1. Background
Sepsis in children remains a significant cause of morbidity and mortality worldwide. Sepsis can be defined as the body’s response to an infection. It is a potentially fatal, whole-body inflammation (a systemic inflammatory response syndrome or SIRS) (1). Severe sepsis is complicated by organ dysfunction. Bacteria are the main cause of sepsis; however, even fungi, viruses, and parasites in the blood, urinary tract, lungs, skin, and other tissues can cause sepsis. The frequency of pediatric sepsis was found to be greater than 42,000 cases annually, with an associated mortality rate of 10% in the United States (2). Studies from the United Kingdom have shown that 17% of children die from severe sepsis and septic shock in pediatric intensive care units (PICUs) (3). The incidence of neonatal sepsis, according to data from the national neonatal perinatal database (NNPD) for 2002 - 03, was 30 per 1,000 live births (2). The sepsis mortality rate of children in PICUs in developing countries is higher than 50% (4). Sepsis occurs progressively in various stages, which include systemic inflammatory response syndrome (SIRS), sepsis, severe sepsis, septic shock, and multiple organ dysfunction syndrome (MODS). The etiology of sepsis is associated with infections such as meningitis, pneumonia, arthritis, osteomyelitis, phlebitis, gastroenteritis, and urinary tract infections. It is also due to immune suppression, major injuries, catheter insertion, or as a nosocomial infection (3). Although everyone could potentially develop sepsis from minor infections, it is most likely to develop in children with very low birth weight, suppressed immune systems, congenital anomalies, catheterization, and co-morbid conditions. The most common sources of infection resulting in sepsis are the lungs, abdomen, and the urinary tract. Common symptoms of sepsis include those related to a specific infection, when accompanied by high fevers, hot flushed skin, elevated heart rate, hyperventilation, altered mental status, swelling, and low blood pressure. In the very young and elderly, or in people with weakened immune systems, the pattern of symptoms may be atypical with hypothermia and without an easily localizable infection. Even after providing a rational therapy, the mortality rate may remain high due to complications caused by sepsis, such as severe sepsis and septic shock, end organ damage, such as respiratory, renal, cardiac, etc., and multiple organ dysfunction syndrome (MODS) or failure (5).
2. Objectives
The present study was conducted with the objective of measuring the incidence of etiological factors and clinical characteristics of sepsis in neonate and pediatric patients.
3. Patients and Methods
This is a descriptive cross-sectional study, with 52 patients enrolled. Of those, there were 30 admissions to the neonatal intensive care unit (NICU) a 60-bed specialized unit and 22 admissions to the pediatric intensive care unit (PICU) of a 1,000-bed tertiary care teaching hospital during the period of October 2014 - March 2015. Among the 52 patients, 29 were diagnosed as having sepsis through cultures, and 23 were diagnosed on the basis of signs and symptoms of sepsis (clinical sepsis). Both patient types were included in the study. Data were collected on age, sex, history, clinical manifestations, laboratory investigations, and culture tests. Air contamination was assessed using the settle plate method in different wards of the hospital (PICU, NICU, maternity ward, labor rooms, and pediatric ward). Patients with sepsis were diagnosed according to the SIRS (systemic inflammatory response syndrome) criteria, which includes changes in temperature, WBC count, respiratory rate, and heart rate. Patients with a severe condition, such as septic shock, were diagnosed on the basis of the SIRS criteria and the presence of two or more organ dysfunctions.
4. Results
A total of 901 patients were admitted for the duration of six months (October 2014 - March 2015), out of which 736 were NICU admissions and 165 were PICU admissions. Of all the patients admitted to the PICU and NICU, the incidence rate was found to be 5.7%, which included both culture proven sepsis and sepsis diagnosed on the basis of signs and symptoms, i.e., clinical sepsis. The median age of the patients was less than three months. Children aged 0 - 3 months accounted for 57.6% of admissions, followed by 3 - 6 months (5.76%), 6 months - 1 year (5.76%), 1 year - 3 years (11.53%), 3 years - 5 years (3.84%), 5 years - 10 years (9.61%), and more than 10 years (5.76%). The male to female ratio was 1.7:1. Common etiologies were pneumonia, meningitis, and urinary tract infection (UTI) associated with congenital anomalies. Catheterization (done by the physicians for medical purposes) and very low birth weight were risk factors in neonates (Table 1); in pediatrics, common etiologies were pneumonia, meningitis, and urinary tract infection (UTI) associated with catheterization as a risk factor (Table 2).
