1. Background
One million cases of tuberculosis (TB) are estimated in children worldwide; of whom 75% occur in 22 high-burden countries. Tuberculosis is among the 10 main causes of mortality in children with a universal estimation of 130,000 deaths per year (1). Cavitary pulmonary TB, adult type TB, is rare in children (2). However, cavities are related to a high mycobacterium load which act as a source of infection in these children and are often nonresponsive to therapy (2, 3). The proportion of adults with pulmonary TB who have a cavitary disease at the time of diagnosis has been recognized in the studies (4-6). However, the data available on cavitary pulmonary TB in children is sparse and inconclusive. Furthermore, TB varies between children and adults in different aspects such as pathophysiological and immunological responses that can affect the diagnosis, prevention, and treatment in children (7).
2. Objectives
The aim of this study was to evaluate the clinical and radiological findings of cavitary pulmonary TB in children.
3. Patients and Methods
This study was conducted on 97 children less than 15 years old with pulmonary TB who were admitted to TB wards of national research institute of tuberculosis and lung disease (NRITLD) in Masih Daneshvari medical center between March 2007 and March 2013 to identify cavitary pulmonary TB. Investigations for diagnosis of TB included history and physical examination, complete blood count, tuberculin skin test (TST), smear of sputum for acid fact bacilli (AFB), culture for Mycobacterium tuberculosis (MTB), and chest imaging (X-ray or computerized tomography (CT )). Cavitary pulmonary TB was defined by a medical history, clinical and laboratory findings compatible with TB, and a chest imaging showing cavitary lung lesion. Institutional review board approval was not required for this retrospective study.
4. Results
Seven children (five females and two males) who were hospitalized with impression of cavitary pulmonary TB were identified. The mean age of the patients was 13.7 (13 - 14 years). Their characteristics are listed in Table 1. Three patients were Iranian and four were Afghan. All patients were symptomatic at the time of admission. The symptoms included cough in 7 patients, fever in 6 patients, weight loss in 6 patients, night sweats in 4 patients, and dyspnea in 1 patient. Examination of lung revealed crackle in 3 patients, wheezing in 1 patient and decreased sound in 2 patients. Only one patient had a close contact with a case of TB (case 7) who previously received chemoprophylaxis with isoniazid.
| Case | Sex | Age, y | Race | Clinical Features | Sputum Smear +/-AFB | Sputum Culture |
|---|---|---|---|---|---|---|
| 1 | M | 13 | Afghan | Cough, fever, weight loss, night sweats | +3 | +3 |
| 2 | F | 14 | Afghan | Cough, fever, weight loss | +3 | +3 |
| 3 | F | 13 | Afghan | Cough, fever, night sweats, weight loss | +3 | NA |
| 4 | M | 14 | Afghan | Cough, fever | +3 | +4 |
| 5 | F | 14 | Iranian | Cough, fever, night sweats, weight loss, dyspnea | + 3 | +3 |
| 6 | F | 14 | Iranian | Cough, fever, weight loss, night sweats | +2 | +4 |
| 7 | F | 14 | Iranian | Cough, weight loss | +3 | +3 |
Abbreviations: AFB, acid-fast bacilli; F, female; M, male; NA, not available.
Complete blood count showed leukocytosis in two patients (cases 1 and 4). The mean value of ESR was 81 mm/hour. The HIV testing was performed in two patients, which was nonreactive. The tuberculin skin test was registered in six patients with positive results in 4 patients (cases 1, 2, 3, and 7). All 7 patients had positive sputum smear results. Positive cultures for M.TB were seen in 6 patients (Table 1). Radiological findings of the patients including chest X-Ray and chest CT are shown in Tables 2 and 3, respectively.
| Case | Consolidation | Cavitary | Cavitary Consolidation | Infiltration | Loss Volume | Plural Effusion | Hydropneumothorax |
|---|---|---|---|---|---|---|---|
| 1 | LUL | NA | NA | NA | NA | NA | NA |
| 2 | NA | NA | RUL/LUL/LLL | RUL/RML/RLL | Left side | NA | NA |
| 3 | NA | NA | RUL | NA | NA | NA | NA |
| 4 | LUL | LUL/RUL | NA | RUL/LUL | NA | NA | NA |
| 5 | LLL/RLL | NA | RUL | NA | Left side | NA | |
| 6 | NA | RLL | NA | LUL | NA | NA | Right side |
| 7 | NA | RUL/LUL | NA | LUL | NA | NA | NA |
Abbreviations: LLL, left lower lobe; LUL, left upper lobe; NA, not availanle; RLL, right lower lobe; RML, right middle lobe; RUL, right upper lobe.
