1. Introduction
Congenital broncho-esophageal fistula (BEF) is a rare anomaly of the lower respiratory tract typically appearing and diagnosed in adults (1, 2). In the majority of the reported cases, the anomaly is isolated with no associated diseases (2). BEF occurs equally in men and women. The diagnosis is usually confirmed by barium esophagogram. The treatment approach is surgical and the result of surgery and the patients’ outcome are excellent (1). However, diagnosing a missed BEF in children with congenital esophageal atresia (EA) and trachea-esophageal fistula (TEF) repaired during the neonatal period is a real challenge as medium leakage in the respiratory tract may be missed on standard contrast studies (3, 4) and the patients may present recurrent or persistent respiratory symptoms. This case report highlights the importance of using flexible bronchoscopy for the diagnosis of such conditions.
2. Case Presentation
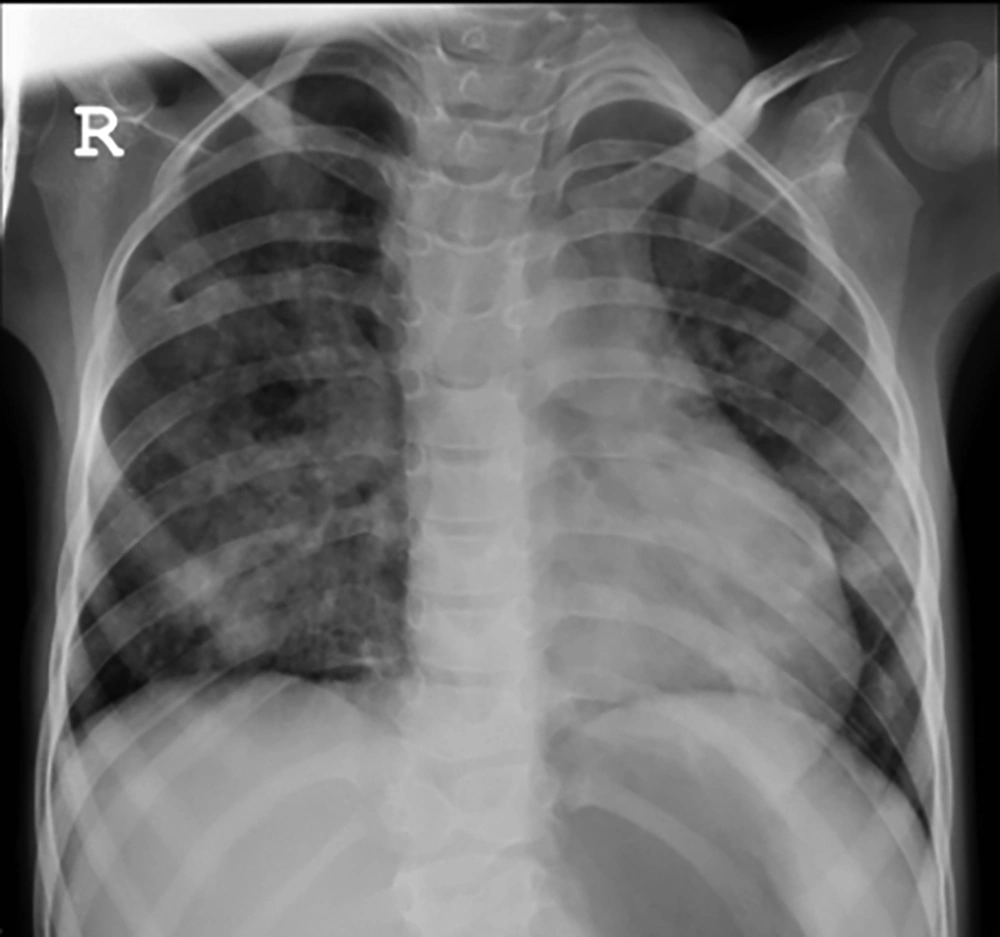
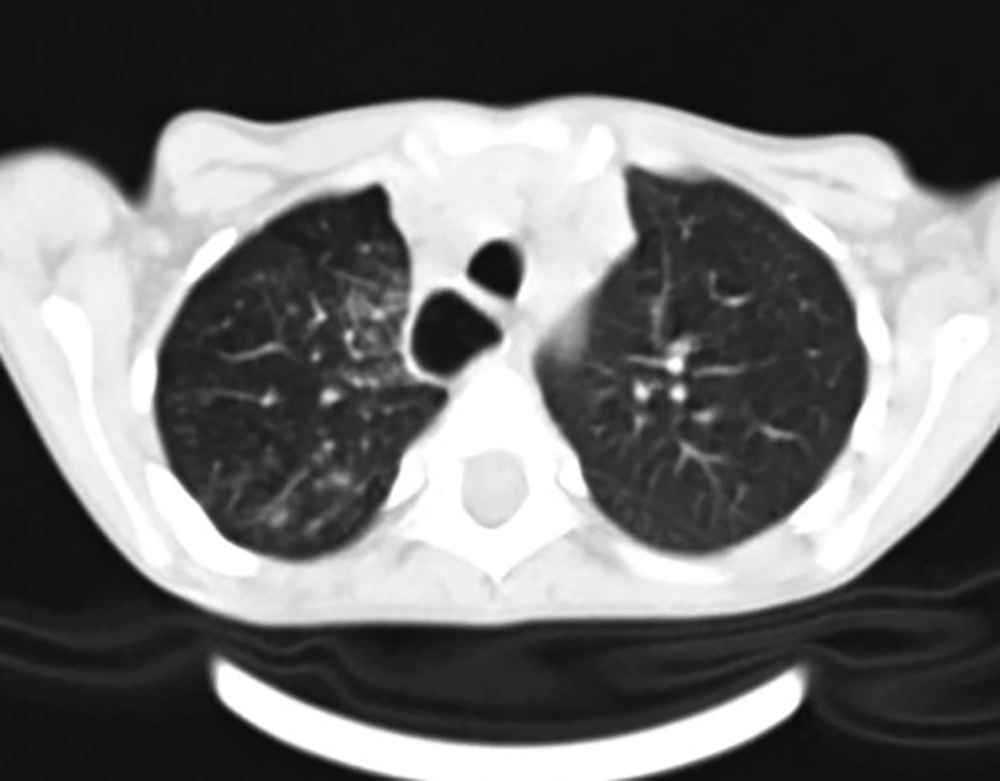
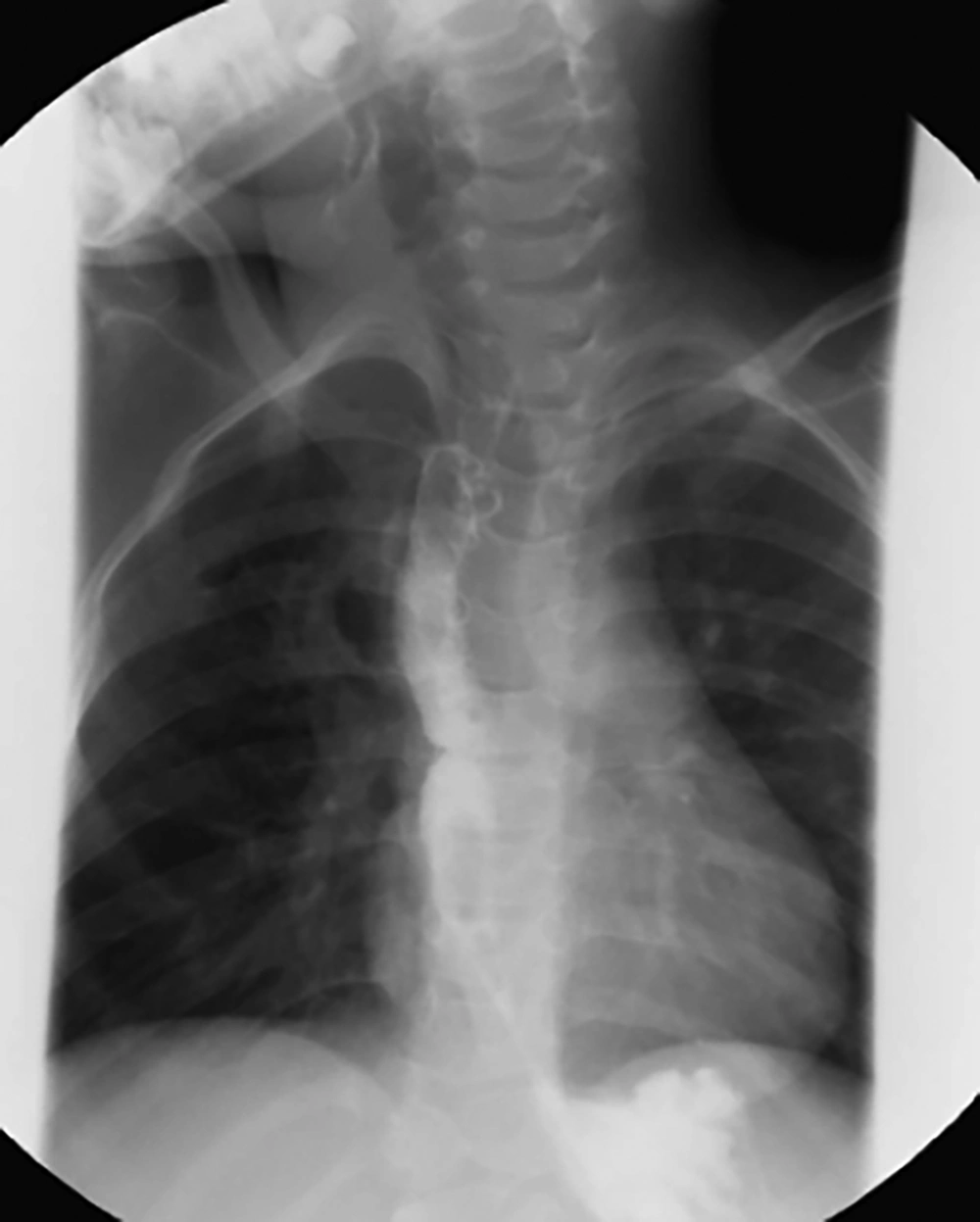
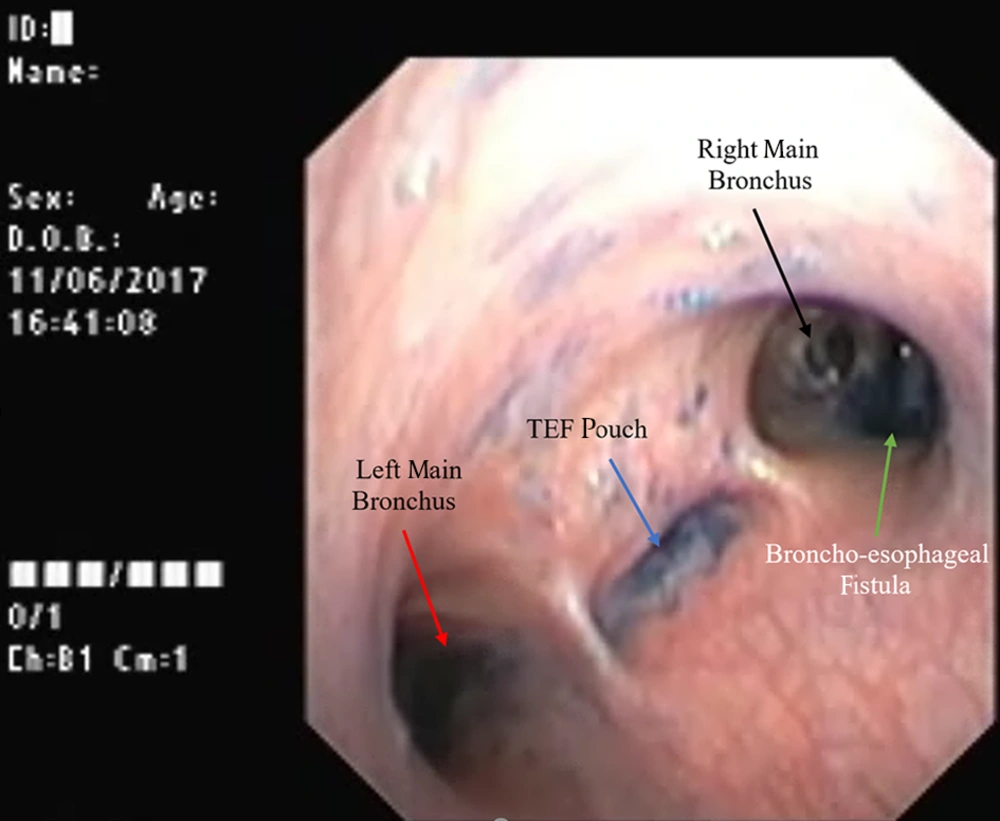
