1. Introduction
Kawasaki disease (KD) is an acute febrile vasculitis of early childhood of unknown origin that can result in coronary artery abnormalities, including aneurysms. Diagnosis of KD is made in the presence of a prolonged fever (at least 5 days) associated with 4 of these 5 criteria: bilateral and non-exudative conjunctivitis, mucosal changes, changes in extremities, rashes, and cervical lymphadenopathy (LAP) (1).
Some patients do not fulfill the diagnostic criteria for KD and are known as atypical or incomplete KD. Echocardiographic changes consistent with KD, elevated erythrocyte sedimentation rate (ESR) or C - reactive protein (CRP) with at least 3 supplemental laboratory criteria should be presented in these patients (2).
The patients should be treated with intravenous immunoglobulin (IVIG) and high-dose aspirin in the first 10 days of illness to minimize cardiac complications.
Although KD may present with only a fever and lymphadenopathy (node-first KD) and may be confused with suppurative cervical lymphadenitis, we report a case with presentation of fever, unilateral conjunctivitis, LAP, and finger desquamation, diagnosed as oculoglandular syndrome, which to our knowledge has not been reported to date (1).
2. Case Presentation
The patient was a 12-year-old boy with fever, unilateral right periorbital edema, and conjunctivitis, followed by ipsilateral preauricular lymphadenopathy during the last few days. He had also developed skin rashes, which were treated as scarlet fever before referral to our hospital. The patient came to our clinic with relapse of sustained fever from 5 days earlier and finger scaling. In his physical examination, he was febrile (rectal temperature: 40° centigrade) and had a bite-like lesion on his right eyelid and finger desquamation. We did not find anything else on his first visit. He was admitted for further evaluations. Urine and blood cultures were negative, and throat culture revealed normal bacteria flora. Results of other laboratory tests are shown in Table 1.
| Laboratory Tests | Result | Unit | Normal Range for Males |
|---|---|---|---|
| White blood cell (WBC) | 9600 | cells/microliter | 4000 - 10000 |
| Hemoglobin (Hb) | 11.2 | gram/deciliter | 14 - 18 |
| Mean corpuscular volume (MCV) | 80.1 | Femoliter (fL) | 79-96 |
| Platelets (Plt) | 243000 | cells/micro liter | 150000 - 450000 |
| Blood urea nitrogen (BUN) | 8 | milligram/deciliter | 7 - 23 |
| Creatinine (Cr) | 0.7 | mg/dl | < 16y: 0.2 - 1 |
| Aspartate aminotransferase | 22 | unit/L | 5 - 40 |
| Alanine Aminotransferase | 18 | unit/L | 0 - 41 |
| Albumin (Alb) | 3.2 | g/dl | 3.5 - 5.5 |
| Amylase | 29 | unit/L | 0 - 100 |
| Erythrocyte sedimentation rate | 125 | millimeter/hour | 0 - 20 |
| C-reactive protein | 1 | Qualitative | Negative |
| ASO titer | 125 | IU/mL | < 200 |
In the second day of hospitalization, because of the patient’s prolonged fever (> 5 days), skin rashes, finger peeling, and elevated ESR, our first differential diagnosis was atypical Kawasaki disease (KD), so we performed echocardiography, which was completely normal. Therefore, our attention directed toward mismanaged oculoglandular syndrome (conjunctivitis and ipsilateral LAP). Serum samples were taken to rule out cat scratch disease, tularemia, and herpes simplex virus infection, and then gentamycin was started. After antibiotic therapy, fever subsided. Serologic tests were all negative. Anti-Nuclear Antibody (ANA), cytoplamsic Anti-neutrophil cytoplasmic antibodies (ANCA-C), perinuclear Anti-neutrophil cytoplasmic antibodies (ANCA-P), and complement component 3 and 4 (C3 and C4) were also requested. All of them were within normal limits.
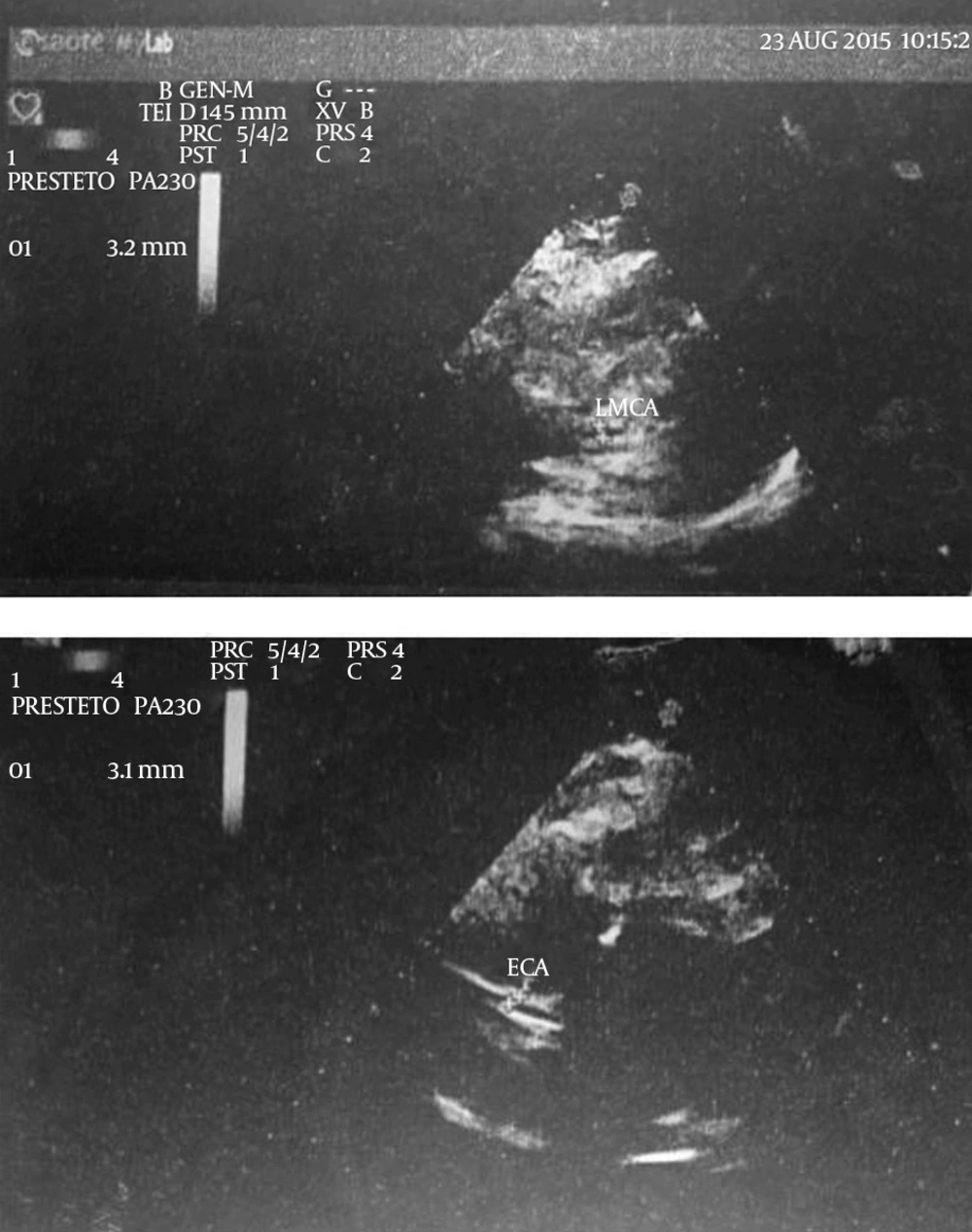