| Case | Consolidation | Cavitary | Multiple Cavities | Cavitary Consolidation | Infiltration | Bronchiectasis | Loss volume | Plural Effusion | Hydro Pneumothorax | Calcified Node | Pleural Thickening |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | RUL/RML/RLL/LLL | LUL | RUL | NA | RUL/RML/RLL/LLL | RUL/RML/RLL/LLL | NA | NA | NA | NA | NA |
| 2 | NA | NA | NA | RUL/LUL/ LLL | LLL/RML/RLL | RML | Left side | NA | NA | NA | NA |
| 3 | RLL | RUL/LUL | NA | NA | RUL/LLL | RUL/LLL | NA | NA | NA | Mediastinal/hilar | NA |
| 4 | LUL | LUL/RUL | NA | NA | RUL/LUL | NA | NA | NA | NA | NA | NA |
| 5 | LLL/LUL | NA | NA | RUL/RLL | RUL/RLL | NA | NA | Both sides | NA | NA | NA |
| 6 | RLL/RML | RLL | NA | NA | LUL/RML | NA | NA | NA | Right side | NA | Right side |
| 7 | NA | NA | RUL/LUL/LLL | NA | Both lungs | NA | NA | NA | NA | NA | NA |
Abbreviations: LLL, left lower lobe; LUL, left upper lobe; NA, not availanle; RLL, right lower lobe; RML, right middle lobe; RUL, right upper lobe.
