1. Introduction
Bacillus Calmette-Guérin (BCG) vaccine, derived from a live attenuated strain of Mycobacterium bovis, is administrated to all newborn infants in endemic regions according to the current World Health Organization (WHO) recommendation (1). In contrast to tuberculosis (TB) dactylitis (also known as spina ventosa) which is one of the known musculoskeletal manifestations of tuberculosis infection (2, 3) BCG dactylitis is an extremely rare consequence of disseminated BCG infection (4, 5). In our country, BCG vaccine is administrated to all newborn infants but due to lack of careful history taking and routine screening program, immunologist and pediatricians frequently encounter with complications of this vaccine in infants who later identified as having primary immunodeficiency disorders (PID). These unfavorable events are severe and have high mortality rates.
2. Case Presentation
A ten-month-boy admitted in our hospital with multiple fusiform painful swelling in his hands. He was a known case of SCID who had received bone marrow transplantation about 7 weeks before admission. In his past history, left subaxillary lymphadenitis was detected 4.5 months after birth and started to progress ever since. In the primary referral medical visit, he did not receive any medication or investigation. After a few weeks, subaxillary adenitis enlarged and fistulated. At that time, further examination and immune status work up performed and diagnosis of SCID was made (T cell and B cell negative type). Before transplantation, serologic tests for common viruses, HIV and hepatotropic viruses had been carried out (data summarized in Table 1). Anti-tuberculosis treatment started with the possible diagnoses of systemic BCG disease. The patient got candidate to receive bone marrow transplantation (BMT) from her full matched sister without conditioning or prophylaxis requirement.
Allogeneic BMT had done with white blood cell (WBC) = 12.18 × 108, mononuclear cell (MNC) = 8.1 × 108, CD34 = 1.51 × 106, and CD3 = 3.1 × 106 in 50 mm volume. Booster dose infusion was administrated two months later because of low and suboptimal chimerism (WBC = 24.18 × 108, MNC = 16.1 × 108). The patient had been hospitalized in transplantation ward for 71 days.
| Virus Marker | Result | Comment |
|---|---|---|
| HBS Ag | negative | |
| Anti-CMV Antibody | ||
| IgG | 29 | reactive |
| IgM | 3 | non-reactive |
| Anti-HSV 1/2 Antibody | ||
| IgG | 129 | reactive |
| IgM | 0.1 | non-reactive |
| Anti-HAV Antibody | ||
| IgM | - | non-reactive |
| Anti-HCV Antibody | ||
| IgM | - | non-reactive |
| Anti-EBV Antibody (VCA) | ||
| IgG | 24 | reactive |
| IgM | 1 | non-reactive |
| Anti-VZV Antibody | ||
| IgG | 46 | reactive |
| IgM | 2 | non-reactive |
| HIV PCR | - | negative |
aAbbreviations: HBS, hepatitis B virus; IgG, Immunoglobulin G; IgM, Immunoglobulin M; CMV, cytomegalovirus; EBV, Epstein-Barr virus; HAV, hepatitis A virus; HBV: hepatitis B virus; HCV, hepatitis C virus; HSV: herpes simplex virus; VZV, varicella zoster virus; HIV, human immunodeficiency virus.
Anti-tuberculosis treatment had discontinued after BMT, and the patient had begun to receive acyclovir and co-trimoxazole prophylaxis. After a few weeks, subaxillary adenitis reappeared, and new fusiform painful swelling in his hands and then feet developed. Anti-tuberculosis treatment started again, which was led to hepatic toxicity along with the rise in liver enzymes and bilirubin. At this time, isoniazid and rifampin discontinued and infectious diseases consultation was requested and patient referred to our hospital for drug adjustment and further management of his complications. He was monitored weekly for liver function and CMV PP65 antigen (with negative results in several checks) (Table 2). No specific work up for detection of BCG was done in the transplant center.
| At Admission | 4 Days After Admission | 7 Weeks Later in Follow up | |
|---|---|---|---|
| WBC | 14000 | 21400 | 8000 |
| N | 70 | 82 | 60 |
| L | 26 | 14 | 36 |
| Hb | 10.8 | 10.2 | 15.7 |
| Plt | 201 × 103 | 147 × 103 | 199 × 103 |
| ESR | 18 | 8 | - |
| PT | 15 | 15 | 14.5 |
| PTT | 53 | 60 | 35 |
| INR | 1.3 | 1.5 | 1.29 |
| Bil total | 8.1 | 7.3 | 4.15 |
| Bil direct | 4.7 | 3.9 | 3.15 |
| ALT | 20 | 21 | 2 |
| AST | 56 | 60 | 42 |
| ALKP | 863 | 854 | 303 |
| CRP | 52 | - | - |
| CMV Ag | negative | negative | negative |
aAbbreviations: N, neutrophil; L, lymphocyte; Hb, hemoglobin; Plt, platelet; ESR, erythrocyte sedimentation rate; CRP, C-reactive protein; PT, prothrombin time; PTT, Partial Thromboplastin Time; INR, International normalized ratio; Bil, Bilirubin; ALT, Alanine transaminase; AST, Aspartate aminotransferase; CMV Ag, cytomegalovirus antigenemia.