| Age | Gender | Risk Factors, % | Etiology, % | Likely Pathogen, % | |
|---|---|---|---|---|---|
| Male | Female | ||||
| Birth - 3 mo | 23 | 7 | Congenital anomalies (16.6), Intra-partum (20), Catheterization (16.6), Surgery (13.3) | UTI (23.3), Meningitis (20), Pneumonia (20) | E. coli (10), Klebsiella (23.3), Enterococcus (16.6%), MRSA (3.3) |
. Common Risk Factors, Etiologies, and Likely Pathogens Prevalent in Neonates
| Age | Gender | Risk Factors, % | Etiology, % | Likely Pathogen, % | |
|---|---|---|---|---|---|
| M | F | ||||
| 3 - 6 mo | 2 | 1 | Surgery (4.5), Other illness (9) | UTI (9), Meningitis (4.5) | E. coli (4.5), Klebsiella (4.5), H. influenzae (4.5) |
| 6, mo - 1 y | 2 | 1 | Catheterization (9) | Pneumonia (9) | Klebsiella (4.5) |
| 1 - 3, y | 3 | 3 | Catheterization (9), Others (9) | Pneumonia (13.6) | Gram-negative sp. (9) |
| 3 - 5, y | 2 | 0 | Catheterization (9) | Pneumonia (4.5) | Klebsiella (4.5) |
| 5 - 10, y | 2 | 3 | Catheterization (9) | Age (4.5), Others (4.5) | Gram-negative sp. (4.5), S. aureus (9) |
| > 10, y | 1 | 2 | HIV (4.5), Others (4.5) | Meningitis (4.5), UTI (4.5) | Others (13.6) |
Common Risk Factors, Etiologies, and Likely Pathogens Prevalent in Pediatrics
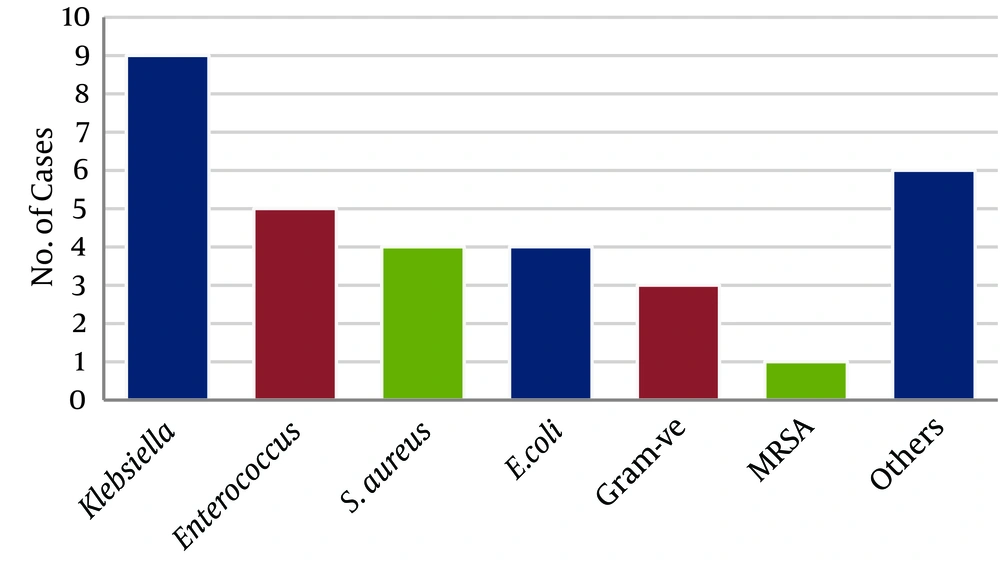
The mean length of stay was four days for patients with severe sepsis and septic shock; the mean length of stay for patients with sepsis was 20 days. Almost 1/2 of the children (29/52) had a culture proven infection. Organisms were isolated from three basic body fluids: blood (46.4%), urine (28.5%), and CSF (25%). The microbiology of septic children admitted to the PICU is shown in Figure 1.