A six-year-old girl referred to a pediatric gastroenterologist at our center for the evaluation of dysphagia to both liquid and solid food, chronic cough, choking, and respiratory distress following eating, resulting in vomiting or regurgitation for three years that was aggravated seven days before admission. She had been diagnosed with congenital EA that was repaired in the neonatal period. Coughs were occurring following drinking water or lying down at night. Gastro-oesophageal reflux disease (GERD) had been suspected. Therefore, pH-metry with impedance had been requested at another center, which demonstrated gastroesophageal reflux. She had been on pantoprazole since then without improvement of symptoms. Therefore, she underwent upper GI endoscopy and balloon dilatation due to severe esophageal strictures. Despite this procedure, there was still no improvement in symptoms. She had several admissions for aspiration pneumonia. On the physical examination, she was noted with emaciation (BMI = 11.1, Z-score = -5.8); she was febrile with increased respiratory rate, as well. Auscultation revealed diffuse fine crackles. Laboratory tests showed mild normochromic normocytic anemia and vitamin D deficiency. Chest X-ray revealed diffuse patchy opacity especially in the right lung, butterfly vertebra in T12, right hemivertebra in T11 that fused to T12, and focal fusion of the fourth and fifth right ribs (Figure 1). A spiral lung CT scan without contrast was requested on the first day of admission at our hospital, disclosing bilateral mild diffuse bronchiectasis and peribronchial thickening prominently in the right lung (Figure 2). Given the importance of clinical signs and symptoms, recurrent TEF was considered in the differential diagnosis. Therefore, contrast swallowing study was requested on the second day of hospitalization (Figure 3). Surprisingly, no leakage of the contrast fluid into a trachea-bronchial tree was seen. The attending physician requested an evaluation by a pediatric pulmonologist. The patient was scheduled for a flexible fiber-optic bronchoscopy that showed a tracheal bronchus and a pouch in the posterior tracheal wall, with no air bubbling during bag valve mask ventilation. As the presence of an abnormal fistula between the trachea-bronchial tree and esophagus was suspected based on clinical symptoms, the methylene blue dye was injected into the esophagus via a catheter while the fiberoptic bronchoscope was adjusted above carina to provide a direct view on tracheal pouch and bronchus. The leakage of the dye was seen from the right main bronchus (Figure 4). Consequently, the presence of broncho-esophageal fistula was confirmed and the patient was operated on the following day.