Four days after admission, he presented with bilateral conjunctivitis. Echocardiography was performed again. Surprisingly, pleural and pericardial effusions with dilated left anterior descending coronary arteries were found: left main coronary artery (LCA) 3.8 mm; left anterior descending artery (LAD) 3.8 mm; and right coronary artery (RCA) 3.2 mm (Figure 1). Consequently, diagnosis of atypical KD was confirmed. He went on IVIG and high-dose aspirin and was discharged from hospital after two days. After two weeks, he underwent a third echocardiograph. Pleural and pericardial effusion had disappeared, but coronary artery dilation was still present. However, after a week, platelets had significantly increased (Plt: 690000) ; after 8 weeks, platelet count and ESR had returned to normal range, and echocardiography revealed no pericardial effusion or coronary artery abnormality (LCA 3.8 mm; LAD 3.1 mm; and RCA 3.2 mm). Close follow-up for coronary dilation by a pediatric cardiologist was strongly recommended.
3. Discussion
Kawasaki disease (KD) is a self-limited febrile illness of childhood. Cardiac involvement is the most important manifestation of the disease, and the diagnosis is made by echocardiographic studies (3). Coronary artery abnormalities, including aneurysms, occur in almost 25% of untreated patients in the second to third week of the disease and are more common in incomplete KD, which, in the presence of appropriate treatment, decreases to 2 - 4% (1, 4-6). The etiology of KD is not established yet, but based on various evidence; infectious origin has been proposed more than other theories (7).
Onset of KD concurrent or following with a recent infection is reported by several authors. Pavone et al. (8) reported two cases of otorrhea in febrile and Epstein bar virus (EBV) positive children with no response to appropriate treatment; they fulfilled KD criteria in the following days). In 2011, Husain and Al-Rashid (9) reported a two-month-old girl with Escherichia coli (E. coli) urinary tract infection who did not respond to antibiotic therapy; she developed clinical manifestations of KD later. In 2010, Vitale et al. (10) reported four cases of typical KD in children with serological evidence of Mycoplasma pneumonia infection. Rigante et al. (11) reported two cases of KD in Italy with concurrent Coxsackie virus B3 infection. There are two reported cases of KD-associated orbital cellulitis, although they were non-bacterial and only responded to IVIG (12, 13). Because of continuing fever despite antibiotic therapy prior to admission to hospital (Penicillin with the possibility of scarlet fever), and given that conjunctivitis is not a sign of scarlet fever, Kawasaki diagnosis for our patient is reasonable.
The patient was a case of KD, with initial presentation of unilateral conjunctivitis and oculoglandular syndrome but who fulfilled diagnostic criteria over time. It should be mentioned that the ceasing of fever in our patient was a result of the self-limited nature of the disease, which can occur after 5 days, and was not related to gentamycin initiation. In fact, five days’ duration of fever is sufficient to be included as a KD criterion and, after that; fever can either subside or continue.
KD is a self-limited disease and the goal of IVIG initiation is to reduce the risk of consequent cardiac involvement, which has a 10-day golden time; if it is delayed, patients are at 20% - 25% risk of coronary artery aneurysms. As a result, the concurrence of different infections with KD is an important issue and can result in delayed diagnosis and missing the limited golden time of the disease. Physicians should therefore be aware of it and pay attention to all signs and symptoms of patients and reevaluate non-responding individuals.