The most commonly seen organisms were Klebsiella (28.1%), Enterococcus (15.6%), S. aureus (12.5%), E. coli (12.5%), gram-negative species (9.4%), MRSA (Methicillin-resistant Staphylococcus aureus) (3.1%), and others (18.8%) (Candida, Streptococcus, H. influenzae, Pseudomonas, etc.), as shown in Figure 2.
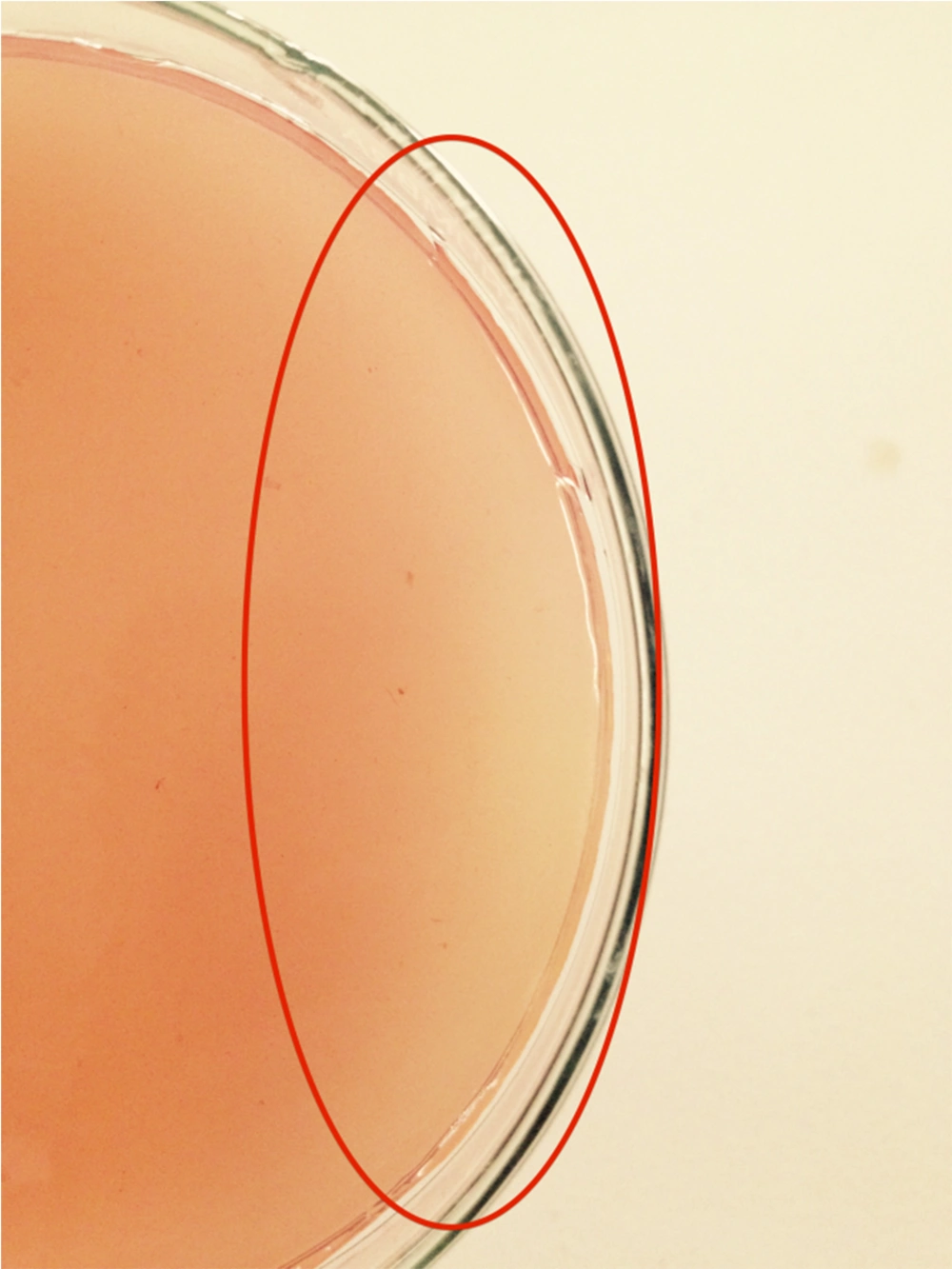
Microbiological testing was conducted to assess the causative relationship between air contamination in different wards of the hospital and the risk of developing sepsis in pediatric and neonate patients. The settle plate method was used, and the samples were collected from the maternity ward, labor rooms, pediatric ward, PICU, and NICU. After incubation, it was found that the highest colony count was present in the labor rooms, and the most commonly isolated bacteria were the gram-negative (Figure 3).