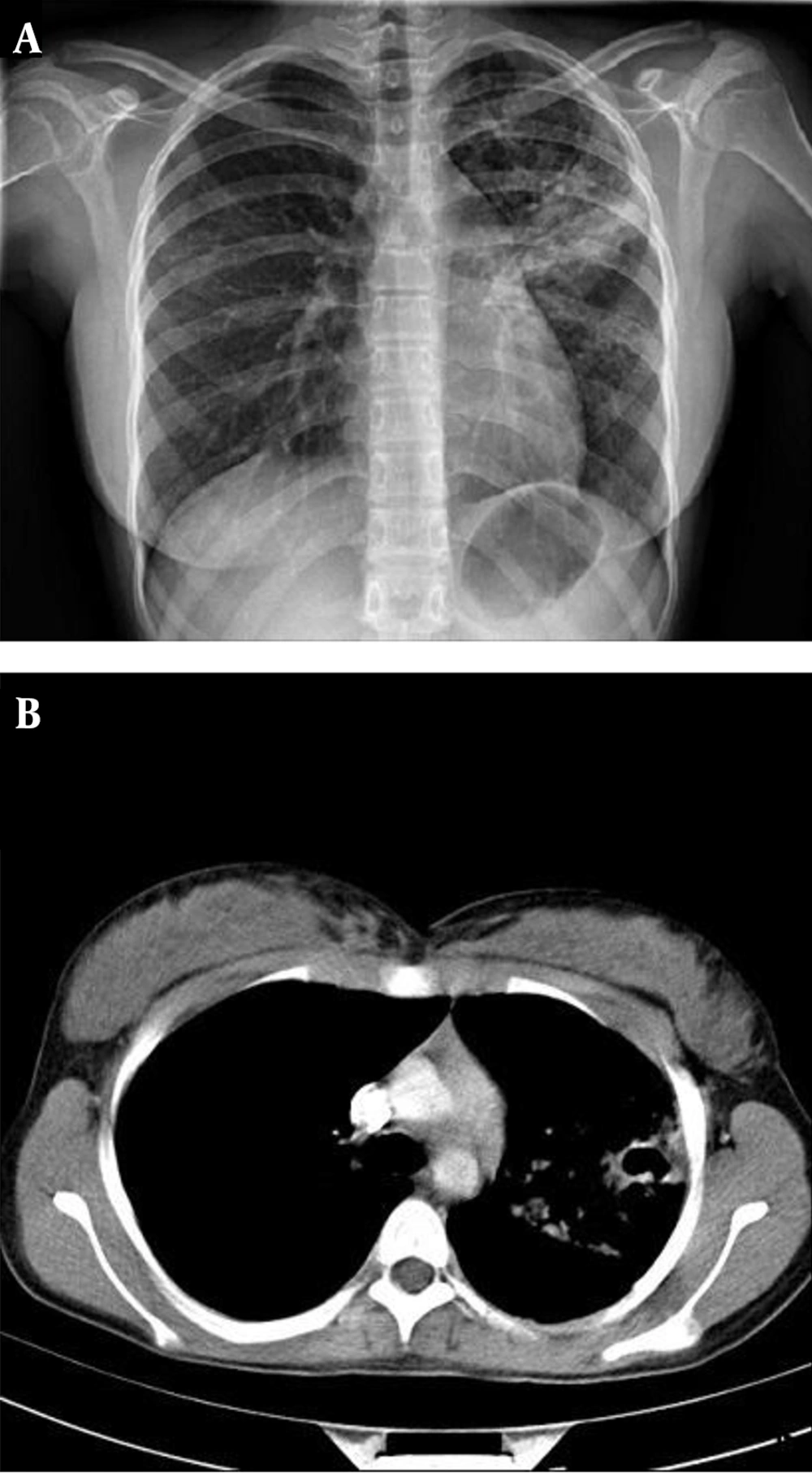
Treatment in all patients was started with the standard isoniazid (INH) and rifampin (RP) program for six months. During the first two months, pyrazinamide (PA) and ethambutol (EB) were also prescribed in all 7 patients. Treatment in six patients was completed during six months, who were finally cured. In case 1, sputum AFB was still positive after five months who was confirmed as a failure case. Drug susceptibility test was performed and resistance to RP and INH were recognized. The patient was received EB, PA, ciprofloxacin and protionamide that responded very well (Figures 1 and 2).
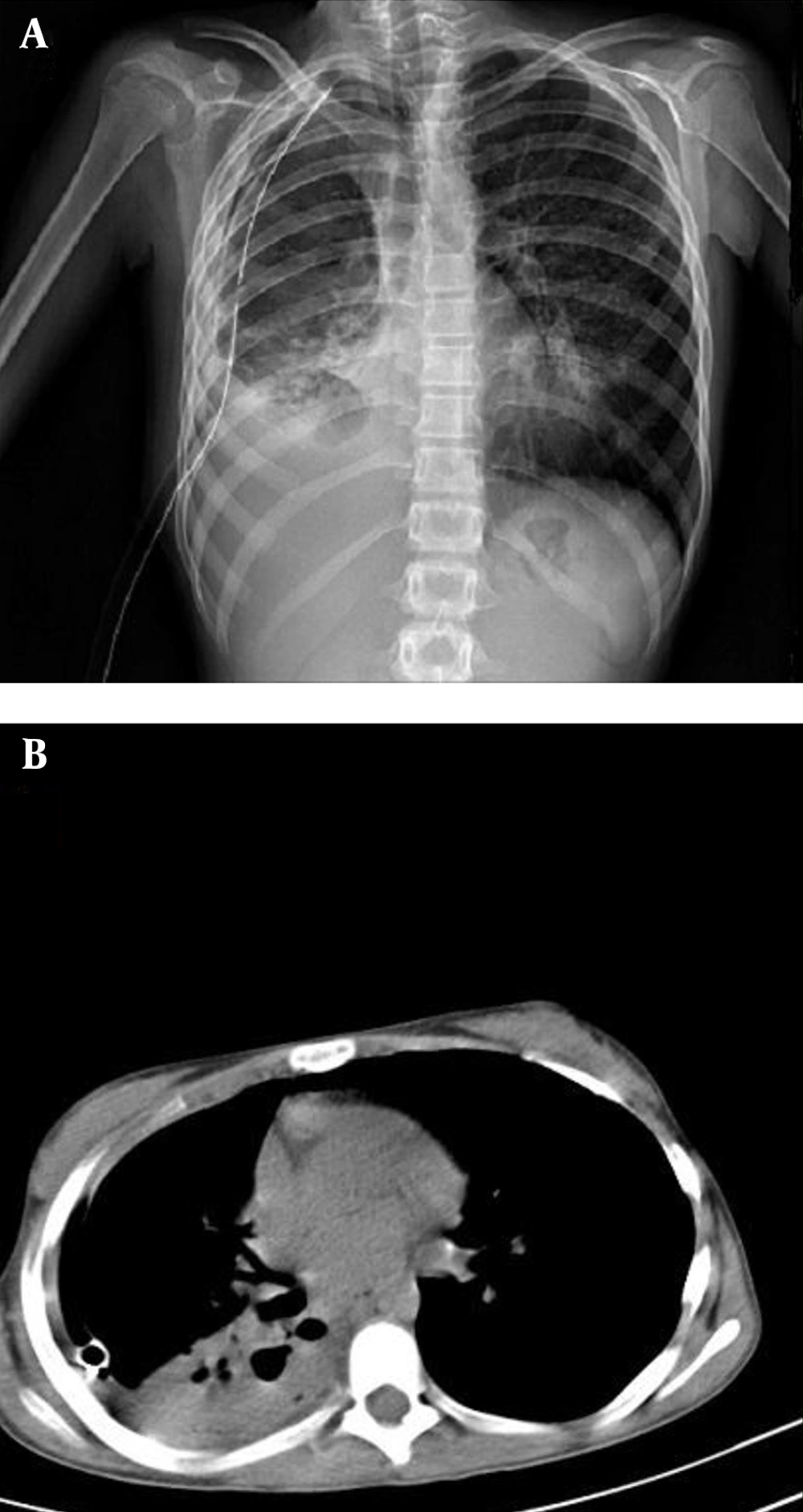
A, Chest radiograph shows cavitary consolidation in the right lower lobe, consolidation in the right middle lobe and hydropneumothorax; B, CT scans demonstrate cavitary consolidation in the right lower lobe, hydropneumothorax, plural thickening and chest tube placed in the right hemi thorax.