Upon admission, the patient was ill, had scleral icterus and seemed icteric in his trunk too. In abdominal exam ascites and hepatosplenomegaly were found. In extremities, he had several fusiform swelling at interdigital space of his hands which resulted in abscess formation of some of them. Soft-tissue mass like lesions were detected in dorsal aspect of his feet; these lesions were intact without fistula formation or ulceration (Figure 1). In left subaxillary space, he had large ulcerative and fistulated adenitis. The rest of the physical examination was normal.
Blood culture with the BACTEC system was negative upon admission. His prolonged PTT and INR corrected with fresh frozen plasma, and he was planned for surgical debridement of axillary adenitis and dactylitis. After FFP infusion and INR correction, CSF sampling was done which revealed acellular CSF and negative culture. No microorganism was seen in direct cerebrospinal fluid (CSF) smear examination. Ultrasonography showed moderate to severe free fluid in abdominopelvic cavity. Therapeutic and diagnostic ascetic fluid tap were done, which revealed WBC = 0, RBC = 2400, protein = 480, and glucose = 100. Ascitic fluid culture was negative after one week. CSF and ascitic fluid were sent for TB-polymerase chain reaction (PCR), smear and culture, which were negative.
Because of other signs than ascites, such as hepatomegaly, visible venous pattern on the chest, abnormal liver enzyme test, γ-GT increase, low albumin, generalize edema and mixed hyperbillirubinemia, work up was performed for underling liver disease. In color Doppler sonography, no evidence of hepatic veno-occlusive disease was found. Ursodeoxycholic acid and spironolactone started after gastroenterologist consult and patients received albumin infusion for several times.
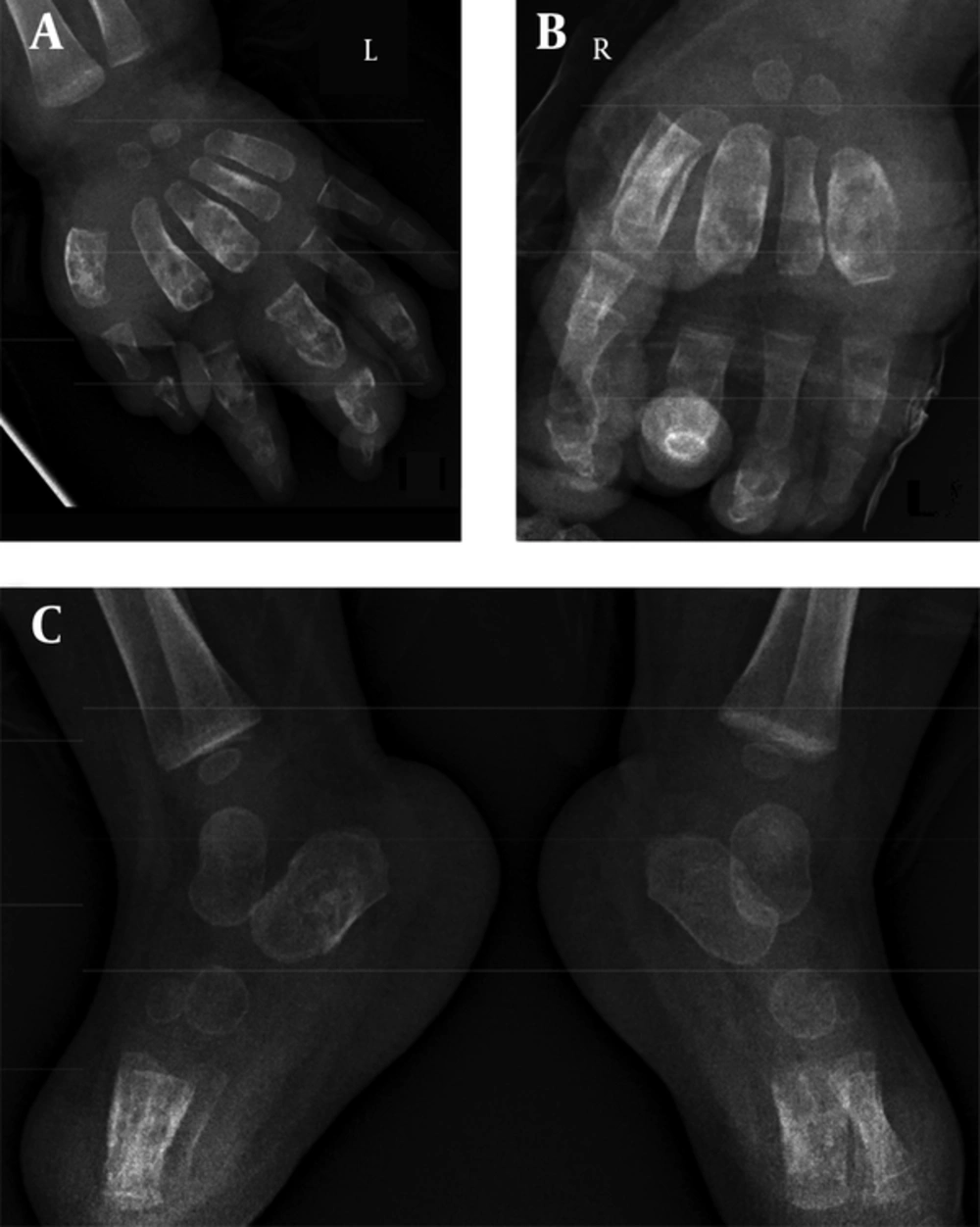
No active infiltrations in lung fields were reported in chest X-ray, cardio thoracic ratio was in normal range, costophrenic angles are clear and soft tissue and bone densities of the thorax are unremarkable. Bone survey was done and revealed several lytic bone lesions with expansion in his hands (in left and first), second and third metacarpal bones and also second, third and fourth proximal and middle phalanges. Third and fourth metacarpal bones and third and fourth proximal phalanges were also shown similar bony involvements in the right side. Lucency in distal radius was also seen (Figure 2).