Neonatal sepsis is classified into early onset and late onset sepsis. Out of 30 sepsis related NICU admissions, 6.6% (two cases) of patients showed early onset sepsis (present before 72 hours of life), and 16.6% (five cases) showed late onset sepsis (present after 72 hours of age) (Figure 4).
Evaluations of clinical characteristics of sepsis were classified into SIRS with sepsis (39%), SIRS with severe sepsis (51%), and SIRS with severe sepsis with cold/warm shock (10%) (Table 3). Multi-organ dysfunction was seen in 61% of the patients (Table 4). The organ dysfunction in sepsis patients is shown in Table 5.
| Age | Gender | MOD, % | |
|---|---|---|---|
| Male | Female | ||
| Birth - 3, mo | 23 | 7 | Hematology (30), Renal (13.3), Respiratory (16.6), Metabolic Acidosis (6.6) |
Classification of Multiple Organ Dysfunctions in Neonates
| Age | Gender | MOD, % | |
|---|---|---|---|
| M | F | ||
| 3 - 6, mo | 2 | 1 | Hematology (9), Renal (4.5) |
| 6, mo - 1, y | 2 | 1 | Hematology (9), Purpura Fulminans (4.5) |
| 1 - 3, y | 3 | 3 | Hematology (18.1), Respiratory (9), CNS (4.5), Purpuric Rash (9) |
| 3 - 5, y | 2 | 0 | Hematology (9) |
| 5 - 10, y | 2 | 3 | Hypoglycemia (4.5), Purpura Fulminans (9), Hematology (9) |
| > 10, y | 1 | 2 | Renal (9), Hematology (13.6), CNS (4.5) |
Classification of Multiple Organ Dysfunctions in Pediatrics
| MOD | Percentage |
|---|---|
| Hematologic | 50 |
| CVS | 38.46 |
| Respiratory | 20.3 |
| Purpura Fulminans | 12.9 |
| Renal | 16.6 |
| Neurologic | 7.4 |
| Hepatic | 3.7 |
Frequency of Organ Dysfunctions
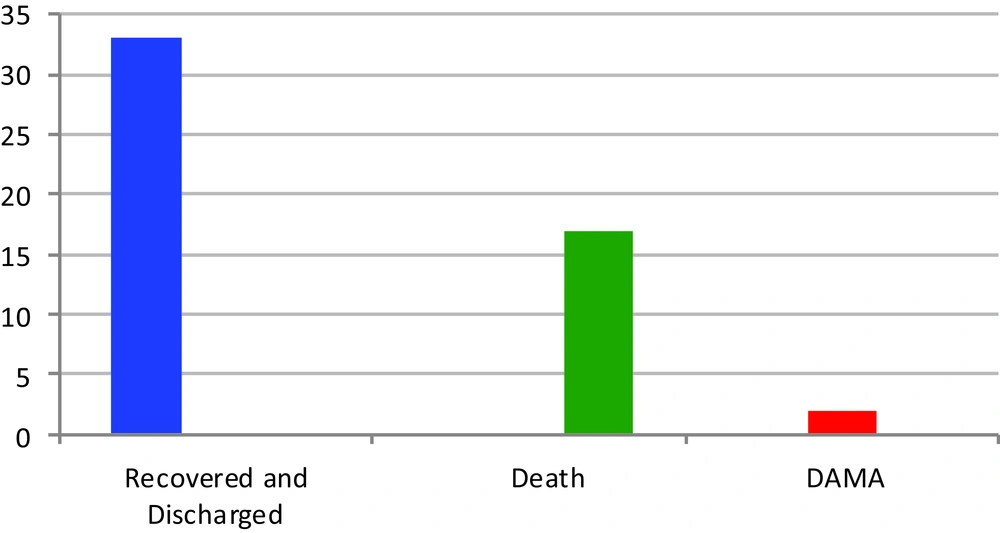
The mortality rate of sepsis was 32.7%. In patients with SIRS, severe sepsis, and MOD, the mortality rate was 5.7%; in septic shock cases, it was 26.9%. With an improved prognosis of 67.30%, the pediatric population recovered, and they were discharged. There was a significant relationship between severity of sepsis and mortality (P < 0.001). Hence, mortality depends on the severity of the sepsis.
5. Discussion