2.1. Follow-Up
During an eight-month serial close follow-up, the patient had adequate feeding without dysphagia or respiratory symptoms with more than 5 kg increases in weight and 6 cm in height. The physical examination demonstrated the regular activity with normal breathing sound. The abdomen was soft. Table 1 shows continued catch-up growth in the eight-month follow-up visit.
| Admission Time | After Two Months | After Four Months | After Six Months | After Eight Months | |
|---|---|---|---|---|---|
| Weight, kg | 14.200 | 16.500 | 17.00 | 17.400 | 19.400 |
| Height, cm | 113 | 115 | 116 | 117 | 120 |
| BMI | 11.1 | 12.5 | 12.6 | 12.7 | 13.5 |
| Z-score | -5.8 | -2.9 | -2.7 | -2.5 | -1.6 |
3. Discussion
Congenital broncho-esophageal fistula (BEF) is a rare disease (1). It is usually diagnosed in infancy and commonly associated with esophageal atresia. Isolated BEF diagnosis may be delayed until adulthood due to the insidious onset of symptoms (2, 5). According to Brambridge and Keith classification, broncho-esophageal fistulas are divided into four types including type 1 that is defined as a wide diverticulum with a fistula at the tip, type 2 that is a simple fistula, type 3 that is a fistula with a cyst, and type 4 that consists of a fistula with sequestration segment (1). The present case was a missed case of type 2 BEF associated with TEF, EA, and skeletal anomalies diagnosed in childhood. The age of presentation and associated anomalies in the present case were unique compared to previously reported cases (1, 6-8). The clinical signs and symptoms of BEF are nonspecific, including coughing, chronic aspiration pneumonia, and hemoptysis (2). Persistent respiratory symptoms following TEF repair is not an unusual presentation. Up to 50% of children with a history of esophageal atresia and TEF repair have recurrent or persistent respiratory symptoms. This is due to tracheomalacia, hyper airway reactivity, or repeated aspirations as a result of esophageal dysmotility or stricture, gastroesophageal reflux, or relapse of repaired TEF (9). The most common cause of respiratory complications in patients undergoing prior TEF repair is GER (10); however, other factors such as BEF must be considered. The upper gastrointestinal series with thickened water-soluble contrast agent is a sensitive and available diagnostic approach. The traditional pull-back technique in which the distal esophagus is first filled and then the esophageal catheter is pulled up to proximal portion may increase the diagnostic precision of the method (11). However, contrast swallow study may fail to demonstrate the fistulous tract, as observed in the present case. Several reasons can account for this phenomenon. First, the length of the fistula may be short with a small diameter; therefore, the thick contrast material cannot pass through it. Second, since the track may have a sharp, upward angle from the esophagus, the contrast would not pass through the fistula as a result of gravity. Third, an esophageal flap may result in a check valve and close the fistulous track intermittently (8). Bronchoscopy or endoscopy can also recognize the abnormal fistula between the tracheobronchial tree and esophagus. However, the detection of tracheal or bronchial opening in small fistulas can be challenging (12). At our center, the demonstration of the fistula is facilitated by the injection of a small amount of methylene blue into the esophagus and the appearance of leakage via the fistulous tract in the tracheobronchial tree.
3.1. Conclusions
Despite the rarity of broncho-esophageal fistula, one should consider it in newborns or children with unusual and persistent pulmonary symptoms in spite of a normal barium esophagogram or endoscopy. The use of methylene blue test with the aid of bronchoscopy is helpful to detect this rare anomaly in children. Following the timely diagnosis of BEF and appropriate treatment, excellent outcomes are possible.