No sclerotic lesion, fracture or dislocation was seen. In further investigation, the following findings were revealed: increase in blood urea nitrogen (BUN), serum creatinine, liver function tests and prolonged PTT, PT, and INR. He was complicated with ascites (Adenosine deaminase = 10 [cut-off values from 36 to 40 IU/L; optimal cut-off point was determined at 39 IU/L] (6); PCR-TB [BCG], acid-fast bacilli (AFB) and TB-culture were negative) and pancytopenia (Table 2). After primary work up, anti-tuberculosis therapy (with isoniazid, rifampin, ethambutol, clofazimine, ofloxacin and Vitamin B6) started. Surgical and orthopedic consult were also requested. Surgical debridement of dactylitis was performed in his both hands.
In the second step, patient was planned for surgical drainage of subaxillary abscess and soft-tissue masses in dorsalis pedis area. Recurrent swelling of the surgical site happened after a week, and the patient underwent repeated drainage. Drainage materials were sent to the National Research Institute of Tuberculosis and Lung Disease (NRITLD) for Mycobacterium tuberculosis and BCG PCR along with aerobic and anaerobic culture and specific staining for fungal pathogens.
Mycology culture and direct smear were negative for fungi. Drainage materials of both hands were reported positive for BCG-PCR. Biopsy specimen of lesions was also positive for BCG-PCR. According to the identification of Mycobacterium bovis, BCG substrain, from the patient’s bone involvement by culture and standard PCR, as well as typical histopathologic changes with granulomatous inflammation, in addition to systemic symptoms and more than 2 areas of involvement beyond the site of BCG vaccination (hepatosplenomegaly and bone involvement) our patient fulfilled all diagnostic criteria of disseminated BCG infection (7, 8).
Because of time elapsed since bone marrow transplantation, our patient was put in post engraftment period; however, based on hyperbillirubinemia, ascites, hypoalbuminemia, pitting edema and other clinical signs of liver failure (visible venous pattern on abdomen and hepatomegaly), we consider other differential diagnosis such as hepatic veno-occlusive disease and GVHD for our patients. No evidence of any hepatic veno-occlusive disease was found in prehepatic or posthepatic venous system by Doppler ultrasonography. Flow cytometric investigation revealed 30% chimerism, thus occurrence of acute GVHD was less likely in this situation (serial flow cytometric are summarized in Table 3). Because of the patient’s general condition and presence of ascites, liver biopsy was not performed.