Sepsis can be defined as the body’s response to an infection. It is a potentially fatal, whole-body inflammation (systemic inflammatory response syndrome or SIRS), and it is assumed to be the result of the host’s invasion by pathogenic organisms, which then spread to and throughout the bloodstream (6). Notably, septicemia is a systemic infection, or infection of the blood, often described as “blood poisoning.”
Out of 901 admissions to the PICU and NICU, the sepsis incidence rate was 5.7%, with a predominance of males versus females (1.7:1). According to studies in developed countries, the overall incidence was higher in neonates and fell dramatically in older children or pediatrics. Additionally, the incidence of sepsis was higher (15%) in males than in females. This difference might be due to the difference in the hospital settings used for the studies. These could include how well the NICUs and PICUs were sanitized and the methods used for handling patients, e.g., insertion of catheters, feeding procedures, etc.
The mean length of stay of patients with severe sepsis and septic shock was four days, and the mean length of stay for patients with sepsis was 20 days (7). This was because patients with severe sepsis and septic shock had a greater rate of fatalities. Out of 17 cases of death, five (29.4%) were neonates and 12 (70.5%) were pediatric patients. These patients were primarily referred from local clinics and secondary hospitals.
The common sources of infection for sepsis in the study were pneumonia, meningitis, and respiratory tract infections in pediatrics as well as neonates. Inwald conducted studies in tertiary care hospitals in the United States, finding that pneumonia is the most common type of community and hospital acquired infection in pediatrics. It has a significantly high rate compared to other sources of infection, such as meningitis, urinary tract infection, etc., because almost all pediatric admissions undergo ventilation and catheterization (like tracheostomy), which creates an access point for microorganisms to infect the lungs (8).
