1. Introduction
Hepatitis A virus is one of the leading causes of acute viral hepatitis in India but usually manifests as a mild self-limiting illness. The most dreaded complication of Hepatitis A infection is acute fulminant hepatic failure with or without encephalopathy (1). Secondary or reactive hemophagocytic lymphohistiocytosis (HLH) has been reported as a rare complication of acute hepatitis A virus infection (2, 3). Acquired HLH can occur secondarily to either infection or rheumatological diseases or haematological malignancy. Infection associated HLH (IAHLH), the commonest of all of these secondary outcomes, can be triggered by any type of infection, although viruses like Epstein–Barr virus (EBV) are most commonly associated. In case of IAHLH, if any underlying treatable cause is found, adequate treatment may be sufficient to control the hypercytokinemia (4). However, most IAHLH need Immunosuprressive therapy in the form of steroids, immunoglobulin, cyclosporine and etoposide depending upon the severity. Here we report a case of IAHLH secondary to hepatitis A virus infection that was treated successfully with a short course of steroids and showed improvement.
2. Case Presentation
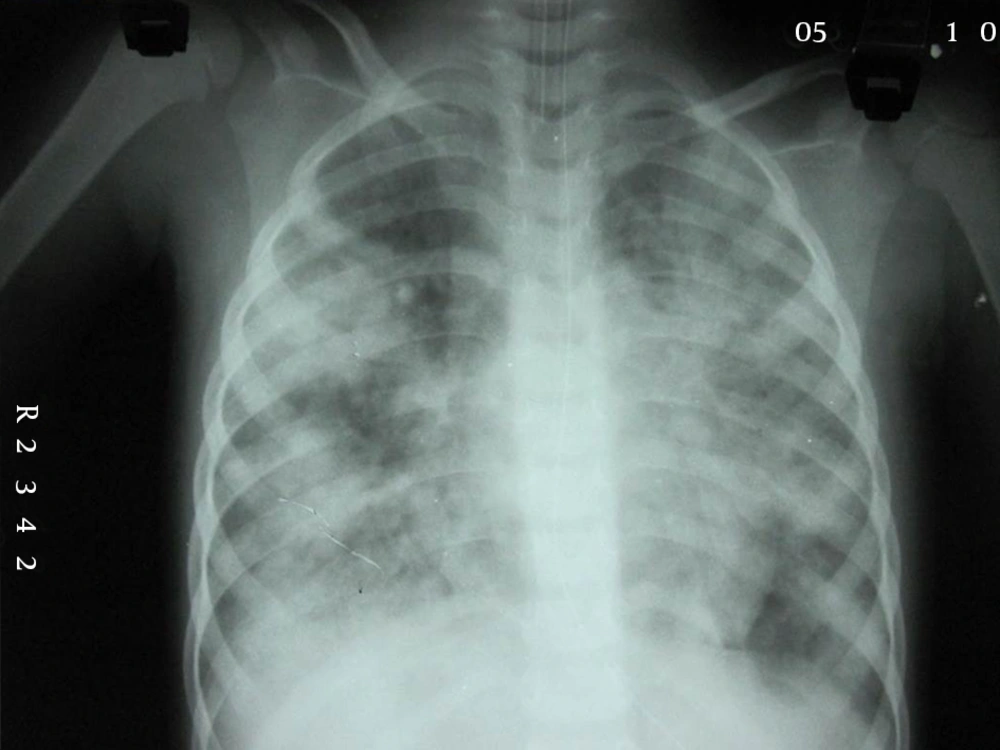
A five-year-old girl was admitted to the hospital with intermittent fever for 15 days, yellowish discoloration of the skin, sclera and urine for three days, gum bleeding, melena and hematochezia for three days and altered sensorium for one day. On admission, the girl was stuporous and had the following characteristics; Glasgow comma scale (GCS)-11/15, febrile, heart rate (HR)-157/min and blood pressure (BP)-90/60. She was pale and icteric and there was a 6 cm hepatomegaly and 3 cm splenomegaly. Plantar was extensor on both sides and deep tendon reflexes were brisk. Initial reports showed hemoglobin (Hb)-5.9 gm%, total leucocyte count-12200/cmm, differential leucocyte count was; neutrophil 75%, lymphocytes 21%, eosinophills 2%, monocyte 2%, platelet-180000/cmm, erythrocyte sedimentation rate (ESR) 36 mm in the 1st hour, C-reactive protein (CRP) 18 mg/L, normal renal function test (RFT), deranged liver function test (LFT) [Bil (T)-8.36 mg/dL, Bil (D)-4.9, Bil (ID)-3.4, serum glutamic oxaloacetic transaminase (SGOT)-3467IU/dL, serum glutamic-pyruvic transaminase (SGPT)-1203 IU/dL, Alk Phos-277, Ptime-40 seconds]. Tests for malarial antigen, HBsAg and widal test were negative. Anti-hepatitis A virus (HAV) IgM was strongly reactive. Initial blood and urine culture were negative. She was shifted to our pediatric intensive care unit and was managed conservatively in the line of acute hepatic failure with iv fluids, vitamin K, antibiotics, N acetyl cysteine infusion and blood product transfusion. She showed improvement in both clinical and laboratory parameters within 48 hours. Fever subsided, prothrombin time/international normalized ratio (INR) improved, liver enzymes decreased and sensorium also improved. However, the patient started developing an erythematous maculopapular rash with a few purpuric spots, first seen on the cubital fossa on the third day of admission, which later spread to the trunk and perineum, and became more confluent over the limbs (Figure 1). Fever reappeared and sensorium deteriorated again. She also developed pallor, edema, abdominal distension, respiratory distress, increased bleeding tendency, deepening of the jaundice and developed type 1 respiratory failure for which she was intubated and ventilated. Chest X ray was suggestive of acute respiratory distress syndrome (ARDS) (Figure 2). Repeat investigations revealed total leucocyte count(TLC)-4,600/cmm, Differential leucocyte count DLC-N12, L78, M6, E4 (ANC 552), ESR-8 mm/1st hour, CRP-123 mg/L (normal < 6), Platelet-12000/cmm, PT-56 seconds (control 12 seconds), activated partial thromboplastin time (APTT)-84 seconds (control 28 seconds), bilirubin-18.2 mg/dL and SGPT-3342 IU/dL.
