatal care, and child health diaries by the research team. Childcare was provided to all children included in the study, with bimonthly scheduled medical appointments for a 1-year period. During these visits, clinical follow-up data were collected, and confirmation of the data provided by the mothers in the health diaries was made. Six medical appointments were provided to each child over the 1-year period. The children were seen by physicians who were medical school professors with a specialization in pediatrics, at 2 outpatient clinics run by the University of Southern Santa Catarina.
The definition of acute diarrhea by the World Health Organization (WHO), i.e. the passage of 3 or more loose or liquid stools per day, guided this study (11). The occurrence of acute diarrhea as defined by the WHO was considered in this study when reported by the child’s mother or primary caregiver and/or identified by a pediatrician, based on clinical signs and symptoms and diagnostic tests, when available.
The Open Source Epidemiologic Statistics for Public Health (OpenEpi), version 2.3.1, was used to calculate the sample size. The collected data were entered into EpiData program, version 3.1, (EpiData Association, Odense, Denmark), and statistical analysis was performed using the Statistical Product and Service Solutions software (SPSS) for Windows, version 20 (IBM SPSS Statistics, Chicago, IL, USA). Mean, median, standard deviation, standard error, and coefficient of variation were calculated for the continuous variables and proportions for the categorical variables. The outcome incidence was calculated as incidence density rate, expressed as the number of events per person-time. The Cox regression analysis was used to calculate the crude and adjusted relative risk for outcome variables. The significance level was set at 5%.
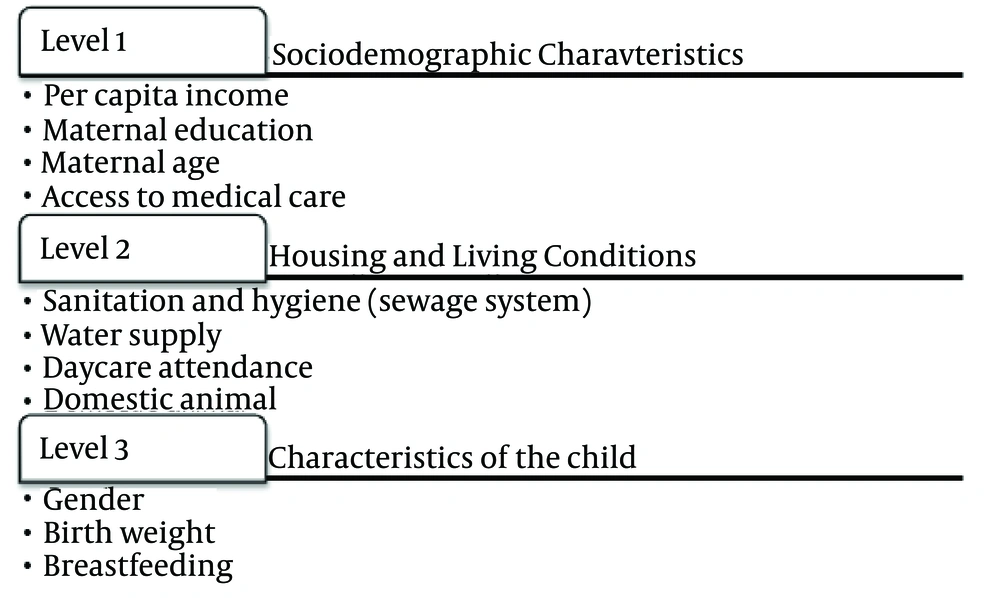
Multivariate analysis to control for confounding factors was performed based on the hierarchical construct model, from studies by Fuchs et al. (12) or those with P < 0.20 in the bivariate analysis, as shown in Figure 1.
The variables in each level that showed P < 0.05 after adjustment were retained in subsequent levels.
4. Results
In total, 210 children were recruited for the study between July 1 and September 30, 2012. There were 23 losses between the first contact and the end of the second month, including the death of 1 baby and 22 mothers who either stopped showing up or answering the phone. Thus, the sample size was reduced to 187 children, who were followed up during their first year of life.