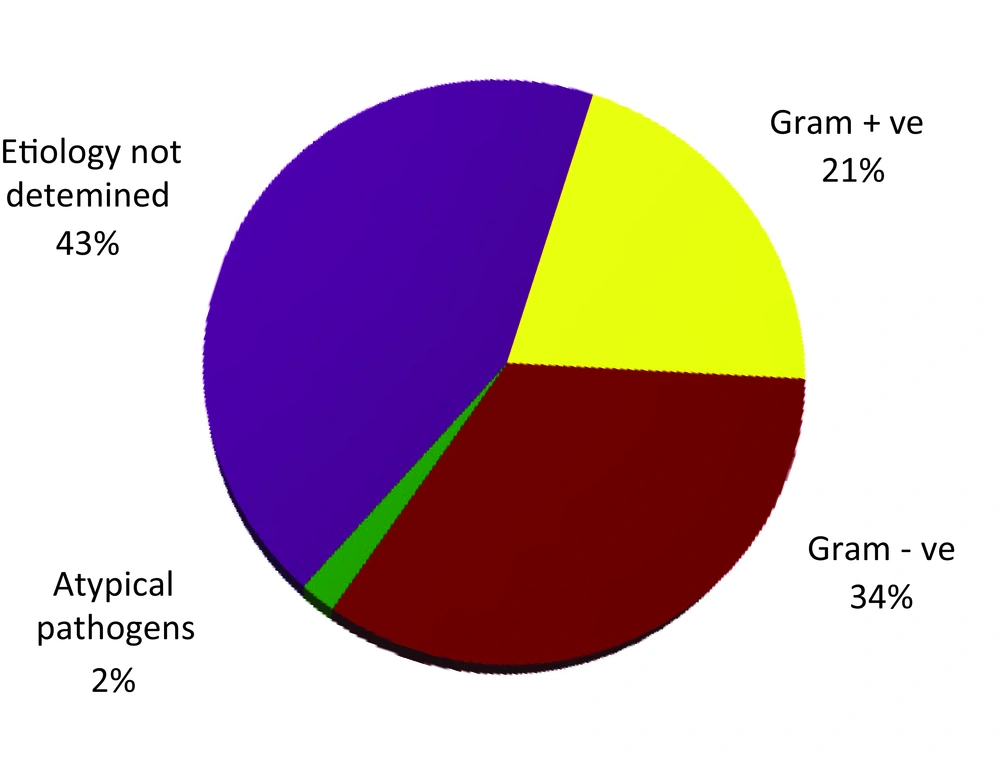
Pathogens were isolated from various specimens, namely blood, urine, and cerebrospinal fluid (CSF). The most commonly isolated pathogens were S. aureus, Klebsiellapneumoniae, E. coli, enterococcus, MRSA (Methicillin-resistant Staphylococcus aureus), candida, and Acinetobacter. Among these, Klebsiella pneumoniae, E. coli, and S. aureus were more isolated in number.
Gram-negative bacteria (i.e., E. coli, K. pneumoniae) are the most potent organisms causing sepsis; this is because sepsis is considered to be a response to an endotoxin a molecule that was thought to be relatively specific to gram-negative bacteria. In fact, some original studies of sepsis state that gram-negative bacteria are the most common cause of sepsis (9).
Sepsis is classified into two main types in neonates: early onset sepsis (EOS) and late onset sepsis (LOS). Anwer et al. (10) conducted a study to compare the characteristics of the two, finding the incidence of late onset sepsis (16.6%) higher than that of early onset sepsis (6.3%). Early onset sepsis presents within the first 72 hours of life. Infants with EOS usually present with respiratory distress and pneumonia. In our study, neonates were seen with respiratory distress. Late onset sepsis usually presents after 72 hours of age. The main sources of infection in LOS cases are nosocomial or community acquired paths. Neonates usually present with septicemia, pneumonia, and meningitis. In this study, neonates diagnosed with LOS presented with respiratory distress and infection of the umbilical cord (omphalitis) (10). The major risk factors for LOS are low birth weight, prematurity, admission to the ICU, mechanical ventilation (i.e., oxygen or nebulization), and invasive procedures. The most common risk factors for developing sepsis in this study were catheterization, congenital anomalies, and low birth weight. This clarifies why late onset sepsis is seen in greater numbers than early onset sepsis.
Microbiological testing was conducted to assess air contamination in different wards to obtain a causative relationship between air contamination and the risk of developing sepsis. Air is the greatest disseminator of pathogenic microbes, which cause significant problems in the indoor hospital environment, particularly in terms of nosocomial infections. Insufficient ventilation, high dusting, overcrowding, aerosols spread through sneezing and coughing, high movement of personnel, and improper management of hospital monitoring are the main sources of indoor air contamination. This study followed the proper sampling method by using disposable plastic Petri dishes containing McConkey’s agar, which is specifically used for isolation of gram-negative bacteria. The samples were collected from the maternity ward, pediatric ward, and labor rooms of the hospital. The petri plates were exposed for approximately one hour and were immediately brought to the laboratory for incubation at 37°C for 24 hours. After incubation, the total colony forming units were counted. The results showed the highest colony count in the labor rooms and maternity ward. There are many reasons why labor rooms are more contaminated than other wards, such as building design, improper ventilation, high movement of individuals (i.e., per labor, there will be at least 3 - 5 medical staff and the patient), wearing unprotected footwear, and improper sanitization. During each labor, a large amount of blood as well as amniotic fluid and other body fluids are spilled in the room, which play a significant role in promoting the growth of microorganisms irrespective of whether or not the mother had any infection during the labor. It was observed that staff did not use or promote the use of any protective footwear for those entering the labor room, unlike what was seen in the PICU and NICUs of this hospital.