Since there was a relapse of fever and unusual late deterioration along with persistent splenomegaly, multisystem involvement, development of cytopenia and coagulopathy and further rise in bilirubin and liver enzymes, possibility of secondary HLH was considered. Relevant investigations were performed, which revealed ferritin 2490 ng/dL, lactate dehydrogenase (LDH)-1886, triglyceride-486 mg/dL, fibrin degradation products FDP > 10000 and fibrinogen-76 g/L. Bone marrow examination revealed plenty of hemophagocytes and confirmed our clinical suspicion. The patient was initiated on iv dexamethasone (10 mg/m2) with broad spectrum antibiotics and blood products transfusion. She started improving rapidly, was extubated on the fifth day of mechanical ventilation, LFT and P Time became near normal on the seventh day of steroid administration and no further immune suppression was needed. In view of the underlying liver disorder, dexamethasone was given for a shorter duration and tapered off within 1 month. The patient has been doing well without any relapse of HLH or further deterioration in liver function.
3. Discussion
Hemophagocytic lymphohistiocytosis (HLH) occurs due to uncontrolled proliferation and activation of macrophages, cytotoxic T cells and antigen presenting cells resulting in a state of hypercytokinemia that is responsible for the protean manifestations of the disease characterized by prolonged fever, hepatosplenomegaly, cytopenia and raised serum ferritin level (4). It can be familial or secondary to diseases like infection, autoimmune or rheumatological disease and malignancy. Viruses are the most common triggering agents for infection associated HLH (IAHLH) and this disease is sometimes termed as virus associated hemophagocytic syndrome (VAHS) (5). Many viruses are implicated in the etiology of VAHS, among them EBV is the commonest. Others include adenoviruses and cytomegaloviruses, etc. Hepatitis A virus is amongst the rare causes of infection associated HLH (2, 3). Whatever the etiological agent, all of them usually result in similar presentations, yet in IAHLH due to hepatitis A, the patient obviously presents with jaundice, as in our index case. Prolonged fever unresponsive to broad-spectrum antibiotics and hepatosplenomegaly are the commonest presenting features. Sometimes, it may be associated with different types of rashes as in this case where a generalized maculopapular rash was seen. IAHLH may be further complicated by multisystem involvement. Central nervous system involvement and coagulopathy are the commonest and carry a poor prognosis (6). Very rarely, respiratory involvement can occur in the form of ARDS as in this case, where the patient developed ARDS and needed ventilation (7). Hepatitis A is a rare cause of IAHLH. In the pediatric population HAV associated with HLH has been reported in only a few case reports. There are two case reports from Japan, where the patients recovered spontaneously without any specific treatment (8). Further literature search revealed two case reports of HLH from Turkey who responded to IVIg (9). There are also case reports from Brazil, England and Taiwan (10). There are reports of two cases of HAV associated with HLH from CMC Vellore, India (11). Both these patients were treated with dexamethasone and cyclosporine as per the HLH 2004 protocol. Our patient did not receive cyclosporine or IV Ig and actually responded well to dexamethsone only. Though HLH 2004 protocol recommends a combination chemotherapy consisting of dexamethasone, cyclosporine and etoposide, many patients with IAHLH can be managed with less intensive therapy and even with steroids alone (12). Although extremely rare, physicians should be aware of uncommon manifestations and complications like HLH, in a relatively common infection like hepatitis A, as early diagnosis and treatment are potentially curative in this life threatening disorder.