The follow-up period started with 187 children and ended with 168 due to 19 interruptions before completing one year of age. The overall follow-up of children in this study totaled 2,144 months. The data collected during the interview at the first contact with the children’s mothers characterized the sample of 187 participants, who were followed up with regard to sociodemographic characteristics. These data included maternal characteristics, family structure, and socioeconomic and environmental features, which are summarized in Table 1.
| Risk Factors | Diarrheal Diseases | P | HR (95% CI) | |
|---|---|---|---|---|
| Yes | No | |||
| Maternal age, y | 0.024 | |||
| < 20 | 12 (24.0) | 12 (8.8) | 2.11 (1.10 - 4.04) | |
| > 20 | 38 (76.0) | 125 (91.2) | 1.0 | |
| School attendance | 0.206 | |||
| < 11 | 23 (46.0) | 48 (35.0) | 1.43 (0.82 - 2.50) | |
| > 11 | 27 (54.0) | 89 (65.0) | 1.0 | |
| Per capita income (n = 177), US $ | 0.776 | |||
| ≤ 497.60 | 13 (26.0) | 31 (22.6) | 1.10 (0.58 - 2.09) | |
| > 497.60 | 34 (68.0) | 98 (71.5) | 1.0 | |
| Unknown | 3 (6.0) | 8 (5.9) | ||
| Medical care | 0.066 | |||
| Public health (National Public Health System [SUS]) | 41 (82.0) | 91 (66.4) | 1.97 (0.96 - 4.05) | |
| Private health care plan | 9 (18.0) | 46 (33.6) | 1.0 | |
| Water supply | 0.950 | |||
| Artesian well | 8 (16.0) | 23 (16.8) | 0.98 (0.46 - 2.09) | |
| Municipal water supply | 40 (80.0) | 105 (76.6) | 1.0 | |
| Unknown | 2 (4.0) | 9 (6.6) | ||
| Sewage system | 0.672 | |||
| Open trench | 2 (4.0) | 9 (6.6) | 0.74 (0.18 - 3.03) | |
| Municipal sewage system/septic tank | 46 (92.0) | 123 (89.8) | 1.0 | |
| Unknown | 2 (4.0) | 5 (3.6) | ||
| Domestic animals | 0.088 | |||
| Yes | 27 (54.0) | 93 (67.9) | 0.62 (0.35 - 1.07) | |
| No | 23 (46.0) | 44 (32.1) | 1.0 | |
a (n = 187).
b Abbreviations: CI, confidence interval; HR, hazard ratio; P, probability of random error.
c COX regression analysis was used to calculate the crude and adjusted relative risk for outcome variables.
| Characteristics | Diarrheal Diseases | P | HR (95% IC) | |
|---|---|---|---|---|
| Yes | No | |||
| Gender | 0.324 | |||
| Male | 19 (38.0) | 68 (49.6) | 0.75 (0.42 - 1.33) | |
| Female | 31 (62.0) | 69 (50.4) | 1.0 | |
| Birth weight, g | 0.210 | |||
| < 2,500 | 7 (14.0) | 10 (7.3) | 1.67 (0.75 - 3.70) | |
| ≥ 2,500 | 43 (86.6) | 127 (92.7) | 1.0 | |
| Breastfeeding, mon | 0.759 | |||
| < 6 | 22 (44.0) | 67 (48.9) | 0.92 (0.52 - 1.60) | |
| ≥ 6 | 28 (56.0) | 70 (51.1) | 1.0 | |
| Use of pacifiers or bottles | 0.686 | |||
| Yes | 33 (66.0) | 82 (59.9) | 0.89 (0.49 - 1.59) | |
| No | 17 (34.0) | 55 (40.1) | 1.0 | |
| Daycare attendance | 0.689 | |||
| Yes | 9 (18.0) | 19 (13.9) | 0.86 (0.42 - 1.78) | |
| No | 41 (82.0) | 118 (86.1) | 1.0 | |
a (n = 187).
b Abbreviations: CI, confidence interval; HR, hazard ratio; P, probability of random error.
c COX regression; CI = 95%.
In this study, 11 (5.9%) children were never breastfed and 27 (14.4%) were exclusively breastfed for at least 6 months. Only 3 children attended daycare or nursery before the fifth month of life.
Overall, 50 (26.7%) children had at least 1 occurrence of acute diarrhea. Of these, 44 (88.0%) had a single episode, 5 (10.0%) had 2 episodes, and 1 (2.0%) had 3 episodes, totaling 7 cases of recurrence. The data also showed that 36 (72.0%) children had the first event at 6 months of age or older. The incidence density of diarrhea in this study was 26.7 (95% CI, 17.5 - 30.5) per 1,000 children per month.