5. Discussion
Cavitary pulmonary TB appeared to be more common in females and children 13 - 14 years old in this report. Predominant site of this disease was the upper lobe of the right lung. All patients had positive sputum smear results.
It has been revealed that sudden changes occur in the nature of TB at the beginning of puberty. Adult type pulmonary TB which is characterized by cavitation that leads to sputum smear positivity and more infection spread is seen from this age onward (8) All seven patients of our study were 13 - 14 years old and five of them were female. In a recent study of pulmonary TB in adolescents in Brazil, it was detected that there was a slight predominance of cavitary pulmonary TB in adolescent females compared with adolescent males although the difference was not statistically significant (9). It has been shown that cavitary pulmonary TB is more frequently seen in females than males between the ages of 14 - 17 years (8).
Adolescents and older children can develop typical adult type reactivation TB. They are more likely to exhibit the typical symptoms of anorexia, fever, productive cough, weight loss, night sweats, and hemoptysis than younger children (10-12). In our study, all patients were symptomatic that their common symptoms were coughs, fever, and weight loss.
Cavitation is the hallmark radiographic feature in postprimary TB, which results from reactivation of an inactive focus of pulmonary TB (13). Chest CT findings in adult patients with active pulmonary TB are related to the number of AFB on the sputum smear. The frequency of cavitation on chest CT increases with the number of AFB on the sputum smear in adult patients with active pulmonary TB (14, 15). In our study, all patients had sputum smear positivity more than 2+ AFB. Nevertheless, no study has examined their correlation in children with pulmonary TB. In all of our patients, the cavitary lesion occurred frequently in the right lung. The upper lobes were involved in six patients. Shewchuk and Reed demonstrated that 100% of the children had cavitation in the upper lobes, while the right lung was involved in 80% of the cases (16). Isolated cavitary pulmonary TB of the lower lobe is rare while involvement of lower lobe along with upper lobe cavitation is not a rare finding (16). In agreement with these findings, we found that three patients had lower lobe cavitation in the presence of upper lobe cavitation while only one patient had cavitation in the isolated lower lobe.
The evidence of previous primary pulmonary TB includes calcified mediastinal or hilar lymph nodes, pleural thickening or calcification, calcified parenchymal foci, reticular scars, and volume loss. Shewchuk and Reed reported these findings on radiography in five of six patients with postprimary disease (16). The evidence of previous primary pulmonary TB was present in 3 patients (cases 2, 3 and 6) in this study. Multiple cavities suggest an underlying immune compromised condition or the possibility of multidrug resistant tuberculosis (MDR-TB) (14, 15). We found two patients with multiple cavities, one of them had MDR-TB who was afghan immigrant and the other one received pervious TB chemoprophylaxis. The emergence and spread of MDR-TB can be linked to the increasing amount of international travel, migration and lost to follow-up after starting treatment (17, 18). Failure to recognize children in contact with infectious adult MDR pulmonary TB may lead to the delayed diagnosis of MDR- TB and progression of the disease.
In conclusion, children with cavitary pulmonary TB were older and more likely to have sputum smear positivity. These patients are highly infectious; therefore, the TB control programs should pay more attention to prevention and treatment of TB in older children especially females. Prompt detection and treatment can reduce the transmission of TB in the community.
.jpg)