| Markers | 2 Weeks Before BMT | 3 Months After BMT | 5 months After BMT | ||||
|---|---|---|---|---|---|---|---|
| % | Gated | % | Gated | % | Gated | Gate | |
| CD2 | 2.3 | 31 | 6 | 23 | 10 | 40 | lymphocyte |
| CD3 | negative | 2 | 7 | 25 | 10 | 40 | lymphocyte |
| CD4 | 0.2 | 2 | 4 | 11 | 3 | 11 | lymphocyte |
| CD7 | - | - | 17 | 58 | - | - | lymphocyte |
| CD8 | 0.6 | 8.7 | 7 | 25 | 6 | 22 | lymphocyte |
| CD19 | negative | negative | 0.2 | 0.4 | 1 | 2 | lymphocyte |
| CD20 | negative | negative | 0.2 | 0.4 | 1 | 2 | lymphocyte |
| CD16 | 73 | 12 | 76 | 60 | 42 | 10 | lymphocyte |
| CD56 | 3 | 40 | 13 | 60 | 6 | 19 | lymphocyte |
| CD34 | - | - | negative | negative | - | - | lymphocyte |
| HLA-DR | - | - | 23 | 16 | - | - | lymphocyte |
| CD2/CD56 | 31% of total | - | - | - | - | - | lymphocyte |
| CD4/CD8 | 0.33 | - | - | - | - | - | lymphocyte |
aAbbreviations: CD, cluster of differentiation; BMT, bone marrow transplantation
3. Discussion
Our patient’s clinical presentation has a unique picture of systemic BCG disease, which involves multifocal dactylitis in his both hands, axillary adenitis and soft tissue swelling over the dorsum of feet without any overlying skin changes along with diffuse bony involvement in hands and feet. This presentation was rarely reported in the literature (4, 5). Kekulawala et al. from Sri Lanka described a case of disseminated BCG in a ten-week-old boy infant with disseminated TB following BCG vaccination, possibly due to faulty techniques of intradermal administration and use of excess doses of the vaccine. Unfortunately, he had not presented his patient’s bone survey, and also he had not been succeeded to attain BCG from bone erosion and dactylitis drainage. Primary immunologic workup for primary and secondary immunodeficiency had negative results (4).
In a more recent report, Khan et al. reported a diffuse osteomyelitis secondary to BCG vaccination in a 4-month-old boy with possible severe combined immunodeficiency manifested with swollen, tender limbs and hepatosplenomegaly accompanied with pancytopenia. Diffuse bony involvement consisted of multiple lytic lesions in the metaphysis of the long bones and diffuse soft-tissue sewelling (5).
Complications following BCG vaccination are frequently being encountered. These complications include “regional disease”, “extra-regional localized disease” and “disseminated disease” (7). Among these complications, disseminated BCG infection is the most serious with the lowest incidence ranged from 0.06 to 1.56 cases per million vaccinated, and with a high mortality rate (7, 9, 10).
Disseminated BCG in an immunodeficient child may be the presenting clinical picture of a PID. There are over 100 different primary genetic immunodeficiencies that predispose the patients to infections with a variety of viruses, bacteria, fungi and protozoa, but only a few have been associated with severe mycobacterial infections (11). These include severe combined immunodeficiency (SCID), chronic granulomatous disease (CGD), Di George syndrome and homozygous complete or partial interferon-γ deficiency (9, 12, 13). Therefore, when dissemination occurs, an underlying immune deficiency state must be excluded, although it can occur even in normal infants (7).
In patients suffered from SCID, the most important factor in improving the prognosis is to diagnose and treat the disease as soon as possible. Accordingly, bone marrow transplantation advised early after diagnose, but because of early administration of BCG vaccination within days of birth and also because no routine screening test for SCID is currently available, these patients usually suffer from complications of BCG vaccination. Disseminated BCG disease happened before or after receiving bone marrow transplantation would cause complexity in management and poorer outcome. Pediatricians should be familiar to uncommon presentation of BCG vaccination in our country. Of special consideration, patients with SCID need to continue anti-tuberculosis treatment until complete immune reconstitution after hematopoietic stem cell transplantation (HSCT).
We suggest that any decision to revise these regimens made with consultation of infectious specialist in treatment of tuberculosis. Finally, BCG vaccination administrated routinely in Iran and screening for primary immune deficiency is impossible currently in our country (as in many other countries) because of limited recourse and absence of standard practices. Accordingly, avoidance of BCG complication in this setting is impossible, so close attention to reschedule immunization programs (postpone immunization) in suspicious newborn is always necessary and is one of the most effective strategies to prevent BCG fatal complications.