1. Introduction
Osteomyelitis (OM) is a rare but serious inflammation of the bone resulting from an infection caused by an organism (1). In children, OM can be either acute or chronic. Chronic OM is an unusual inflammatory process involving multiple osseous sites. OM often affects the pelvis and vertebrae of the spine. It can also occur in the feet. There are three ways that organisms can infect the bone: via the blood stream, by transfer from the immediate vicinity of a wound through penetrating trauma, and from iatrogenic causes (2). The most common pathogens causing OM depend on the patient's age. Staphylococcus is the most common cause of acute or chronic hematogenous OM in children (3). In this paper, we present the case of a girl with chronic cranial OM resulting from a skin graft following an acid attack.
2. Case Presentation
A 3-year-old girl was referred to the infectious diseases clinic of Mofid children’s hospital of Tehran with a past medical history of acid exposure from an acid-throwing attack 3 years prior. Her cranium, right eye, hands and feet were damaged during this attack. Prior to her presenting at our clinic, she had been admitted for the restoration of her scalp hair. Ten days after receiving a scalp expansion graft, she developed a fever and discharge from the commissure of the skull. Due to her severe illness upon admission, a treatment of intravenous vancomycin and meropenem was begun after obtaining the appropriate laboratory work-up and blood cultures. Imaging modalities were also performed.
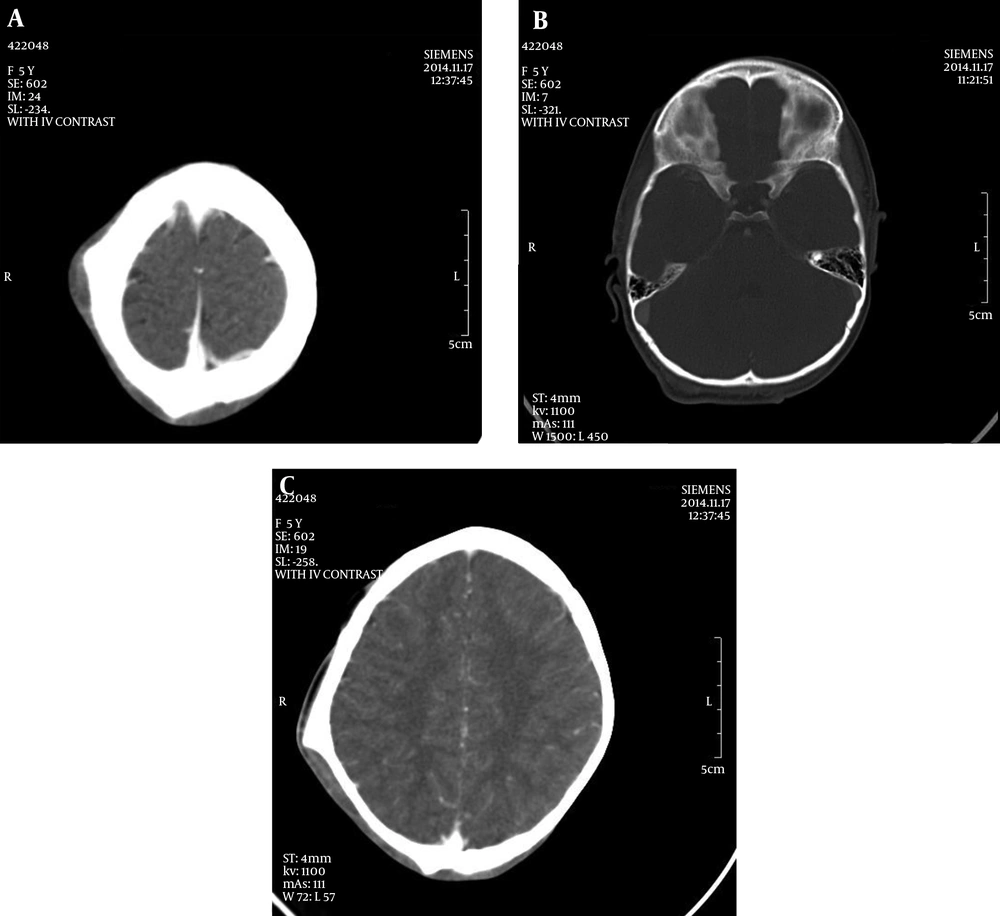
In laboratory data, she was found to have a high erythrocyte sedimentation rate (ESR) and C- reactive protein (CRP), and neutrophilic dominant leukocytosis. Her blood culture was positive for E. coli. A brain spiral computed tomography (CT) scan without contrast was done. A brain spiral CT scan without contrast and brain magnetic resonance (MR) imaging showed chronic OM of the cranium. A solid periosteal reaction was seen at both ends of the elevated periosteum in the right parietal and occipital bones. Soft tissue density areas were seen adjacent to the right parietal bone. Erosion was seen in the outer table of the right parietal bone. These findings are strong indications of chronic OM. Findings in the MR images of the cranial bones were consistent with this diagnosis.
In our hospital, the patient was treated with intravenous vancomycin and meropenem for 25 days. She was then discharged with two oral antibiotics, cefixim and clindamycin, to continue taking at home.
3. Discussion
Chronic OM of the skull base is a rare entity. There are few other conditions than can involve the bones of the skull. It is therefore reasonable to use imaging modalities such as MR imaging or CT scans to rule out other conditions, especially malignancy. The morbidity and mortality of skull-base OM is very high. Central skull base OM mainly involves the sphenoid or occipital bones without coexisting eternal otitis. CT findings in this case included clival and cortical bone erosion and adjacent soft tissue swelling. MR findings showed texture changes and enhancement of the involved bones and soft tissues. (See Figure 1), Biopsy specimens revealed chronic inflammation.
In one case reported by Jeong et al. (2) in Seoul, a patient presented with an occipital headache and a unilateral posterior neck mass. In MR imaging, OM was seen in in the left petrous apex and both clivus and skull bones. Yousef et al. at the American university of Beirut medical center reported another case in which an immunocompetent patient with invasive aspergillus mastoiditis due to OM was treated successfully (3). Both of these patients had negative cultures of their external auditory canals. After six weeks all patients showed resolution of the temporal bone abnormality seen on gallium scans. And in a follow-up six months later, none of the patients had a recurrence of the infection. Connolly et al. (4) reported a 10-year-old immunocompetent girl with headache and chronic sinusitis who developed lateral medullary syndrome following streptococcal milleri esphenoidal OM. In another case report, unilateral skull bone OM with facial paralysis and lower cranial nerve palsies occurred following bilateral otalgia.
We know that, while rare, chronic skull base OM is one of the most severe infections that can happen in childhood. Iatrogenic causes of this condition, such as acid-throwing attacks, are unusual. Most cases of OM of the skull base occur as a complication of localized malignant otitis external and sinusitis. But our patient developed chronic OM as a complication of a skin graft and tissue damage. In the literature, positive cultures are extremely rare, but in this case we had a positive culture of the blood. Patients with chronic OM rarely appear ill, but our patient was febrile and did appear ill. With special attention to spiral head CTs, the penetration of the infection into the brain’s parenchyma and other areas of the skull was identifiable. This is a very important point in outstanding our report (5-8).
3.1. Conclusion
Chronic cranial OM should be considered in the differential diagnosis for patients experiencing complicated traumatic head injuries and treatments.