Most of the patients presented with multiple organ dysfunction syndrome (MODS), with an association of two or more organ dysfunctions. The most common were hematological (50%), cardiovascular (38.46%), and respiratory (20.3%). Balk (11) conducted a study, finding that, out of 248 cases of sepsis, 56 presented with MOD with an association of four or more organ dysfunctions (35%). The most common organ dysfunction was cardiovascular, which occurred in 17% of the children with sepsis. Correlating with the major risk factors seen in this study, as mentioned before, catheterization is a major risk factor for developing sepsis. Catheters are directly introduced into the bloodstream, creating easy passage for microorganisms to invade the blood.
A blood culture is the gold standard for diagnosing septicemia; it should be performed in all cases prior to starting antibiotics. In this study, blood cultures, complete blood counts, CSF testing, and radiology were done to confirm a diagnosis of sepsis. Specific markers of sepsis, such as procalcitonin (PCT), were also used in this study in cases of negative blood cultures. Procalcitonin (PCT) is a peptide precursor of the hormone calcitonin, the latter being involved with calcium homeostasis. In healthy people, plasma PCT concentrations are typically below 0.05 ng/mL, but PCT concentrations can increase up to 1,000 ng/mL in patients with sepsis, severe sepsis, or septic shock. PCT concentrations exceeding 0.5 ng/mL are generally considered abnormal, and values in the range of 0.5 - 2 ng/mL suggest that the patient is at risk for sepsis; they generally represent a gray zone in terms of the assessment of sepsis and related conditions (12).
Despite extensive medical advances over the past two decades, the number of reported cases of sepsis continues to increase at an alarming annual rate due to limited progress in treatment and diagnostic methods.
Clinical outcomes were assessed based on two parameters: recovery and death. Recovery was considered depending on the patient’s condition at the time of discharge. Patients who showed improvement in their condition and were hemodynamically stable were discharged. All vital signs within normal limits and improvement in one of the organ dysfunctions were considered as a recovering state for sepsis patients (33 cases; 63.46%). Another clinical outcome assessed was death (17 cases; 32.69%). The most common cause of death found in our study was septic shock with organ dysfunction. In this study, two cases underwent discharge against medical advice (DAMA). According to various studies in the United States (10%), United Kingdom (17%), and in other developing countries (> 50%), mortality in sepsis was largely due shock and/or MOD.
After the assessment of clinical outcomes, the severity of sepsis was compared with the death cases, and it was found in each grade of sepsis SIRS with sepsis, SIRS with severe sepsis with MOD, and SIRS with sepsis with cold/warm shock. After applying statistics, it was found that there was a significant relationship between mortality and severity of sepsis (P < 0.001), i.e., the more severe the case, the greater the risk of mortality (13). This could be due to the lifestyles of people in developing countries, inefficient facilities, education, and hygiene in hospitals.
5.1. Conclusions
The incidences of LOS are greater than EOS, with catheterization as LOS’s major risk factor. This is why hemodynamic dysfunction is the most predominant organ dysfunction; it gives direct access to microorganisms to invade the blood, subsequently causing hemodynamic dysfunction. Gram-negative bacteria play an important role in catheter-induced sepsis. Microbiological air contamination testing for gram-negative bacteria confirmed that the labor room is the most contaminated ward. This is a major risk factor for neonatal sepsis. A significant relationship between severity and mortality was established, i.e., the more severe the condition of sepsis, the greater the chances of mortality (P < 0.001).