With regard to the seasonal distribution of the occurrences of diarrhea, 32 (64.0%) cases occurred in the spring or summer. Regarding the distribution of the occurrences of diarrhea by age, only 6 (10.5%) cases occurred in children younger than 4 months, 11 (19.3%) cases between 4 and 5 months of age, and 40 (70.2%) cases were diagnosed in children 6 months of age or older.
The results of the multivariate analysis based on the ranking of the main independent variables are presented in Table 3.
| Independent Variables | HR (95% CI) | P |
|---|---|---|
| First level: Sociodemographic Characteristicsb | ||
| Maternal age, y | 0.029 | |
| < 20 | 2.24 (1.09 - 4.61) | |
| > 20 | 1.0 | |
| School attendance | 0.870 | |
| < 11 | 0.95 (0.49 - 1.82) | |
| > 11 | 1.0 | |
| Per capita income, US $ | 0.616 | |
| < 497.60 | 0.84 (0.43 - 1.66) | |
| > 497.60 | 1.0 | |
| Medical care | 0.045 | |
| Public health (National Public Health System [SUS]) | 2.31 (1.02 - 5.22) | |
| Private health care plan | 1.0 | |
| Second level: Housing and Living Conditions c | ||
| Water supply | 0.499 | |
| Artesian well | 0.74 ( 0.31 - 1.77) | |
| Municipal water supply | 1.0 | |
| Sewage system | 0.602 | |
| Open trench | 0.68 (0.16 - 2.85) | |
| Municipal sewage system/septic tank | 1.0 | |
| Domestic animals | 0.108 | |
| Yes | 0.62 (0.34 - 1.11) | |
| No | 1.0 | |
| Daycare attendance | 0.218 | |
| Yes | 1.62 (0.75 - 3.49) | |
| No | 1.0 | |
| Number of children (continuous variable) | 0.90 (0.60 - 1.35) | 0.608 |
| Third Level: Characteristics of the Child d | ||
| Gender | 0.355 | |
| Male | 0.76 (0.42 - 1.36) | |
| Female | 1.0 | |
| Birth weight, g | 0.213 | |
| < 2,500 | 1.69 (0.74 - 3.84) | |
| > 2,500 | 1.0 | |
| Breastfeeding, mon | 0.859 | |
| < 6 | 0.95 (0.54 - 1.67) | |
| > 6 | 1.0 | |
a Abbreviations; C, confidence interval; HR, hazard ratio; P, probability of random error.
b Adjusted for maternal age, maternal education, per capita income, and type of medical care.
c Adjusted for maternal age, medical care, water supply, sewage systems, domestic animals, daycare attendance, and number of children.
d Adjusted for maternal age, medical care, child gender, birth weight, and breastfeeding.
5. Discussion
In this study, the density incidence of acute diarrhea was 26.7 per 1,000 children per month, according to the measurement of incidence density used, or 298 per 1,000 children, according to the cumulative incidence. Therefore, there was a high incidence rate of the disease in the study population compared with data from the state of Santa Catarina, where the estimated incidence was 93.9 per 1,000 population for children aged under 1 year old, in the 2000 - 2012 period, according to the Department of Epidemiological Surveillance. A cohort study in Northeast Brazil followed up 250 children under 1 year of age for 2 years. In the first year of follow-up, researchers found an incidence rate less significant than that observed in this study (8.4 and 8.7 cases of diarrhea per 1,000 children vaccinated and not vaccinated against rotavirus, respectively) (13).
A systematic review that investigated the incidence of diarrhea in children aged 0 - 59 months in middle and low-income economies included 11 studies conducted in Brazil, which represented approximately 50% of Latin American Studies in the area. This review presented an estimate incidence rate of 4.1 episodes of diarrhea per child aged 0 - 5 months per year for 2010 and 6.2 episodes of diarrhea per child aged 6 - 11 months per year in the Americas for the same year (14). In fact, when compared with the data of the present study, the number of the episodes of diarrhea among children older than 6 months was larger (70.2%) than that among those aged 0 - 5 months (29.8%). A cross-sectional study conducted in Guarulhos, Sao Paulo, showed that infants aged between 4 and 9 months and 10 months or older had a higher risk of diarrhea than other age groups (15).
There has been a slight decline in the incidence of diarrhea in Brazil over the past 20 years (14), as identified by a systematic review (16), which also studied the incidence of infant morbidity and mortality from diarrhea. The systematic review showed an estimated incidence of 3.2 cases per child aged 0 - 5 years per year in developing countries, based on studies published between 1990 and 2000. The authors of that study emphasized that the morbidity rate did not show the same reduction in mortality rates, and they hypothesized that the population growth concentrated in economically disadvantaged regions was a reason for that fact (14, 16).
Based on the literature review, it is possible to understand that many variables are not directly responsible for the occurrence of diarrhea, but they favor the exposure to determinant agents (17). The sociodemographic pattern of the family establishes the child’s housing conditions, influences the mother’s ability to care for the child, and defines the access to health care. Whereas the environment is responsible for the child’s exposure to pathogens, maternal care and access to health care influence the nutritional conditions and severity of diarrhea. Such reasoning permeated the ranking of independent variables in this study, which shows similar suggestions to those made by other authors (12, 18).
In this cohort study, maternal age was considered an independent risk factor for the occurrence of the outcome, given that the children of younger mothers had a higher frequency of acute diarrhea than the children of older mothers. This fact can be attributed to the greater ability of older mothers to identify exposure situations or even to perceive signs and symptoms of diarrhea and anticipate the necessary care compared with younger mothers, either by previous experience or by better education. Vanderlei and Silva supported this hypothesis with a case-control study conducted at the Instituto Materno Infantil of Pernambuco. The authors demonstrated that there was an association between infant hospitalization for diarrhea and maternal knowledge about the management of children with this injury (10). In the same study, no association was found with maternal age, although the results were unexpected for the authors, based on the literature review that they had performed (18).
There was a high prevalence of mothers who reported that they could not afford to pay for private health care and depended on the public health system, the National Public Health System (SUS). It should be noted that, in this study, income was not considered a risk factor for diarrhea; however, the type of health care access was shown to be an independent risk factor for the occurrence of the outcome, which shows that the children who depended on the SUS had a higher incidence of the disease. A study conducted at Hospital Nossa Senhora da Conceicao, located in the same city where this cohort study was conducted, supports the findings presented here, showing that 73.7% of the hospitalizations for the diarrhea of a presumed infectious origin in children up to 5 years of age were paid by the SUS (19). Another study conducted in Pelotas, Rio Grande do Sul, compared 3 cohorts from 3 consecutive decades and demonstrated that children from poorer families had higher rates of hospitalization for diarrhea than their counterparts (20). Indeed, low-income families have low access to health care plans, whereas high-income families can pay for their private health care plans. Therefore, to a certain extent, access to quality health care services depends on per capita income (17).
In the present study, few children were exclusively breastfed for at least 6 months, as recommended by the Brazilian Ministry of Health and by the WHO, which interferes with the assessment of their immune protection (21). Exclusive breastfeeding for fewer than 6 months resulted in doubling the chance of diarrhea incidence (8). A recent study evaluated the influence of breastfeeding on 4,164 infants and showed that exclusive breastfeeding for at least 4 months and partial breastfeeding after this period resulted in low risk for gastrointestinal tract infections, with an odds ratio of 0.41. The same study stated that partial breastfeeding did not provide significant protection, even if it lasted for at least 6 months (22). However, in the current study, breastfeeding was not a statistically significant protection against the occurrence of diarrhea.
There were limitations to this study regarding the development of the proposed methodology. Keeping in touch with the mothers was a major challenge, especially with those who opted to see pediatricians not affiliated with this cohort. Another limitation was the lack of laboratory tests to identify the etiologic agent of acute diarrhea in order to control the transmission mode, and consequently, the risk factors related to the outcome. In addition, the sample showed a homogeneous sociodemographic profile, considering that there was another maternity hospital for patients who had private health insurance. Some mothers with high-income levels refused to participate in the study, which may have influenced the results of our data analysis. Despite these limitations, the study design helped identify causative factors and allowed the estimation of the incidence density of diarrhea. Given that the estimation of incidence density includes the follow-up period in its calculation, it enjoys high accuracy when compared with cumulative incidence, which is one of the advantages of a cohort study.
Based on the results, this study concluded that the incidence of acute diarrhea in children aged 0 - 1 years was 26.7 cases per 1,000 children per month, and the independent risk factors for the occurrence of diarrhea were maternal age under 20 years and health care services provided by the SUS.